Phytochemicals have been used as antiviral agents against several viruses since they could inhibit via different mechanisms, either at the viral entry point or the replication stages and also immunomodulation potentials.
- COVID-19
- medicinal plants
- phytochemicals
- herbs
- antiviral agents
- SARS-CoV-2
1. Introduction
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19) has become a major pandemic, which has rapidly spread to more than 215 countries, causing serious global health concerns, panic, and huge economic losses [1]. Lack of specific treatment against SARS-CoV-2 has rendered the world helpless hence various countries are exploring phytochemicals obtained from medicinal plants and herbs as alternatives for treating COVID-19 patients via phytotherapy approaches [2][3][4][5][6]. Recent publications on SARS-CoV-2/COVID-19 suggest that phytochemicals used to treat the human immunodeficiency virus (HIV) infection can be explored for COVID-19 treatment [7]. Some of the most promising small plant molecules found to inhibit coronavirus are conjugated with fused ring structures and are classified as polyphenols [8]. In an in silico study conducted with SARS-CoV-2 main protease (Mpro) and angiotensin-converting enzyme 2 (ACE2) as targets in treating coronavirus infection, it was found that absinthin, quercetin 3-glucuronide-7-glucoside, and quercetin 3-vicianoside have a good binding potential to these targets [9]. Therefore, reliable and detailed knowledge of the structure of SARS-CoV-2 and pathogenesis of COVID-19 and also of plant phytochemicals will help us find a treatment for this coronavirus. SARS-CoV-2 has certain important factors that affect its virulence: the spike proteins that mediate its entry into the host, the nucleocapsid that protects its genetic material, and the RNA through which the virus replicates in the host [10]. There are various plants, including Glycyrrhiza glabra, Azadirachta indica, Andrographis paniculata, Calotropis gigantea, Ocimum sanctum, Curcuma longa, Withania somnifera, Zingiber officinale, Allium sativum, Tinospora cordifolia, Moringa oleifera, and others, that have anti-viral and immunomodulatory properties [11][12][13]. Plant-specific compounds, such as lignans, saponins, alkaloids, kaempferol, luteolin, apigenin, baicalin, quercetin, catechins, flavonoids, and polysulphates (sulphated polysaccharides) play various roles in inhibiting viral entry, destroying the nucleocapsid and genetic material, and inhibiting the replication of viruses, which includes, dengue, herpes simplex virus (HSV), hepatitis C virus (HCV), influenza, chikungunya, SARS, and others [13].
2. Structure and Pathogenesis of SARS-CoV-2
SARS-CoV-2 has a positive-sense, single-stranded RNA that is associated with nucleoproteins present in its capsid comprising matrix proteins [14]. The envelope is made up of club-shaped glycoprotein projections and few coronaviruses have hemagglutinin esterase (HE)-protein [15] in their envelope. SARS-CoV-2 contains four different structural proteins: the spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins, which is encoded by open reading fragments located on one-third of the genome near the 3’ terminal. Apart from the main structural proteins, it also has other structural and accessory proteins (HE, 3a/b protein, and 4a/b protein) that play various roles in replication and genome maintenance [16][17]. The membrane glycoprotein (M) is the most common structural protein and it covers the membrane bilayer. It has a short NH2-domain situated on the outside and a long -COOH terminal located within the virion [15]. The spike protein plays an important role as an inducer of neutralizing antibodies and also acts as a type I membrane glycoprotein along with peplomers. Figure 1 depicts the structure of SARS-CoV-2.
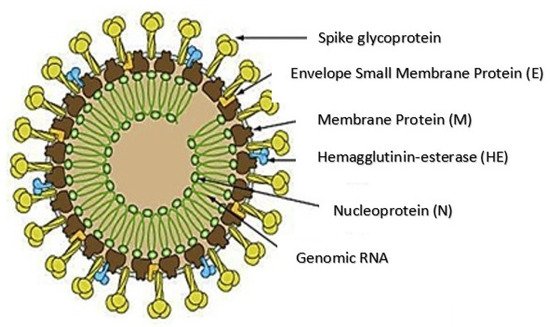
Figure 1. Structure of COVID-19 [Source: http://ruleof6ix.fieldofscience.com/2012/09/a-new-coronavirus-should-youcare html (accessed on 20 June 2020)].
SARS-CoV-2 enters the host through the binding of its spike proteins to ACE2 receptors, and this process is primed with the help of a protease called TMPRSS2 [18][19]. After entry, the virus gets uncoated and starts genome replication and translation at the cytoplasmic membrane with the help of a coordinated process of RNA synthesis (continuous and discontinuous) mediated by a complex of the protein encoded by 20kb replicase gene [20]. The coronaviruses have a replicase enzyme that is not found in other RNA viruses, with the presence of the putative sequence-specific endoribonuclease, 3′-to-5′exoribonucleases, 2′-o-ribo methyltransferases, and ADP-ribose-1’-phosphatase [21]. The mechanism of pathogenesis is represented in Figure 2.
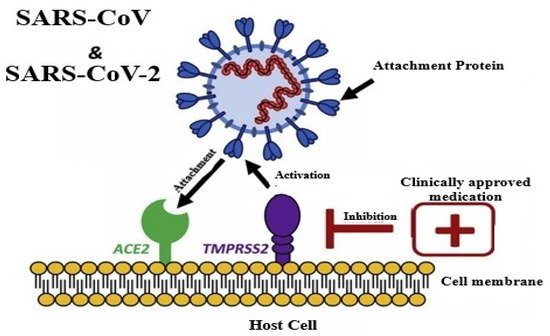
Figure 2. Pathology of COVID-19 [Source: Leila Mousavizadeh, Sorayya Ghasemi, Genotype and phenotype of COVID-19: Their roles in pathogenesis. Journal of Microbiology, Immunology and Infection. 2020].
3. Similarities of Viruses to SARS COV-2
The idea of SARS-CoV-2 structure and pathology will help in comparing viruses that share certain similarities. The zika virus is a single-stranded positive-sense RNA virus with nucleocapsid, the open reading frames codes a single protein which is processed into the capsid, membrane protein, and envelope structural proteins [22]. The rabies virus belongs to the RNA viruses. Although it is a negative RNA virus it has the lipid bilayer membrane covered with transmembrane glycoprotein spikes and a nucleocapsid that covers its genetic material [23]. Dengue virus has a positive-sense RNA [24]. The H1NI (swine flu virus) also affects the respiratory tract with a minimum incubation period of 5 to 7 days and it is an enveloped virus with glycoprotein spikes on the lipid bilayer membrane and also hemagglutinin on the envelope [25].
The chikungunya virus is also a spherical virus with an envelope consisting of glycoprotein spikes and a positive-sense single-stranded RNA [26]. The Ebola virus even though a tubular-shaped virus with negative-stranded RNA has a lipid bilayer membrane and glycoprotein spikes [27]. SARS-CoV2 Mpro and HCV NS3/4A protease shows similarity in three-dimensional structure and also in the arrangement of active site residues. Besides, 8 protease inhibitors of HCV are also capable of binding to Mpro active site suggesting that protease inhibitors of HCV can effectively inhibit SARS-CoV-2 protease and the replication of SARS-CoV2 [28]. Spike protein HE found in SARS-CoV2 and hemagglutinin of influenza virus has a similar function [29]. HIV has two copies of single-stranded positive-sense RNA and belonging to the retrovirus family [30]. All the above-mentioned viruses can be compared to their genetic material like RNA viruses or positive-sense RNA virus, a structure like spherical shape, glycoprotein spikes, hemagglutinin, lipid bilayer, nucleocapsid, and the site of infection with SARS CoV-2.
