Trimethylamine N-oxide (TMAO) may play a key mediator role in the relationship between the diet, gut microbiota and cardiovascular diseases, particularly in people with kidney failure.
- TMAO
- trimethylamine N-oxide
- foods
- fish
- meat
- eggs
- dairy
1. Introduction
Trimethylamine N-oxide (TMAO) has been identified as an osmolyte molecule of the fish world [1]. In many marine species, it acts as a protein stabiliser that counteracts the concentration of urea. The oxidised form decomposes into trimethylamine (TMA) which is responsible for the characteristic odour of putrefied fish [2]. The free TMAO from seafood is directly absorbed into the systemic circulation without metabolism by the gastrointestinal microbiome. In humans, the gut microbiota is responsible for the formation of TMA [3]. The metabolic pathway allows the conversion of choline, betaine and carnitine molecules into TMA, whilst a liver enzyme belonging to the flavin-containing monooxygenases (FMO) family is responsible for its conversion into TMAO [4].
In recent years, numerous studies have suggested that high blood TMAO levels might be associated with heart disease, atherosclerosis, diabetes and cancer [5,6][5][6]. Compelling evidence suggests that circulating TMAO may promote atherosclerosis by altering the clearance of cholesterol in the liver, promoting inflammation and oxidation of LDL cholesterol by up-regulation of the macrophage scavenger and foam cell formation [7]. The current literature shows that TMAO may be a major risk factor for cardiovascular disease (CVD), especially in individuals who have already had a cardiovascular event or have a kidney disease [8,9][8][9].
The factors that can influence the plasma concentration of TMAO are different and complex [10]. For instance, TMAO precursors are among the main bacterial products produced by the intestinal microbiota, and it is likely that the microbiota is essential for TMAO metabolism [6].
The correlation between fish intake and TMAO has been demonstrated since the discovery of this molecule. For other foods, there is an extensive conflicting literature. The aim of our review is to evaluate all the studies in the literature to establish which foods are associated with an increase in plasma or urinary TMAO.
2. Search Strategy and Selection Criteria
The present research was conducted and reported based on the PRISMA guidelines. We searched PubMed, Web of Science, EMBASE and Cochrane Central Register of Controlled Trials (CENTRAL) electronic databases using the following keywords as title/abstract fields: (“Trimethylamine N-oxide” OR “TMAO”) AND (“egg” OR “meat” OR “fish” OR “dairy” OR “vegetables” OR “fruit” OR “food”). We researched papers from 1 January 1990 to 1 December 2020. Studies published in languages other than English were not considered.
Figure 1 depicts the flow of the step-by-step process of applying the inclusion and exclusion criteria to generate a final number of studies for analysis in the review. Studies evaluating food intake in correlation with urinary or plasma TMAO were considered. Reviews, letters, comments, animal studies, and abstracts for posters were excluded. Thus, studies that focused on diets, supplements or nutraceutical use were not considered. Studies evaluating only TMAO measurement techniques or biochemical aspects without focusing on food were excluded.
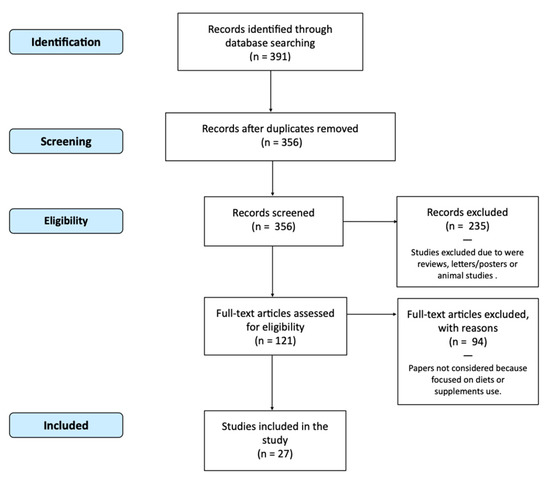
Figure 1. Flow Chart (PRISMA) of Studies Included.
Fish
15 studies evaluated the possible relationship between fish and TMAO. 13 studies demonstrated that levels of urinary or plasma TMAO and/or TMA are significantly associated with the intake of fish [11,12,20,21,24,27,28,30,31,32,33,34,36][11][12][13][14][15][16][17][18][19][20][21][22][23]. One of the earliest studies evaluated 46 different foods and demonstrated that only fish and other sea-products significantly increase urinary TMAO [12]. Cho et al. [21][14] supposed that the rapid rise in circulating TMAO in response to fish consumption might demonstrate that the absorption of intact dietary TMAO is independent of the microbiota. In one paper, the association of fish and shellfish intake with TMAO plasma concentrations was limited to men only [31][19]. Only two papers demonstrated no association. Rohrmann et al. [17][24] revealed that meat, egg or fish consumption is not associated with TMAO, choline or betaine concentrations. Thus, a prospective cohort study showed that dietary intake of fish does not significantly impact the TMAO value in immunodeficient subjects [35][25].
