1. An anterior cruciate ligament injury
An anterior cruciate ligament injury (ACL) is considered one of the most significant and debilitating injuries an athlete can experience, with an abundance of negative economic [
1,
2,
3], psychological [
1,
4], and health [
1,
5] implications. ACL injury risk factors are multifactorial (anatomical, hormonal, biomechanical, neuromuscular, environmental) [
1,
6] and a complex interaction of both internal (within the body) and external (outside the body) factors [
6,
7,
8]. In simplistic terms, ACL injuries occur when a catastrophic applied load exceeds the ligament’s tolerance [
7,
9], or due to a “fatigue failure” mechanism whereby the accumulation of high magnitudes and repetitive cycles of knee joint loading [
10,
11,
12,
13,
14]. This process, without adequate rest and repair, can lead to micro damage and subsequent ACL failure [
13] from mechanical loads which previously could be tolerated [
14,
15,
16]. Mitigating ACL injury risk therefore is considered highly important in sports medicine and science environments.
Non-contact ACL injuries generally occur during high-impact tasks such as change of directions (COD) (side-step, cut or turn, plant-and-cut manoeuvres) [
17,
18,
19,
20,
21,
22,
23,
24,
25,
26], landing (predominantly single-leg weight bearing) [
17,
19,
21,
25,
27], and deceleration actions [
20,
21,
28]; attributable to the potential generation of high multiplanar knee joint loading (flexion, rotation, abduction and translatory moments) during foot contact [
29,
30,
31,
32,
33], thus increasing ACL strain [
34,
35,
36,
37,
38]. These multiplanar knee joint loads are often used as surrogates of non-contact ACL injury risk [
29,
32,
39,
40], and are amplified during COD, landings, and decelerations when aberrant and “high-risk” neuromuscular control and biomechanical deficits are displayed (e.g., lateral trunk flexion, knee valgus, etc.) [
1,
31,
32,
33,
41,
42,
43]. Importantly, neuromuscular control and biomechanical deficits are modifiable through appropriate training and conditioning [
31,
32,
33,
41,
42,
44,
45], which may reduce knee joint loading during high-impact actions and subsequent risk of non-contact ACL injury [
1,
43,
44,
45,
46]. As such, the mechanism of ACL injury, from a knee joint loading perspective, has been stated as “multiplanar” [
6]; highlighting the importance of reducing multiplanar joint loading during high-risk activities to mitigate ACL injury risk [
9,
47,
48].
2. Qualitative Screening: Why Assess Cutting Movement Quality?
Due to the plethora of negative implications associated with non-contact ACL injury, being able to profile and classify athletes as potentially “high-risk” of injury is a crucial process in ACL injury mitigation [
1,
49]. Side-step cutting (lateral foot plant) is an important high-intensity action performed in numerous sports, and is a pivotal action performed to evade opponents, penetrate defensive lines and gain territorial advantage in sports such as rugby, American football, and handball [
50,
51,
52,
53,
54]. However, because side-steps are frequently performed movements in sports [
50,
51,
52,
53], and performed at high-intensity, and thus have the potential to generate high impact forces and knee joint loads [
31,
33,
55], they are also commonly observed manoeuvres during non-contact ACL injury events [
17,
18,
19,
20,
21,
22,
23,
24,
25,
26]. For example, 60–67% of non-contact ACL injuries in rugby [
18], American football [
26], and handball [
19] occur during side-step cutting, while this manoeuvre is also linked with non-contact ACL injury events in soccer [
17], badminton [
25], and Australian rules football [
21]. Consequently, screening tools and field-based interventions that can assist in ACL injury risk mitigation is of great interest, particularly for practitioners working in sports where cutting is the predominant mechanism of non-contact ACL injury.