4. Plant-Specific Compounds and Antiviral Mechanisms
4.1. Flavonoids
Flavonoids are known for their antiviral activity. Many flavonoid compounds are well-known to act as antiviral agents by inhibiting the binding and entry of viral, its replication, translation of the viral protein, the formation of envelopes using glycoproteins complexes, and virus release [31]. Flavonoids help in the signaling process in the host cell by activating gene transcription factors and also by secreting cytokines [32]. The structure-activity relationship of flavonoids shows that it is a good inhibitor of the neuraminidase enzyme of the influenza virus, thereby preventing its replication [33]. Flavonoids have shown potential in therapy against COVID-19 [34]. They may inhibit SARS-CoV-2 entry into the cell [35] hence have been used in the therapy of COVID-19 patients [36].
4.2. Catechins
Green tea contains important catechins (polyphenols), which are of different types, such as (─)-epigallocatecheingallate (EGCG), (─)-epicatechingallate (ECG), and (─)-epogallocatechin (EGC), and has high medicinal values with health benefits [37]. In a quantitative study performed using RT-PCR, high concentrations of EGCG and ECG, but not EGC, decreased viral RNA synthesis in MDCK cells [38]. ECG and EGCG affected the activity of neuraminidase by inhibiting it more efficiently than EGC [38]. The neuraminidase enzyme in viruses is important in transporting budding viruses to other cells by cleaving the sialic acid present in glycoproteins located in the envelope. Similarly, EGCG inhibits both HSV-1 and HSV-2 by binding to their envelope proteins such as gB, gD, or other envelope proteins, which help for the fusion of the virus to cells [39]. Catechin binds the receptor-binding domain of viral S-protein, as well as ACE2 of the host, thus may serve as a therapeutic agent for COVID-19 [40]. In one of the docking analysis study, compound EGCG found in green tea revealed the highest binding affinity with S protein of SARS-CoV-2, which reflects its potential usage in preventing or treating the COVID-19 patients.
4.3. Quercetin
Quercetin is a flavonoid compound present in vegetables and fruits [41]. It is found to acts against the HCV virus by inhibiting the action of a heat shock protein that is involved in non-structural protein 5A-mediated translation of viral internal ribosome entry site [42]. Quercetin acts against HCV through the inhibition of HCV NS3 protease, which stops the replication of HCV in the subgenomic RNA replicon cell system [43]. Quercetin halts rhinovirus pathogenesis at different stages of the life cycle of the virus, which includs endocytosis, protein synthesis, and viral genome transcription [44]. Furthermore, quercetin, along with myricetin, quercetagetin, and baicalin, affected the growth of the Rauscher murine leukemia virus RLV [45]. Quercetin along with vitamin C has been proposed to have a synergistic effect in treating COVID-19 patients [36]. Synergistic antiviral, antioxidant, and immunomodulatory activities and the ability of ascorbate to recycle quercetin, increase the effectiveness of quercetin against SARS-CoV-2 [36].
4.4. Apigenin and Baicalin
Apigenin acts against the African swine fever virus by decreasing protein synthesis, thereby causing a three-log decrease in the yield of viruses and is also effective against DNA viruses such as adenoviruses and (hepatitis B virus) HBV [46]. It shows potent antiviral effects against RNA viruses such as picornavirus and acts by inhibiting viral IRES activity, thereby inhibiting the synthesis of viral proteins [47][48]. The translation of enterovirus-71 is disrupted by inhibition of the association of viral RNA with transacting factors that regulate enterovirus-71 [49]. Apigenin is found to disturb HCV virus replication by decreasing the microRNA122, which is a liver-specific microRNA [50].
Baicalin acts against HBV by disrupting its DNA and viral protein synthesis [51]. In H5N1 virus infection, baicalin lowers the levels of interleukin-6 and -8 (IL-6; IL-8) produced but does not interfere with IP-10 levels [52]. Baicalin can inhibit the synthesis of human cytomegalovirus DNA and proteins; however, it does not affect the viral polymerase activity. Baicalin, by interfering with neuraminidase activity, stops the replication of H5N1 in the human lung- and monocyte-derived macrophages [52]. H1N1-infected BALB/c mice administered baicalin orally showed decreased lung virus titers and an increased mean time of death [53]. The results were also found in mice infected with the Sendai virus [54]. Studies have shown that baicalin could help in the production of IFN-γ by CD4+ and CD8+ T cells during infection with the influenza virus [55]. In silico studies on baicalin strongly suggest that it has a good binding ability with the NS3/NS2B protein of the dengue virus; however, baicalin shows better interactions with NS5 protein.
4.5. Luteolin
Luteolin and luteolin-rich fractions are found to have antiviral property, including SARS–CoV, chikungunya virus, Japanese encephalitis virus, and rhesus rotaviruses [56][57][58][59]. Luteolin inhibited HIV-1 by preventing clade B- and C- Tat-driven long terminal repeat (LTR) transactivation [60]. In the case of the Epstein-Barr virus, luteolin deregulated the binding of transcription factor Sp1, which decreased the activity of early genes Zta and Rta [61]. Above all, it was found to be the most potent compound among 400 natural compounds against enterovirus-71 and coxsackievirus A 16 infections, since it disrupts viral RNA replication [62]. Luteolin has antiviral, anti-inflammatory, neurotrophic actions, anti-oxidant, anti-cancer, and anti-apoptotic activities [63]. It has shown the ability to inhibit the entry of the SARS-CoV virus and fusion with human receptors, thus may have potential anti-SARS-CoV-2 activity [63].
4.6. Kaempferol
The compound kaempferol obtained from Ficus benjamina has demonstrated to have a protective effect on HSV-1 and HSV-2, except for its aglycone form [64]. A rhamnose residue containing kaempferol inhibits coronavirus release by affecting 3a channels [65]. Kaempferol and kaempferol-7-o-glucoside display inhibitory effect on HIV 1 reverse transcriptase. Besides, kaempferol 3,7-bisrhamnoside isolated from Taxillus sutchuenensis, is effective against HCV NS3 protease function [66]. In the case of H1N1 and H9N2 influenza viruses, kaempferol affects neuraminidase activity using specific functional groups [67]. RNA frameshift site (fs RNA) is found to be the target site of kaempferol, which serves to inhibit the Japanese encephalitis virus [68]. Kaempferol has more binding stability and its structural features have shown that it affects binding at the site of N3 in the SARS-CoV-2 Mpro [69].
4.7. Alkaloids
Lycorine is the most important alkaloids found in the Amaryllidaceae family. The lycorine was found to inhibit the poliomyelitis virus in Vero cells at a low concentration of 1 µg/mL but was cytotoxic at a concentration of 25 µg/mL [70]. Lycorine obtained from Lycoris radiata had significant antiviral activity against two strains (BJ001, BJ006) of SARS-CoV grown on Vero cells, with an EC50 at 15.7 ± 1.2 nM, CC50 at 14,980.0 ± 912.0 nM, and a selective index (SI), which is greater than 900 [71]. This SI index is a ratio between the antiviral effect and the toxicity of a compound; the greater the SI value, the safer the drug could be when administered in vitro [72]. Another compound, sophoridine, was found to have antiviral activity against Enterovirus-71 when Vero cells were pretreated with sophoridine before being infected with this virus [73]. In a study conducted with coxsackievirus in mice, sophoridine obtained from Sophora flavescens had a potential role in enhancing the expression of IFN-γ and interleukin-10 (IL-10) to increase the host resistance response against the virus [74]. Among the ipecac, alkaloidsemetine, ipecac alkaloids and analogues are possible antiviral agents for CoVs, hence having prospects for use in COVID-19 therapy [75].