Table 2Table 1 shows the four studies that specifically evaluated the influence on TMA and TMAO of eating different types of fish. TMAO was higher in subjects that eat saltwater fish and shellfish but not freshwater fish [27][16]. These data were confirmed in another study that evidenced higher TMAO values in the group that consumed shellfish and dark meat fish (tuna steak, mackerel, salmon, sardines, bluefish and swordfish) [36][23]. Another paper showed that cod intake has stronger effects on plasma and urine TMAO concentrations than salmon intake [33][21]. One study evaluated cooking methods and demonstrated that TMAO values are strongly associated with deep-fried fish consumption [27][16].
Table 21. Associations of different types of fish intake with TMAO.
| First Author | Year | Study Design | Cod | Farmed Salmon | Halibut | Herring | Mackerel | Sardine | swordfish | Shellfish | Clam | Tuna | Trout | Ref |
|---|
| Zhang AQ # | 1999 | Clinical trial | ↑↑ 5135.3 |
↑↑ 8230.2 |
↑↑ 4345 |
↑ 1424.1 |
↑ 2769.4 |
↑ 1562 |
= 377.1 |
= 301.8 |
= 495.2 |
[12] | ||
| Yu D | 2019 | Case-control multicentre | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | = | [27] |
| Yu D | 2019 | Case-control multicentre | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | ↑↑ * | = | [16] |
| Hagen IV | 2020 | RCT | ↑↑ | ↑ | ||||||||||
| ↑ | ||||||||||||||
| [ | 33 | ] | ||||||||||||
| Hagen IV | 2020 | RCT | ↑↑ | [21] | ||||||||||
| Hamaya R | ||||||||||||||
| Hamaya R | ||||||||||||||
| 2020 | Retrospective | ↑↑ | ↑? | ↑↑ | ↑↑ | ↑↑ | ↑↑ | ↑↑ | ||||||
| 2020 | Retrospective | ↑↑ | ||||||||||||
| ↑? | ||||||||||||||
| [ | 34 | ] | ||||||||||||
| ↑↑ | ↑↑ | ↑↑ | ↑↑ | ↑↑ | [22] |
3. Eggs
17 studies that assessed the correlation between egg consumption and increased TMAO were evaluated. Robust correlations between TMAO and eggs were demonstrated in six studies [13,14,19,25,30,34][26][27][28][29][18][22]. Pignanelli et al. [25][29] described that the intake of egg yolk contributes significantly to plasma levels of TMAO. The phosphatidylcholine in egg yolk, via action of the intestinal microbiome, may be the major contributor to production of TMAO. The increase in TMAO induced by egg consumption has also been related to cardiovascular risk. Tang et al. studied the effects on plasma TMAO after a test dose of two hard-boiled eggs and found that patients in the highest quartile for TMAO had a 2.5-fold increase in the three-year risk of myocardial infarction or stroke [13][26]. In contrast, studies mainly starting from 2014 have assessed little or no effect of egg consumption on TMAO levels [12,15,17,18,21,22,23,27,31,35,37][12][30][24][31][14][32][33][16][19][25][34]. Some of these studies have revealed that plasma choline and betaine increase dose-dependently with egg intake. Many of these studies have been funded by the egg industry [15,18,21,22,23,37][30][31][14][32][33][34].
4. Meat
12 studies [12,17,20,21,26,27,28,30,31,34,35,36][12][24][13][14][35][16][17][18][19][22][25][23] evaluated the possible correlation between meat consumption and an increase of TMAO. Seven studies showed that the levels of urinary or plasma TMAO and/or TMA are significantly associated with the intake of meat. In most of these studies, the differences between white meat, red meat and preserved meat were not evaluated. Yu et al. showed that TMAO is strongly associated with deep-fried meat but not with red meat or poultry [27][16]. In one study, the effect on TMAO of meat and fish was compared. Fish was shown to induce a two-fold increase in urinary TMAO compared to meat [36][23]. Five papers [14,19,33,36,37][27][28][21][23][34] demonstrated that ingestion of meats has no measurable effects on plasma or urinary TMAO.