The ability to predict non-contact ACL injury using screening tools is a contentious issue [
56,
57,
58]; however, much attention has been placed on screening and profiling movement quality because of the adaptable nature of movement biomechanics, which in turn is a modifiable ACL risk factor [
1,
43,
45,
57,
59]. Additionally, creating “injury-risk profiles” through the identification of “high-risk” biomechanical and neuromuscular control deficits is considered important in terms quantifying relative injury risk [
59,
60,
61]. For example, “high-risk” postures include knee abduction angles (KAA–synonymous with knee valgus angles) [
33,
40,
42,
62,
63], lateral trunk flexion [
31,
42,
64,
65,
66], extended knee postures [
24,
67,
68], and hip internal rotation [
40,
41,
63,
69] are related to greater multiplanar knee joint loads and subsequent ACL loading [
46,
70,
71].
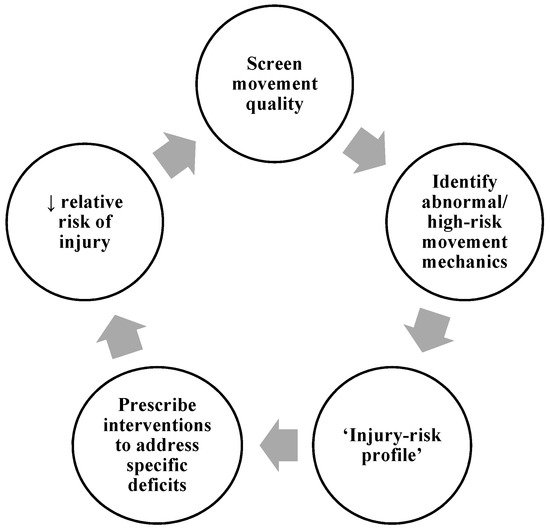
displays the screening process commonly adopted by practitioners, whereby athletes are typically screened/profiled during a movement to assess their movement quality, joint kinetics, or kinematics against pre-determined criteria or benchmarks. This can be done via three-dimensional (3D) motion and ground reaction force (GRF) analysis whereby joint kinetics and kinematics can be examined and surrogates of injury risk are measured, creating an “injury-risk profile”, and subsequently used to infer potential injury risk. For example, peak KAMs and peak KAAs can be measured during a COD or a drop landing to identify athletes who display values greater than normative data or a threshold to define “high-risk” [
39,
72,
73]. Alternatively, qualitative screening of movement quality may take place using high-speed two-dimensional (2D) cameras, whereby movement is filmed (usually in the frontal and sagittal plane) and aberrant and “high-risk” movement patterns can be identified via visual observations (i.e., visible knee valgus/lateral trunk flexion). Qualitative assessments have been shown to reflect aspects of performance during 3D motion analysis, such as the Landing Error Scoring System (LESS) [
74] and Qualitative Analysis of Single Leg Loading (QASLS) [
75].
Figure 1. Screening movement quality process.
Irrespective of the screening method, athletes identified as potentially “higher-risk” of injury can therefore be prescribed individualised interventions to address the specific “high-risk” deficits [
57,
59]. This should theoretically reduce injury risk, and the training intervention’s success is monitored be re-evaluating and screening movement quality at the end of the intervention. Practitioners may continuously go through the process multiple times (normally at the end of mesocycles) during the macrocycle. Therefore, validated and reliable screening tools which assess movement quality are considered integral for practitioners working in strength and conditioning, sports medicine, and sports rehabilitation [
59,
76].