4.8. Saponins
Saponin isolated from Anagallis arvensis was found to have antiviral property against poliovirus-2 and HSV-1 by protecting the host cells from structural damage [76]. Tormentic acid glucosyl ester, a triterpenoid saponin demonstrated antiviral property against HSV-1 by inhibiting its viral capsid protein synthesis and DNA replication, respectively [77]. Administration of polyphylla saponin I (obtained from Paris polyphylla, 5–10 mg/kg) and oseltamivir (3 mg/kg) to mice infected with influenza virus decreased viral hemagglutination titers and reduced pathological conditions in lung tissues of the infected mice, thereby reducing their mortality [78]. Saponins may inhibit the cellular attachment, entry, adsorption, and penetration of a virion into the host cell. Saponins possess immunomodulatory, anti-inflammatory activities, anti-proliferative effect, and antiviral activities including SARS-CoV [4][79][80], hence may have a role in curing COVID-19 patients [79].
4.9. Lignans
Lignans are phenolic compounds derived from the shikimic acid biosynthetic pathway in plants [81]. Niranthin obtained from Phyllanthus niruri acts against the HBV virus by inhibiting its antigen expression in vitro; it also inhibits duck HBV by inhibiting its DNA replication [82][83]. Nordihydroguaiaretic acid, found in the leaves of Larrea tridentata, shows antiviral properties against various viruses, including HCV, dengue virus, influenza A virus, and zika virus by inhibiting genome replication and viral assembly. It affects HCV proliferation by altering host lipid metabolism, interfering with the lipid metabolism and it also suppresses the replication of influenza A virus [83][84][85][86][87]. Terameprocol, a semisynthetic compound from lignin, which is derived from the leaves of L. tridentata acts against the West Nile virus by affecting viral replication against poxvirus by inhibiting the cell-to-cell transfer of the virus, and against HSV and HIV by preventing viral replication through inhibition of the binding with host transcription factor [88][89][90][91][92]. Arctigenin demonstrates antiviral properties including influenza A virus and HIV-1 by inducing the release of IFNs and also by inhibiting the expression of the proteins (p17 and p24) of the HIV-1 virus [93][94][95][96][97].
The addition of yatein, a compound obtained from the dried leaves of Chamaecyparis obtusa, to HeLa cells inhibited the expression of HSV-1ICP0 and ICP4 that arrests DNA synthesis in HSV [98][99]. The compound diphyllin obtained from epigeal parts of the genus Haplophyllum inhibits the vacuolar ATPase in zika virus infection; it also interferes with the downstream replication of influenza A virus to inhibit its infection [100][101][102][103][104]. Patentiflorin obtained from the leaves and stem of Justicia gendarussa acts against zika virus by impeding its fusion with the host cellular membrane, thus preventing infection by avoiding the acidification of lysosomal or endosomal cells of the target. This acts against HIV-1 by inhibiting its reverse transcriptase enzyme [103][104][105][106][107]. Clemastanin B affects viral endocytosis and ribonucleoprotein export from the nucleus while acting against influenza A virus [107][108][109][110]. Silymarin obtained from the seeds of Silybum marianum inhibits HCV production by increasing the expression of anti-inflammatory and anti-proliferative genes, but it does not affect serum albumin levels [111][112]. Thus, having considerable antiviral effects through the inhibition of viral replication, lipid metabolism, apoptosis, protein, and cytokine expression; lignins may have potent anti-SARS-CoV-2 actions as they have shown effects against SARS-CoV also [113][114].
4.10. Tannins
Tannins have the potential in targeting viral replication at different stages like attacking their attachment, host replication process, viral particle assembly, and protein transport [115]. Ellagitannins, 1,3,4,6-tetra-O-galloyl-β-d-glucose and geraniin present in Phyllanthus urinaria were found to be useful in suppressing the HSV-1 and HSV-2 respectively [116]. Corilagin and geraniin (ellagitannins) found in Phyllanthus amarus reduced the interaction of HIV and its replication [117]. Punicalagin and chebulagic acid, two hydrolysable tannins present in Terminalia chebula have been successful in inhibiting the viral entry and transport of virus in HSV-1 [118].
According to the study conducted with the combination of ellagitannins like castalagin, vescalagin, and grandinin with acyclovir, the effect of castalagin and vescalagin versus HSV-1 was found to be identical to acyclovir, which interpreted that the combination of ellagitannins with acyclovir was efficient [119][120]. Castalagin followed by vescalagin have the highest activity against alphaherpesvirus-1 [121]. Castalagin was also found to inhibit the HSV-1 replication with its highest sensitivity being recorded at 0–3 h post-viral inoculation [122].
Various plants and herbs have shown effective antiviral and immune-boosting potentials against emerging viruses such as SARS-CoV, zika, ebola, nipah virus, and other highly pathogenic viruses [8][71][109][123][124][125][126]. Apart from developing effective vaccines, therapeutics, and antiviral drugs, the potent antiviral applications of various plants, plant extracts and herbs are required to be endorsed and proliferated optimally by strengthening researches and development activities along with conducting appropriate clinical trials and validation experiments to combat COVID-19 pandemic and its high challenges posed [12][127][128][129][130][131][132][133][134][135]. Advances in the fields of biotechnology, immunology, biochemistry, pharmacology, pharmaceuticals, and nanotechnology may be warranted to their full potential for developing successful antiviral drugs and medicines out of these safe and valuable natural resources against SARS-CoV-2 [136][137][138][139][140][141][142][143][144]. Beneficial applications of medicinal values of plants and herbs could lessen the high incidences, devastating scenario, and public health concerns of SARS-CoV-2/COVID-19. Figure 3 represented the antiviral properties of the plant compounds.
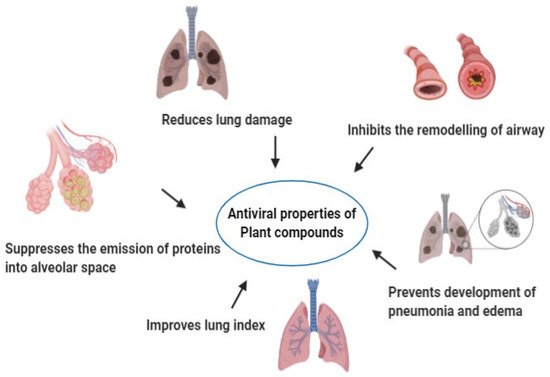
Figure 3. Antiviral properties of plant compounds.
References
- Dhama, K.; Khan, S.; Tiwari, R.; Sircar, S.; Bhat, S.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Coronavirus disease 2019-COVID-19. Clin. Microbiol. Rev. 2020, 33, e00028-20.
- Aanouz, I.; Belhassan, A.; El-Khatabi, K.; Lakhlifi, T.; El-Ldrissi, M.; Bouachrine, M. Moroccan Medicinal plants as inhibitors against SARS-CoV-2 main protease: Computational investigations. J. Biomol. Struct. Dyn. 2020, 1–9.
- Divya, M.; Vijayakumar, S.; Chen, J.; Vaseeharan, B.; Durán-Lara, E.F. A review of South Indian medicinal plant has the ability to combat against deadly viruses along with COVID-19? Microb. Pathog. 2020, 104277.
- Jahan, I.; Onay, A. Potentials of plant-based substance to inhabit and probable cure for the COVID-19. Turk. J. Biol 2020, 44, 228–241.
- Ul Qamar, M.T.; Alqahtani, S.M.; Alamri, M.A.; Chen, L.L. Structural basis of SARS-CoV-2 3CLpro and anti-COVID-19 drug discovery from medicinal plants. J. Pharm. Anal. 2020, 10, 313–319.
- Xu, J.; Zhang, Y. Traditional Chinese medicine treatment of COVID-19. Complement. Clin. Pr. 2020, 39, 101165.
- Devanssh, M. Possible plant based medicines and phytochemicals to be cure for deadly coronavirus COVID 19. World J. Pharm. Pharm. Sci. 2020, 9, 531–533.