5. Dairy
Eight studies that assessed the correlation between fermented and non-fermented dairy consumption and increased TMAO were evaluated. Two papers [17,29][24][36] showed a positive association between dairy food consumption and plasma TMAO concentrations. Lower circulating and urinary TMAO with fermented dairy consumption compared to non-fermented dairy consumption has been shown [29][36].
6. Plant-Based Foods
Three papers evaluated plant-based food consumption [14,37][27][34]. Ingestion of fruits, vegetables, cereals [12] and fibre [35][25] did not significantly impact TMAO concentrations. Different foods were evaluated by Yu et al. [27][16]; they showed that consumption of soy foods or legumes does not modify urinary or plasma TMAO values.
References
- Velasquez, M.T.; Ramezani, A.; Manal, A.; Raj, D.S. Trimethylamine N-Oxide: The Good, the Bad and the Unknown. Toxins 2016, 8, 326.
- Baker, R.; Chaykin, S. The Biosynthesis of Trimethylamine-N-Oxide. J. Biol. Chem. 1962, 237, 1309–1313.
- Canyelles, M.; Tondo, M.; Cedó, L.; Farràs, M.; Escolà-Gil, J.C.; Blanco-Vaca, F. Trimethylamine N-Oxide: A Link among Diet, Gut Microbiota, Gene Regulation of Liver and Intestine Cholesterol Homeostasis and HDL Function. Int. J. Mol. Sci. 2018, 19, 3228.
- Fennema, D.; Phillips, I.R.; Shephard, E.A. Trimethylamine and Trimethylamine N-Oxide, a Flavin-Containing Monooxygenase 3 (FMO3)-Mediated Host-Microbiome Metabolic Axis Implicated in Health and Disease. Drug Metab. Dispos. 2016, 44, 1839–1850.
- Farhangi, M.A. Gut microbiota-dependent trimethylamine N-oxide and all-cause mortality: Findings from an updated systematic review and meta-analysis. Nutrients 2020, 78, 110856.
- Haghikia, A.; Li, X.S.; Liman, T.G.; Bledau, N.; Schmidt, D.; Zimmermann, F.; Kränkel, N.; Widera, C.; Sonnenschein, K.; Haghikia, A.; et al. Gut Microbiota–Dependent Trimethylamine N -Oxide Predicts Risk of Cardiovascular Events in Patients With Stroke and Is Related to Proinflammatory Monocytes. Arter. Thromb. Vasc. Biol. 2018, 38, 2225–2235.
- Tang, W.W.; Wang, Z.; Kennedy, D.J.; Wu, Y.; Buffa, J.A.; Agatisa-Boyle, B.; Li, X.S.; Levison, B.S.; Hazen, S.L. Gut Microbiota-Dependent TrimethylamineN-Oxide (TMAO) Pathway Contributes to Both Development of Renal Insufficiency and Mortality Risk in Chronic Kidney Disease. Circ. Res. 2015, 116, 448–455.
- Gruppen, E.G.; Garcia, E.; Connelly, M.A.; Jeyarajah, E.J.; Otvos, J.D.; Bakker, S.J.L.; Dullaart, R.P.F. TMAO is Associated with Mortality: Impact of Modestly Impaired Renal Function. Sci. Rep. 2017, 7, 1–9.
- Farhangi, M.A.; Vajdi, M. Novel findings of the association between gut microbiota–derived metabolite trimethylamine N-oxide and inflammation: Results from a systematic review and dose-response meta-analysis. Crit. Rev. Food Sci. Nutr. 2020, 60, 2801–2823.
- Obeid, R.; Awwad, H.M.; Rabagny, Y.; Graeber, S.; Herrmann, W.; Geisel, J. Plasma trimethylamine N-oxide concentration is associated with choline, phospholipids, and methyl metabolism. Am. J. Clin. Nutr. 2016, 103, 703–711.
- Svensson, B.; Åkesson, B.; Nilsson, A.; Paulsson, K. Urinary excretion of methylamines in men with varying intake of fish from the baltic sea. J. Toxicol. Environ. Health Part A 1994, 41, 411–420.
- Zhang, A.; Mitchell, S.; Smith, R. Dietary Precursors of Trimethylamine in Man: A Pilot Study. Food Chem. Toxicol. 1999, 37, 515–520.
- Krüger, R.; Merz, B.; Rist, M.J.; Ferrario, P.G.; Bub, A.; Kulling, S.E.; Watzl, B. Associations of current diet with plasma and urine TMAO in the KarMeN study: Direct and indirect contributions. Mol. Nutr. Food Res. 2017, 61.