- Mani, J.S.; Johnson, J.B.; Steel, J.C.; Broszczak, D.A.; Neilsen, P.M.; Walsh, K.B.; Naiker, M. Natural product-derived phytochemicals as potential agents against coronaviruses: A review. Virus Res. 2020, 284, 197989.
- Joshi, T.; Joshi, T.; Sharma, P.; Mathpal, S.; Pundir, H.; Bhatt, V.; Chandra, S. In silico screening of natural compounds against COVID-19 by targeting Mpro and ACE2 using molecular docking. Eur. Rev. Med. Pharm. Sci. 2020, 24, 4529–4536.
- Guo, Y.R.; Cao, Q.D.; Hong, Z.S.; Tan, Y.Y.; Chen, S.D.; Jin, H.J.; Tan, K.S.; Wang, D.Y.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil. Med Res. 2020, 7, 1–10.
- Ganjhu, R.K.; Mudgal, P.P.; Maity, H.; Dowarha, D.; Devadiga, S.; Nag, S.; Arunkumar, G. Herbal plants and plant preparations as remedial approach for viral diseases. Virusdisease 2015, 26, 225–236.
- Tiwari, R.; Latheef, S.K.; Ahmed, I.; Iqbal, H.; Bule, M.H.; Dhama, K.; Samad, H.A.; Karthik, K.; Alagawany, M.; El-Hack, M.E.; et al. Herbal immunomodulators—A remedial panacea for designing and developing effective drugs and medicines: Current scenario and future prospects. Curr. Drug Metab. 2018, 19, 264–301.
- Dhama, K.; Karthik, K.; Khandia, R.; Munjal, A.; Tiwari, R.; Rana, R.; Khurana, S.K.; Ullah, S.; Khan, R.U.; Alagawany, M.; et al. Medicinal and therapeutic potential of herbs and plant metabolites / extracts countering viral pathogens—Current knowledge and future prospects. Curr. Drug Metab. 2018, 19, 236–263.
- Mousavizadeh, L.; Ghasemi, S. Genotype and phenotype of COVID-19: Their roles in pathogenesis. J. Microbiol. Immunol. Infect. 2020, S1684-1182(20)30082-7.
- De Haan, C.A.; Kuo, L.; Masters, P.S.; Vennema, H.; Rottier, P.J. Coronavirus particle assembly: Primary structure requirements of the membrane protein. J. Virol. 1998, 72, 6838–6850.
- van Boheemen, S.; de Graaf, M.; Lauber, C.; Bestebroer, T.M.; Raj, V.S.; Zaki, A.M.; Osterhaus, A.D.; Haagmans, B.L.; Gorbalenya, A.E.; Snijder, E.J.; et al. Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio 2012, 3, e00473-12.
- Czub, M.; Weingartl, H.; Czub, S.; He, R.; Cao, J. Evaluation of modified vaccinia virus Ankara based recombinant SARS vaccine in ferrets. Vaccine 2005, 23, 2273–2279.
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280.e8.
- South, A.M.; Brady, T.M.; Flynn, J.T. ACE2 (Angiotensin-Converting Enzyme 2), COVID-19, and ACE Inhibitor and Ang II (Angiotensin II) receptor blocker use during the pandemic: The pediatric perspective. Hypertension 2020, 76, 16–22.
- Sola, I.; Almazan, F.; Zuniga, S.; Enjuanes, L. Continuous and discontinuous RNA synthesis in coronaviruses. Annu. Rev. Virol. 2015, 2, 265–288.
- Ziebuhr, J. Coronavirus replication and reverse genetics. In Current Topics in Microbiology and Immunology; Enjuanes, L., Ed.; Springer: Berlin/Heidelberg, Germany, 2005; Volume 287, pp. 57–94.
- Šebera, J.; Dubankova, A.; Sychrovský, V.; Ruzek, D.; Boura, E.; Nencka, R. The structural model of Zika virus RNA-dependent RNA polymerase in complex with RNA for rational design of novel nucleotide inhibitors. Sci. Rep. 2018, 8, 11132.
- Rupprecht, C.E. Rhabdovirus. In Medical Microbiology, 4th ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996.
- Kuhn, R.J.; Zhang, W.; Rossmann, M.G.; Pletnev, S.V.; Corver, J.; Lenches, E.; Jones, C.T.; Mukhopadhyay, S.; Chipman, P.R.; Strauss, E.G.; et al. Structure of dengue virus: Implications for flavivirus organization, maturation, and fusion. Cell 2002, 108, 717–725.
- Jilani, T.N.; Jamil, R.T.; Siddiqui, A.H. H1N1 influenza (swine flu). In StatPearls; Stat Pearls Publishing: Treasure Island, FL, USA, 2019.
- Ganesan, V.K.; Duan, B.; Reid, S.P. Chikungunya virus: Pathophysiology, mechanism, and modeling. Viruses 2017, 9, 368.
- Lee, J.E.; Saphire, E.O. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol. 2009, 4, 621–635.
- Bafna, K.; Krug, R.M.; Montelione, G.T. Structural similarity of SARS-CoV-2 Mpro and HCV NS3/4A proteases suggests new approaches for identifying existing drugs useful as COVID-19 therapeutics. ChemRxiv 2020.
- Biswas, A.; Bhattacharjee, U.; Chakrabarti, A.K.; Tewari, D.N.; Banu, H.; Dutta, S. Emergence of novel coronavirus and COVID-19: Whether to stay or die out? Crit. Rev. Microbiol. 2020, 46, 182–193.
- Fanales-Belasio, E.; Raimondo, M.; Suligoi, B.; Buttò, S. HIV virology and pathogenetic mechanisms of infection: A brief overview. Ann. Sanita 2010, 46, 5–14.
- Ogbole, O.O.; Akinleye, T.E.; Segun, P.A.; Faleye, T.C.; Adeniji, A.J. In vitro antiviral activity of twenty-seven medicinal plant extracts from Southwest Nigeria against three serotypes of echoviruses. Virol. J. 2018, 15, 110.
- Andres, A.; Donovan, S.M.; Kuhlenschmidt, M.S. Soy isoflavones and virus infections. J. Nutr. Biochem. 2009, 20, 563–569.
- Liu, A.L.; Liu, B.; Qin, H.L.; Lee, S.M.; Wang, Y.T.; Du, G.H. Anti-influenza virus activities of flavonoids from the medicinal plant Elsholtzia rugulosa. Planta Med. 2008, 74, 847–851.
- Ngwa, W.; Kumar, R.; Thompson, D.; Lyerly, W.; Moore, R.; Reid, T.E.; Lowe, H.; Toyang, N. Potential of flavonoid-inspired phytomedicines against COVID-19. Molecules 2020, 25, 2707.
- Bhowmik, D.; Nandi, R.; Kumar, D. Evaluation of flavonoids as 2019-nCoV cell entry inhibitor through molecular docking and pharmacological analysis. ChemRxiv 2020.
- Colunga Biancatelli, R.M.L.; Berrill, M.; Catravas, J.D.; Marik, P.E. Quercetin and vitamin C: An experimental, synergistic therapy for the prevention and treatment of SARS-CoV-2 related disease (COVID-19). Front. Immunol. 2020, 11, 1451.
- Saeed, M.; Naveed, M.; Arif, M.; Kakar, M.U.; Manzoor, R.; Abd El-Hack, M.E.; Alagawany, M.; Tiwari, R.; Khandia, R.; Munjal, A.; et al. Green tea (Camellia sinensis) and l-theanine: Medicinal values and beneficial applications in humans-A comprehensive review. Biomed. Pharm. 2017, 95, 1260–1275.
- Song, J.M.; Lee, K.H.; Seong, B.L. Antiviral effect of catechins in green tea on influenza virus. Antivir. Res. 2005, 68, 66–74.
- Isaacs, C.E.; Wen, G.Y.; Xu, W.; Jia, J.H.; Rohan, L.; Corbo, C.; Di Maggio, V.; Jenkins, E.C.; Hillier, S. Epigallocatechin gallate inactivates clinical isolates of herpes simplex virus. Antimicrob. Agents Chemother. 2008, 52, 962–970.
- Jena, A.B.; Kanungo, N.; Nayak, V.; Chainy, G.B.N.; Dandapat, J. Catechin and curcumin interact with corona (2019-nCoV/SARS-CoV2) viral S protein and ACE2 of human cell membrane: Insights from computational study and implication for intervention. Nature 2020.
- Harwood, M.; Danielewska-Nikiel, B.; Borzelleca, J.F.; Flamm, G.W.; Williams, G.M.; Lines, T.C. A critical review of the data related to the safety of quercetin and lack of evidence of in vivo toxicity, including lack of genotoxic/carcinogenic properties. Food Chem. Toxicol. 2007, 45, 2179–2205.
- Gonzalez, O.; Fontanes, V.; Raychaudhuri, S.; Loo, R.; Loo, J.; Arumugaswami, V.; Sun, R.; Dasgupta, A.; French, S.W. The heat shock protein inhibitor Quercetin attenuates hepatitis C virus production. Hepatology 2009, 50, 1756–1764.
- Bachmetov, L.; Gal-Tanamy, M.; Shapira, A.; Vorobeychik, M.; Giterman-Galam, T.; Sathiyamoorthy, P.; Golan-Goldhirsh, A.; Benhar, I.; Tur-Kaspa, R.; Zemel, R. Suppression of hepatitis C virus by the flavonoid quercetin is mediated by inhibition of NS3 protease activity. J. Viral Hepat. 2012, 19, e81–e88.
- Ganesan, S.; Faris, A.N.; Comstock, A.T.; Wang, Q.; Nanua, S.; Hershenson, M.B.; Sajjan, U.S. Quercetin inhibits rhinovirus replication in vitro and in vivo. Antivir. Res. 2012, 94, 258–271.
- Zandi, K.; Teoh, B.T.; Sam, S.S.; Wong, P.F.; Mustafa, M.R.; Abu Bakar, S. Antiviral activity of four types of bioflavonoid against dengue virus type-2. Virol. J. 2011, 8, 1.
- Hakobyan, A.; Arabyan, E.; Avetisyan, A.; Abroyan, L.; Hakobyan, L.; Zakaryan, H. Apigenin inhibits African swine fever virus infection in vitro. Arch. Virol. 2016, 161, 3445–3453.
- Lv, X.; Qiu, M.; Chen, D.; Zheng, N.; Jin, Y.; Wu, Z. Apigenin inhibits enterovirus 71 replication through suppressing viral IRES activity and modulating cellular JNK pathway. Antivir. Res. 2014, 109, 30–41.
- Rogerio, A.P.; Dora, C.L.; Andrade, E.L.; Chaves, J.S.; Silva, L.F.; Lemos-Senna, E.; Calixto, J.B. Anti-inflammatory effect of quercetin-loaded microemulsion in the airways allergic inflammatory model in mice. Pharmacol. Res. 2010, 1, 288–297.
- Zhang, W.; Qiao, H.; Lv, Y.; Wang, J.; Chen, X.; Hou, Y.; Tan, R.; Li, E. Apigenin inhibits enterovirus-71 infection by disrupting viral RNA association with trans-acting factors. PLoS ONE 2014, 9, e110429.
- Shibata, C.; Ohno, M.; Otsuka, M.; Kishikawa, T.; Goto, K.; Muroyama, R.; Kato, N.; Yoshikawa, T.; Takata, A.; Koike, K. The flavonoid apigenin inhibits hepatitis C virus replication by decreasing mature microRNA122 levels. Virology 2014, 462, 42–48.
- Huang, H.; Zhou, W.; Zhu, H.; Zhou, P.; Shi, X. Baicalin benefits the anti-HBV therapy via inhibiting HBV viral RNAs. Toxicol. Appl. Pharm. 2017, 323, 36–43.
- Sithisarn, P.; Michaelis, M.; Schubert-Zsilavecz, M.; Cinatl Jr, J. Differential antiviral and anti-inflammatory mechanisms of the flavonoids biochanin A and baicalein in H5N1 influenza A virus-infected cells. Antivir. Res. 2013, 97, 41–48.
- Xu, G.; Dou, J.; Zhang, L.; Guo, Q.; Zhou, C. Inhibitory effects of baicalein on the influenza virus in vivo is determined by baicalin in the serum. Biol. Pharm. Bull. 2010, 33, 238–243.
- Dou, J.; Chen, L.; Xu, G.; Zhang, L.; Zhou, H.; Wang, H.; Su, Z.; Ke, M.; Guo, Q.; Zhou, C. Effects of baicalein on Sendai virus in vivo are linked to serum baicalin and its inhibition of hemagglutinin-neuraminidase. Arch. Virol. 2011, 156, 793–801.
- Chu, M.; Xu, L.; Zhang, M.B.; Chu, Z.Y.; Wang, Y.D. Role of Baicalin in anti-influenza virusA as a potent inducer of IFN gamma. Biomed. Res. Int. 2015, 2015, 263630.
- Fan, W.; Qian, S.; Qian, P.; Li, X. Antiviral activity of luteolin against Japanese encephalitis virus. Virus Res. 2016, 220, 112–116.
- Knipping, K.; Garssen, J.; van’t, L.B. An evaluation of the inhibitory effects against rotavirus infection of edible plant extracts. Virol. J. 2012, 9, 1–8.
- Murali, K.S.; Sivasubramanian, S.; Vincent, S.; Murugan, S.B.; Giridaran, B.; Dinesh, S.; Gunasekaran, P.; Krishnasamy, K.; Sathishkumar, R. Anti-chikungunya activity of luteolin and apigenin rich fraction from Cynodon dactylon. Asian Pac. J. Trop. Med. 2015, 8, 352–358.
- Yi, L.; Li, Z.; Yuan, K.; Qu, X.; Chen, J.; Wang, G.; Zhang, H.; Luo, H.; Zhu, L.; Jiang, P.; et al. Small molecules blocking the entry of severe acute respiratory syndrome coronavirus into host cells. J. Virol. 2004, 78, 11334–11339.
- Mehla, R.; Bivalkar-Mehla, S.; Chauhan, A. Aflavonoid, luteolin, cripples HIV-1 by abrogation of tat function. PLoS ONE 2011, 6, e27915.
- Wu, H.; Myszka, D.G.; Tendian, S.W.; Brouillette, C.G.; Sweet, R.W.; Chaiken, I.M.; Hendrickson, W.A. Kinetic and structural analysis of mutant CD4 receptors that are defective in HIV gp120 binding. Proc. Natl. Acad. Sci. USA 1996, 93, 15030–15035.
- Xu, L.; Su, W.; Jin, J.; Chen, J.; Li, X.; Zhang, X.; Sun, M.; Sun, S.; Fan, P.; An, D.; et al. Identification of luteolin as enterovirus 71 and coxsackievirus A16 inhibitors through reporter viruses and cell viability-based screening. Viruses 2014, 6, 2778–2795.
- Ansari, W.A.; Ahamad, T.; Khan, M.A.; Khan, Z.A.; Khan, M.F. Luteolin: A dietary molecule as potential anti-COVID-19 agent. Comput. Chem. 2020.
- Mitrocotsa, D.; Mitaku, S.; Axarlis, S.; Harvala, C.; Malamas, M. Evaluation of the antiviral activity of kaempferol and its glycosides against human cytomegalovirus. Planta Med. 2000, 66, 377–379.