- Cho, C.E.; Taesuwan, S.; Malysheva, O.V.; Bender, E.; Tulchinsky, N.F.; Yan, J.; Sutter, J.L.; Caudill, M.A. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial. Mol. Nutr. Food Res. 2017, 61, 1600324.
- Schmedes, M.; Balderas, C.; Aadland, E.K.; Jacques, H.; Lavigne, C.; Graff, I.E.; Eng, Ø.; Holthe, A.; Mellgren, G.; Young, J.F.; et al. The Effect of Lean-Seafood and Non-Seafood Diets on Fasting and Postprandial Serum Metabolites and Lipid Species: Results from a Randomized Crossover Intervention Study in Healthy Adults. Nutrients 2018, 10, 598.
- Yu, D.; Shu, X.; Rivera, E.S.; Zhang, X.; Cai, Q.; Calcutt, M.W.; Xiang, Y.; Li, H.; Gao, Y.; Wang, T.J.; et al. Urinary Levels of Trimethylamine-N-Oxide and Incident Coronary Heart Disease: A Prospective Investigation Among Urban Chinese Adults. J. Am. Hear. Assoc. 2019, 8, e010606.
- Andraos, S.; Lange, K.; Clifford, S.; Jones, B.; Thorstensen, E.B.; Kerr, J.; Wake, M.; Saffery, R.; Burgner, D.P.; O’Sullivan, J.M. Plasma Trimethylamine N-Oxide and Its Precursors: Population Epidemiology, Parent–Child Concordance, and Associations with Reported Dietary Intake in 11- to 12-Year-Old Children and Their Parents. Curr. Dev. Nutr. 2020, 4, nzaa103.
- De Souza, R.J.; Shanmuganathan, M.; Lamri, A.; Atkinson, S.; Becker, A.; Desai, D.; Gupta, M.; Mandhane, P.J.; Moraes, T.J.; Morrison, K.M.; et al. Maternal Diet and the Serum Metabolome in Pregnancy: Robust Dietary Biomarkers Generalizable to a Multiethnic Birth Cohort. Curr. Dev. Nutr. 2020, 4.
- Gessner, A.; Di Giuseppe, R.; Koch, M.; Fromm, M.F.; Lieb, W.; Maas, R. Trimethylamine-N-oxide (TMAO) determined by LC-MS/MS: Distribution and correlates in the population-based PopGen cohort. Clin. Chem. Lab. Med. 2020, 58, 733–740.
- Gibson, R.; Lau, C.-H.E.; Loo, R.L.; Ebbels, T.M.D.; Chekmeneva, E.; Dyer, A.R.; Miura, K.; Ueshima, H.; Zhao, L.; Daviglus, M.L.; et al. The association of fish consumption and its urinary metabolites with cardiovascular risk factors: The International Study of Macro-/Micronutrients and Blood Pressure (INTERMAP). Am. J. Clin. Nutr. 2019, 111, 280–290.
- Hagen, I.V.; Helland, A.; Bratlie, M.; Midttun, Ø.; McCann, A.; Sveier, H.; Rosenlund, G.; Mellgren, G.; Ueland, P.M.; Gudbrandsen, O.A. TMAO, creatine and 1-methylhistidine in serum and urine are potential biomarkers of cod and salmon intake: A randomised clinical trial in adults with overweight or obesity. Eur. J. Nutr. 2019, 59, 2249–2259.
- Hamaya, R.; Ivey, K.L.; Lee, D.H.; Wang, M.; Li, J.; Franke, A.; Sun, Q.; Rimm, E.B. Association of diet with circulating trimethylamine-N-oxide concentration. Am. J. Clin. Nutr. 2020, 112, 1448–1455.
- Yin, X.; Gibbons, H.; Rundle, M.; Frost, G.; McNulty, B.A.; Nugent, A.P.; Walton, J.; Flynn, A.; Brennan, L. The Relationship between Fish Intake and Urinary Trimethylamine-N-Oxide. Mol. Nutr. Food Res. 2020, 64, e1900799.
- Rohrmann, S.; Linseisen, J.; Allenspach, M.; von Eckardstein, A.; Müller, D. Plasma Concentrations of Trimethylamine-N-oxide Are Directly Associated with Dairy Food Consumption and Low-Grade Inflammation in a German Adult Population. J. Nutr. 2016, 146, 283–289.
- MacPherson, M.E.; Hov, J.R.; Ueland, T.; Dahl, T.B.; Kummen, M.; Otterdal, K.; Holm, K.; Berge, R.K.; Mollnes, T.E.; Trøseid, M.; et al. Gut Microbiota-Dependent Trimethylamine N-Oxide Associates with Inflammation in Common Variable Immunodeficiency. Front. Immunol. 2020, 11, 2217.