- Schwarz, S.; Sauter, D.; Wang, K.; Zhang, R.; Sun, B.; Karioti, A.; Bilia, A.R.; Efferth, T.; Schwarz, W. Kaempferol derivatives as antiviral drugs against the 3a channel protein of coronavirus. Planta Med. 2014, 80, 177–182.
- Yang, L.; Lin, J.; Zhou, B.; Liu, Y.; Zhu, B. Activity of compounds from Taxillus sutchuenensis as inhibitors of HCV NS3serine protease. Nat. Prod. Res. 2016, 13, 1–5.
- Jeong, H.J.; Ryu, Y.B.; Park, S.; Kim, J.H.; Kwon, H.-J.; Kim, J.H.; Park, K.H.; Rho, M.-C.; Lee, W.S. Neuraminidase inhibitory activities of flavonols isolated from Rhodiola rosea roots and their in vitro anti-influenza viral activities. Bioorg. Med. Chem. 2009, 17, 6816–6823.
- Zhang, T.; Wu, Z.; Du, J.; Hu, Y.; Liu, L.; Yang, F.; Jin, Q. Anti-Japanese-encephalitis-viral effects of kaempferol and daidzin and their RNA-binding characteristics. PLoS ONE 2012, 7, e30259.
- Owis, A.I.; El-Hawary, M.S.; Dalia, E.L.; Amir Omar, M.A.; Abdelmohsen, U.R.; Kamel, M.S. Molecular docking reveals the potential of Salvadora persica flavonoids to inhibit COVID-19 virus main protease. RSC Adv. 1957, 10, 19570–19575.
- Ieven, M.; Vlietinick, A.J.; Berghe, D.V.; Totte, J.; Dommisse, R.; Esmans, E.; Alderweireldt, F. Plant antiviral agents. III. Isolation of alkaloids from Clivia miniata Regel (Amaryl-lidaceae). J. Nat. Prod. 1982, 45, 564–573.
- Li, S.Y.; Chen, C.; Zhang, H.Q.; Guo, H.Y.; Wang, H.; Wang, L.; Zhang, X.; Hua, S.N.; Yu, J.; Xiao, P.G.; et al. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antivir. Res. 2005, 67, 18–23.
- Flamand, L.; Lautenschlager, I.; Krueger, G.; Ablashi, D. (Eds.) Human Herpesviruses HHV-6A, HHV-6B and HHV-7: Diagnosis and Clinical Management; Elsevier: Amsterdam, The Netherlands, 2014.
- Ren, G.; Ding, G.; Zhang, H.; Wang, H.; Jin, Z.; Yang, G.; Han, Y.; Zhang, X.; Li, G.; Li, W. Antiviral activity of sophoridine against enterovirus 71 in vitro. J. Ethnopharmacol. 2019, 236, 124–128.
- Zhang, Y.; Zhu, H.; Ye, G.; Huang, C.; Yang, Y.; Chen, R.; Yu, Y.; Cui, X. Antiviral effects of sophoridine against coxsackievirus B3 and its pharmacokinetics in rats. Life Sci. 2006, 78, 1998–2005.
- Bleasel, M.D.; Peterson, G.M. Emetine, Ipecac, Ipecac, Alkaloids and analogues as potential antiviral agents for coronaviruses. Pharmaceuticals 2020, 13, 51.
- Amoros, M.; Fauconnier, B.; Girre, R.L. In vitro antiviral activity of a saponin from Anagallis arvensis, Primulaceae, against herpes simplex virus and poliovirus. Antivir. Res. 1987, 8, 13–25.
- Simões, C.M.; Amoros, M.; Girre, L. Mechanism of antiviral activity of triterpenoid saponins. Phytother. Res. 1999, 13, 323–328.
- Pu, X.; Ren, J.; Ma, X.; Liu, L.; Yu, S.; Li, X.; Li, H. Polyphylla saponin I has antiviral activity against influenza A virus. Int. J. Clin. Exp. Med. 2015, 8, 18963.
- Bahbah, E.I.; Negida, A.; Nabet, M.S. Purposing saikosaponins for the treatment of COVID-19. Med. Hypotheses 2020, 140, 109782.
- Yan, Y.M.; Shen, X.; Cao, Y.K.; Zhang, J.J.; Wang, Y.; Cheng, Y.X. Discovery of anti-2019-nCoV agents from Chinese patent drugs via docking screening. Hypothesis 2020.
- Teponno, R.B.; Kusari, S.; Spiteller, M. Recent advances in research on lignans and neolignans. Nat. Prod. Rep. 2016, 33, 1044–1092.
- Huang, R.L.; Huang, Y.L.; Ou, J.C.; Chen, C.C.; Hsu, F.L.; Chang, C. Screening of 25 compounds isolated from Phyllanthus species for anti-human hepatitis B virus in vitro. Phytother. Res. 2003, 17, 449–453.
- Liu, S.; Wei, W.; Shi, K.; Cao, X.; Zhou, M.; Liu, Z. In vitro and in vivo anti-hepatitis B virus activities of the lignan niranthin isolated from Phyllanthus niruri L. J. Ethnopharmacol. 2014, 155, 1061–1067.
- Soto-Acosta, R.; Bautista-Carbajal, P.; Syed, G.H.; Siddiqui, A.; DelAngel, R.M. Nordihydroguaiaretic acid (NDGA) inhibits replication and viral morphogenesis of dengue virus. Antivir. Res. 2014, 109, 132–140.
- Syed, G.H.; Siddiqui, A. Effects of hypolipidemic agent nordihydroguaiaretic acid on lipid droplets and hepatitis C virus. Hepatology 2011, 54, 1936–1946.
- Merino-Ramos, T.; de Oya, N.J.; Saiz, J.C.; Martín-Acebes, M.A. Antiviral activity of nordihydroguaiaretic acid and its derivative tetra-O-methyl nordihydroguaiaretic acid against West Nile virus and Zika virus. Antimicrob. Agents Chemother. 2017, 61, e00376-17.
- Wang, S.; Le, T.Q.; Kurihara, N.; Chida, J.; Cisse, Y.; Yano, M.; Kido, H. Influenza virus—cytokine-protease cycle in the pathogenesis of vascular hyperpermeability in severe influenza. J. Infect. Dis. 2010, 202, 991–1001.
- Oyegunwa, A.O.; Sikes, M.L.; Wilson, J.; Scholle, F.; Laster, S.M. Tetra-O-methyl nordihydroguaiaretic acid (Terameprocol) inhibits the NF-κB-dependent transcription of TNF-αand MCP-1/CCL2 genes by preventing RelA from binding its cognate sites on DNA. J. Inflamm. 2010, 7, 59.
- Pollara, J.J.; Laster, S.M.; Petty, I.T. Inhibition of poxvirus growth by Terameprocol, a methylated derivative of nordihydroguaiaretic acid. Antivir. Res. 2010, 88, 287–295.
- Chen, H.; Teng, L.; Li, J.N.; Park, R.; Mold, D.E.; Gnabre, J.; Hwu, J.R.; Tseng, W.N.; Huang, R.C. Antiviral activities of methylated nordihydroguaiaretic acids. 2. Targeting herpes simplex virus replication by the mutation insensitive transcription inhibitor tetra-O-methyl-NDGA. J. Med. Chem. 1998, 41, 3001–3007.
- Gnabre, J.N.; Brady, J.N.; Clanton, D.J.; Ito, Y.; Dittmer, J.; Bates, R.B.; Huang, R.C. Inhibition of human immunodeficiency virus type 1 transcription and replication by DNA sequence-selective plant lignans. Proc. Natl. Acad. Sci. USA 1995, 92, 11239–11243.
- Khanna, N.; Dalby, R.; Tan, M.; Arnold, S.; Stern, J.; Frazer, N. Phase I/II clinical safety studies of terameprocol vaginal ointment. Gynecol. Oncol. 2007, 107, 554–562.