- Tang, W.W.; Wang, Z.; Levison, B.S.; Koeth, R.A.; Britt, E.B.; Fu, X.; Wu, Y.; Hazen, S.L. Intestinal Microbial Metabolism of Phosphatidylcholine and Cardiovascular Risk. N. Engl. J. Med. 2013, 368, 1575–1584.
- Miller, C.; Corbin, K.D.; Da Costa, K.-A.; Zhang, S.; Zhao, X.; Galanko, J.; Blevins, T.; Bennett, B.J.; O’Connor, A.; Zeisel, S.H. Effect of egg ingestion on trimethylamine-N-oxide production in humans: A randomized, controlled, dose-response study. Am. J. Clin. Nutr. 2014, 100, 778–786.
- Iannotti, L.L.; Lutter, C.K.; Waters, W.F.; Riofrío, C.A.G.; Malo, C.; Reinhart, G.; Palacios, A.; Karp, C.; Chapnick, M.; Cox, K.; et al. Eggs early in complementary feeding increase choline pathway biomarkers and DHA: A randomized controlled trial in Ecuador. Am. J. Clin. Nutr. 2017, 106, 1482–1489.
- Pignanelli, M.; Bogiatzi, C.; Gloor, G.; Allen-Vercoe, E.; Reid, G.; Urquhart, B.L.; Ruetz, K.N.; Velenosi, T.J.; Spence, J.D. Moderate Renal Impairment and Toxic Metabolites Produced by the Intestinal Microbiome: Dietary Implications. J. Ren. Nutr. 2019, 29, 55–64.
- West, A.A.; Shih, Y.; Wang, W.; Oda, K.; Jaceldo-Siegl, K.; Sabaté, J.; Haddad, E.; Rajaram, S.; Caudill, M.A.; Burns-Whitmore, B. Egg n-3 Fatty Acid Composition Modulates Biomarkers of Choline Metabolism in Free-Living Lacto-Ovo-Vegetarian Women of Reproductive Age. J. Acad. Nutr. Diet. 2014, 114, 1594–1600.
- DiMarco, D.M.; Missimer, A.; Murillo, A.G.; Lemos, B.S.; Malysheva, O.V.; Caudill, M.A.; Blesso, C.N.; Fernandez, M.L. Intake of up to 3 Eggs/Day Increases HDL Cholesterol and Plasma Choline While Plasma Trimethylamine-N-oxide is Unchanged in a Healthy Population. Lipids 2017, 52, 255–263.
- Lemos, B.S.; Medina-Vera, I.; Malysheva, O.V.; Caudill, M.A.; Fernandez, M.L. Effects of Egg Consumption and Choline Supplementation on Plasma Choline and Trimethylamine-N-Oxide in a Young Population. J. Am. Coll. Nutr. 2018, 37, 716–723.
- Missimer, A.; Fernandez, M.L.; DiMarco, D.M.; Norris, G.H.; Blesso, C.N.; Murillo, A.G.; Vergara-Jimenez, M.; Lemos, B.S.; Medina-Vera, I.; Malysheva, O.V.; et al. Compared to an Oatmeal Breakfast, Two Eggs/Day Increased Plasma Carotenoids and Choline without Increasing Trimethyl AmineN-Oxide Concentrations. J. Am. Coll. Nutr. 2017, 37, 140–148.
- Zhu, C.; Sawrey-Kubicek, L.; Bardagjy, A.S.; Houts, H.; Tang, X.; Sacchi, R.; Randolph, J.M.; Steinberg, F.M.; Zivkovic, A.M. Whole egg consumption increases plasma choline and betaine without affecting TMAO levels or gut microbiome in overweight postmenopausal women. Nutr. Res. 2020, 78, 36–41.
- Wang, Z.; Bergeron, N.; Levison, B.S.; Li, X.S.; Chiu, S.; Jia, X.; Koeth, R.; Li, L.; Wu, Y.; Tang, W.H.W.; et al. Impact of chronic dietary red meat, white meat, or non-meat protein on trimethylamine N-oxide metabolism and renal excretion in healthy men and women. Eur. Hear. J. 2019, 40, 583–594.
- Burton, K.J.; Krüger, R.; Scherz, V.; Münger, L.H.; Picone, G.; Vionnet, N.; Bertelli, C.; Greub, G.; Capozzi, F.; Vergères, G. Trimethylamine-N-Oxide Postprandial Response in Plasma and Urine Is Lower After Fermented Compared to Non-Fermented Dairy Consumption in Healthy Adults. Nutrients 2020, 12, 234.