- Gao, Y.; Dong, X.; Kang, T.G. Activity of in vitro anti-influenza virus of arctigenin. Chin. Tradit. Herb. Drugs 2002, 33, 724–725.
- Fu, L.; Xu, P.; Liu, N.; Yang, Z.; Zhang, F.; Hu, Y. Antiviral effect of arctigenin compound on influenza virus. Tradit. Chin. Drug Res. Clin. Pharmacol. 2008, 4.
- Hayashi, K.; Narutaki, K.; Nagaoka, Y.; Hayashi, T.; Uesato, S. Therapeutic effect of arctiin and arctigenin in immunocompetent and immunocompromised mice infected with influenza A virus. Biol. Pharm. Bull. 2010, 33, 1199–1205.
- Schröder, H.C.; Merz, H.; Steffen, R.; Müller, W.E.; Sarin, P.S.; Trumm, S.; Schulz, J.; Eich, E. Differential in vitro anti-HIV activity of natural lignans. Z. Für Nat. 1990, 45, 1215–1221.
- Eich, E.; Pertz, H.; Kaloga, M.; Schulz, J.; Fesen, M.R.; Mazumder, A.; Pommier, Y. -Arctigenin as a lead structure for inhibitors of human immunodeficiency virus type-1 integrase. J. Med. Chem. 1996, 39, 86–95.
- Kuo, Y.C.; Kuo, Y.H.; Lin, Y.L.; Tsai, W.J. Yatein from Chamaecyparis obtusa suppresses herpes simplex virus type 1 replication in HeLa cells by interruption the immediate-early gene expression. Antivir. Res. 2006, 70, 112–120.
- Wang, Y.; Wang, X.; Xiong, Y.; Kaushik, A.C.; Muhammad, J.; Khan, A.; Dai, H.; Wei, D.Q. New strategy for identifying potential natural HIV-1 non-nucleoside reverse transcriptase inhibitors against drug-resistance: An in silico study. J. Biomol. Struct. Dyn. 2019, 30, 1–5.
- Chen, H.; Liu, P.; Zhang, T.; Gao, Y.; Zhang, Y.; Shen, X.; Li, X.; Shen, W. Effects of diphyllin as a novel V-ATPase inhibitor on TE-1 and ECA-109 cells. Oncol. Rep. 2018, 39, 921–928.
- Nesmelova, E.F.; Razakova, D.M.; Akhmedzhanova, V.I.; Bessonova, I.A. Diphyllin from Haplophyllum alberti-regelii, H. bucharicum, and H. perforatum. Chem. Nat. Compd. 1983, 19, 608.
- Sørensen, M.G.; Henriksen, K.; Neutzsky-Wulff, A.V.; Dziegiel, M.; Karsdal, M.A. Diphyllin, a novel and naturally potent V-ATPase inhibitor, abrogates acidification of the osteoclastic resorption lacunae and bone resorption. J. Bone Min. Res. 2007, 22, 1640–1648.
- Martinez-Lopez, A.; Persaud, M.; Chavez, M.P.; Zhang, H.; Rong, L.; Liu, S.; Wang, T.T.; Sarafianos, S.G.; Diaz-Griffero, F. Glycosylated diphyllin as a broad-spectrum antiviral agent against Zika virus. EBioMedicine 2019, 47, 269–283.
- Chen, H.W.; Cheng, J.X.; Liu, M.T.; King, K.; Peng, J.Y.; Zhang, X.Q.; Wang, C.H.; Shresta, S.; Schooley, R.T.; Liu, Y.T. Inhibitory and combinatorial effect of diphyllin, a v-ATPase blocker, on influenza viruses. Antivir. Res. 2013, 99, 371–382.
- Susplugas, S.; Hung, N.V.; Bignon, J.; Thoison, O.; Kruczynski, A.; Sévenet, T.; Guéritte, F. Cytotoxic arylnaphthalene lignans from a Vietnamese acanthaceae, Justicia p atentiflora. J. Nat. Prod 2005, 68, 734–738.
- Zhang, H.J.; Rumschlag-Booms, E.; Guan, Y.F.; Liu, K.L.; Wang, D.Y.; Li, W.F.; Cuong, N.M.; Soejarto, D.D.; Fong, H.H.; Rong, L. Anti-HIV diphyllin glycosides from Justicia gendarussa. Phytochemistry 2017, 136, 94–100.
- Yang, Z.; Wang, Y.; Zheng, Z.; Zhao, S.; Zhao, J.I.; Lin, Q.; Li, C.; Zhu, Q.; Zhong, N. Antiviral activity of Isatis indigotica root-derived clemastanin B against human and avian influenza A and B viruses in vitro. Int. J. Mol. Med. 2013, 31, 867–873.
- Liu, G.T. Bicyclol: A novel drug for treating chronic viral hepatitis B and C. Med. Chem. 2009, 5, 29–43. Available online: (accessed on 12 July 2020).
- Zhang, J.T. New drugs derived from medicinal plants. Therapie 2002, 57, 137–150.
- Ruan, B.; Wang, J.W.; Bai, X.L. Comparison of bicyclol therapy for patients with genotype B and C of hepatitis B virus. Zhonghua shi yan he lin chuang bing du xue za zhi= Zhonghua shiyan he linchuang bingduxue zazhi = Chin. J. Exp. Clin. Virol. 2007, 21, 366–368.
- Liu, C.H.; Jassey, A.; Hsu, H.Y.; Lin, L.T. Antiviral activities of silymarin and derivatives. Molecules 2019, 24, 1552.
- Song, J.H.; Choi, H.J. Silymarin efficacy against influenza A virus replication. Phytomedicine 2011, 18, 832–835.
- Cui, Q.; Du, R.; Liu, M.; Rong, L. Lignans and their derivatives from plants as antivirals. Molecules 2020, 25, 183.
- Wen, C.C.; Kuo, Y.H.; Jan, J.T.; Liang, P.H.; Wang, S.Y.; Liu, H.G.; Lee, C.K.; Chang, S.T.; Kuo, C.J.; Lee, S.S.; et al. Specific plant terpenoids and lignoids possess potent antiviral activities against severe acute respiratory syndrome coronavirus. J. Med. Chem. 2007, 50, 4087–4095.
- Vilhelmova-Ilieva, N.; Galabov, A.S.; Mileva, M. Tannins as antiviral agents. Tannins-structural properties, biological properties and current knowledge. Alfredo Aires 2019.
- Yang, C.M.; Cheng, H.Y.; Lin, T.C.; Chiang, L.C.; Lin, C.C. The in vitro activity of geraniin and 1,3,4,6-tetra-O-galloyl-β-d-glucose isolated from Phyllanthus urinaria against herpes simplex virus type 1 and type 2 infection. J. Ethnopharmacol. 2007, 110, 555–558.
- Notka, F.; Meier, G.; Wagner, R. Concerted inhibitory activities of on HIV replication In vitro and ex vivo. Antivir. Res. 2004, 64, 93–102.
- Lin, L.T.; Chen, T.Y.; Chung, C.Y.; Noyce, R.S.; Grindley, T.B.; McCormick, C.; Lin, T.C.; Wang, G.H.; Lin, C.C.; Richardson, C.D. Hydrolyzable tannins (chebulagic acid and punicalagin) target viral glycoprotein-glycosaminoglycan interactions to inhibit herpes simplex virus 1 entry and cell-to-cell spread. J. Virol. 2011, 85, 4386–4398.
- Vilhelmova, N.; Jacquet, R.; Quideau, S.; Stoyanova, A.; Galabov, A.S. Three-dimensional analysis of combination effect of ellagitannins and acyclovir on herpes simplex virus types 1 and 2. Antivir. Res. 2011, 89, 174–181.
- Vilhelmova-Ilieva, N.; Jacquet, R.; Quideau, S.; Galabov, A.S. Ellagitannins as synergists of ACV on the replication of ACV-resistant strains of HSV 1 and 2. Antivir. Res. 2014, 110, 104–114.
- Vilhelmova-Ilieva, N.; Sirakov, I.; Jacquet, R.; Deffieux, D.; Quideau, S.; Galabov, A.S. Antiviral activities of ellagitannins against bovine herpesvirus 1, suid alphaherpesvirus 1 and caprine herpesvirus 1. J. Vet. Med. Anim. Health 2020, 12, 139–143.
- Vilhelmova-Ilieva, N.; Deffieux, D.; Quideau, S. Castalagin: Some aspects of the mode of anti-herpes virus activity. Ann. Antivir. Antiretrovir. 2018, 2, 004–007.
- Wahyuni, T.S.; Azmi, D.Z.; Permanasari, A.; Adianti, M.; Lydia, T.; Widiandani, T.; Aoki, U.C.; Widyawaruyanti, A.; Fuad, A.; Hak, H. Anti-viral activity of Phyllanthus niruri against hepatitis c virus. Malays. Appl. Biol. 2019, 48, 105–111.
- Dhama, K.; Karthik, K.; Khandia, R.; Chakraborty, S.; Munjal, A.; Latheef, S.K.; Kumar, D.; Ramakrishnan, M.A.; Malik, Y.S.; Singh, R.; et al. Advances in designing and developing vaccines, drugs, and therapies to counter Ebola virus. Front. Immunol. 2018, 9, 1803.
- Munjal, A.; Khandia, R.; Dhama, K.; Sachan, S.; Karthik, K.; Tiwari, R.; Malik, Y.S.; Kumar, D.; Singh, R.K.; Iqbal, H.M.N.; et al. Advances in developing therapies to combat Zika virus: Current knowledge and future perspectives. Front. Microbiol. 2017, 8, 1469.
- Singh, R.K.; Dhama, K.; Chakraborty, S.; Tiwari, R.; Natesan, S.; Khandia, R.; Munjal, A.; Vora, K.S.; Latheef, S.K.; Karthik, K.; et al. Nipah virus: Epidemiology, pathology, immunobiology and advances in diagnosis, vaccine designing and control strategies—A comprehensive review. Vet. Q. 2019, 39, 26–55.
- Li, Y.; Liu, X.; Guo, L.; Li, J.; Zhong, D.; Zhang, Y.; Clarke, M.; Jin, R. Traditional Chinese herbal medicine for treating novel coronavirus (COVID-19) pneumonia: Protocol for a systematic review and meta-analysis. Syst. Rev. 2020, 9, 75.
- Chen, L.; Hu, C.; Hood, M.; Zhang, X.; Zhang, L.; Kan, J.; Du, J. A novel combination of vitamin C, curcumin and glycyrrhizic acid potentially regulates immune and inflammatory response associated with coronavirus infections: A perspective from system biology analysis. Nutrients 2020, 12, 1193.
- Dhama, K.; Sharun, K.; Tiwari, R.; Dadar, M.; Malik, Y.S.; Singh, K.P.; Chaicumpa, W. COVID-19, an emerging coronavirus infection: Advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum. Vaccin Immunother. 2020, 16, 1232–1238.
- Gangal, N.; Nagle, V.; Pawar, Y.; Dasgupta, S. Reconsidering traditional medicinal plants to combat COVID-19. AIJR 2020. Available online: (accessed on 24 August 2020).
- Malik, Y.S.; Kumar, N.; Sircar, S.; Kaushik, R.; Bhat, S.; Dhama, K.; Gupta, P.; Goyal, K.; Singh, M.P.; Ghoshal, U.; et al. Coronavirus disease pandemic (COVID-19): Challenges and a global perspective. Pathogens 2020, 9, E519.
- Rastogi, S.; Pandey, D.N.; Singh, R.H. COVID-19 Pandemic: A pragmatic plan for Ayurveda intervention. J. Ayurveda Integr. Med. 2020.
- Vellingiri, B.; Jayaramayya, K.; Iyer, M.; Narayanasamy, A.; Govindasamy, V.; Giridharan, B.; Ganesan, S.; Venugopal, A.; Venkatesan, D.; Ganesan, H.; et al. COVID-19: A promising cure for the global panic. Sci. Total Environ. 2020, 725, 138277.
- Yang, Y.; Islam, M.S.; Wang, J.; Li, Y.; Chen, X. Traditional Chinese medicine in the treatment of patients infected with 2019-new coronavirus (SARS-CoV-2): A review and perspective. Int J. Biol. Sci. 2020, 16, 1708–1717.
- Yatoo, M.I.; Hamid, Z.; Parray, O.R.; Wani, A.H.; Ul Haq, A.; Saxena, A.; Patel, S.K.; Pathak, M.; Tiwari, R.; Malik, Y.S.; et al. COVID-19—Recent advancements in identifying novel vaccine candidates and current status of upcoming SARS-CoV-2 vaccines. Hum. Vaccin Immunother. 2020, 1–14.
- Dhama, K.; Chakraborty, S.; Tiwari, R.; Verma, A.K.; Saminathan, M.; Amarpal, Y.M.; Nikousefat, Z.; Javdani, M.; Khan, R.U. A concept paper on novel technologies boosting production and safeguarding health of humans and animals. Res. Opin. Anim. Vet. Sci. 2014, 4, 353–370.
- Abd El-Hack, M.E.; Alagawany, M.; Farag, M.R.; Arif, M.; Emam, M.; Dhama, K.; Sarwar, M.; Sayab, M. Nutritional and pharmaceutical applications of nanotechnology: Trends and advances. Int. J. Pharm. 2017, 13, 340–350.
- Prasad, M.; Lambe, U.P.; Brar, B.; Shah, I.; Manimegalai, J.; Ranjan, K.; Rao, R.; Kumar, S.; Mahant, S.; Khurana, S.K.; et al. Nanotherapeutics: An insight into healthcare and multi-dimensional applications in medical sector of the modern world. Biomed. Pharm. 2018, 97, 1521–1537.
- Borkotoky, S.; Banerjee, M. A computational prediction of SARS-CoV-2 structural protein inhibitors from Azadirachta indica (Neem). J. Biomol. Struct. Dyn. 2020, 1–7.
- Manoharan, Y.; Haridas, V.; Vasanthakumar, K.C.; Muthu, S.; Thavoorullah, F.F.; Shetty, P. Curcumin: A wonder drug as a preventive measure for COVID19 management. Indian J. Clin. Biochem. 2020, 35, 373–375.
- Zahedipour, F.; Hosseini, S.A.; Sathyapalan, T.; Majeed, M.; Jamialahmadi, T.; Al-Rasadi, K.; Banach, M.; Sahebkar, A. Potential effects of curcumin in the treatment of COVID-19 infection. Phytother. Res. 2020, 34, 2911–2920.
- Straughn, A.R.; Kakar, S.S. Withaferin A: A potential therapeutic agent against COVID-19 infection. J. Ovarian Res. 2020, 13, 1–5.
- Pandey, P.; Khan, F.; Kumar, A.; Srivastava, A. Screening of potent inhibitors against 2019 novel coronavirus (Covid-19) from Allium sativum and Allium cepa: An in silico approach. Biointerface Res. Appl. Chem. 2020, 11, 7981–7993.
- Meireles, D.; Gomes, J.; Lopes, L.; Hinzmann, M.; Machado, J. A review of properties, nutritional and pharmaceutical applications of Moringa oleifera: Integrative approach on conventional and traditional Asian medicine. Adv. Tradit. Med. 2020, 17, 1–21.