The optimal method for assessing movement kinetics and kinematics is 3D and GRF analysis [
1,
57], whereby this approach is used to identify “high-risk” athletes that display poor movement quality (i.e., knee valgus) and high multiplanar knee joint moments (surrogates of non-contact ACL injury risk) [
59]. Although insightful and can indeed provide detailed insight into athletes’ movement strategies and surrogates of injury risk, 3D motion and GRF analysis does have its limitations including, cost, complexity, the time required to perform mass screening, and the required laboratory facilities [
1,
57,
72,
77,
78,
79]; thus, restricting its use for practitioners in field-based environments. As such, qualitative screening tools such as the LESS [
74,
80], Tuck Jump Assessment (TJA) [
81,
82,
83], and QASLS [
84,
85] have been developed, offering practitioners an easier and cost-effective method to evaluate aberrant movement quality and postures associated with greater ACL injury risk, typically during landing tasks. Although screening landing mechanics during vertical orientated tasks is indeed applicable for jump-landing sports where the landing is the predominant action associated with non-contact ACL injury [
27,
28,
86,
87], changing direction is a unilateral and multiplanar movement which is biomechanically distinctly different to landing, thus screening landing lacks specificity to directional changes [
57,
60,
76]. This is pertinent for practitioners who seek to profile athletes who participate in sports (handball, American football, rugby, and soccer) where the side-step cutting is a predominant mechanism of non-contact ACL injury [
17,
18,
19,
20,
21,
22,
23,
24,
25,
26]. Furthermore, mixed findings have been observed between “high-risk” postures and knee joint loads between landing and cutting tasks [
72,
88,
89,
90], with researchers demonstrating that “injury-risk profiles” are task dependent [
72,
91,
92]. Therefore, it would be more suitable to assess movement mechanics associated with the primary action of injury in that sport [
49,
57,
60]. As such, there is a requirement for a specific field-based qualitative screening tool to evaluate and identify poor movement quality and “high-risk” mechanics specifically for cutting.
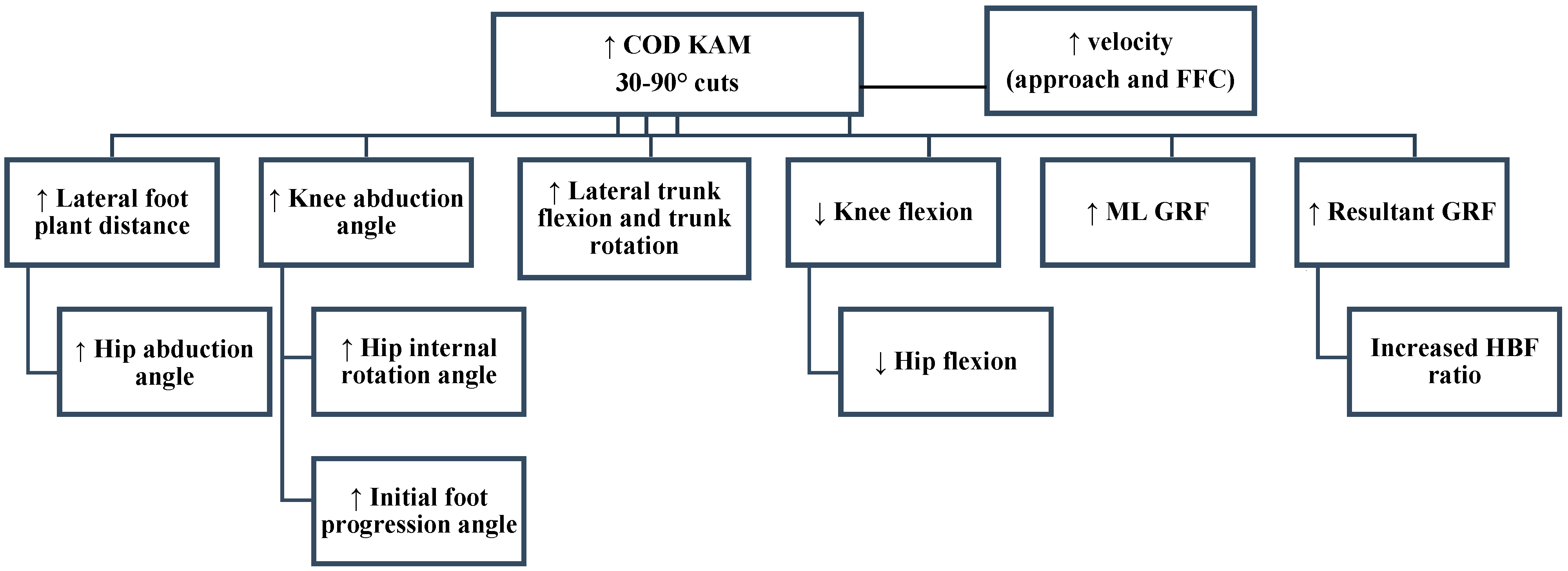
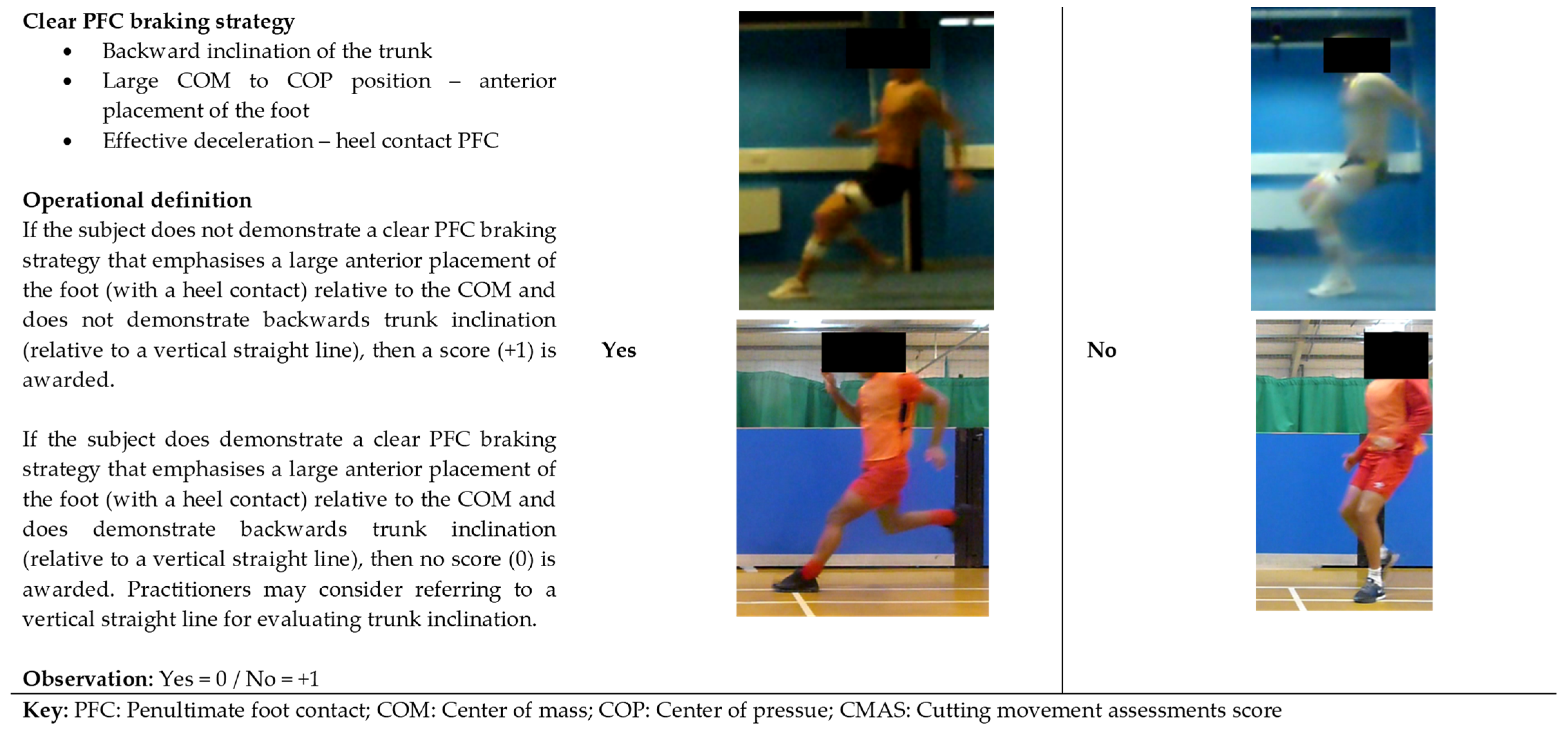
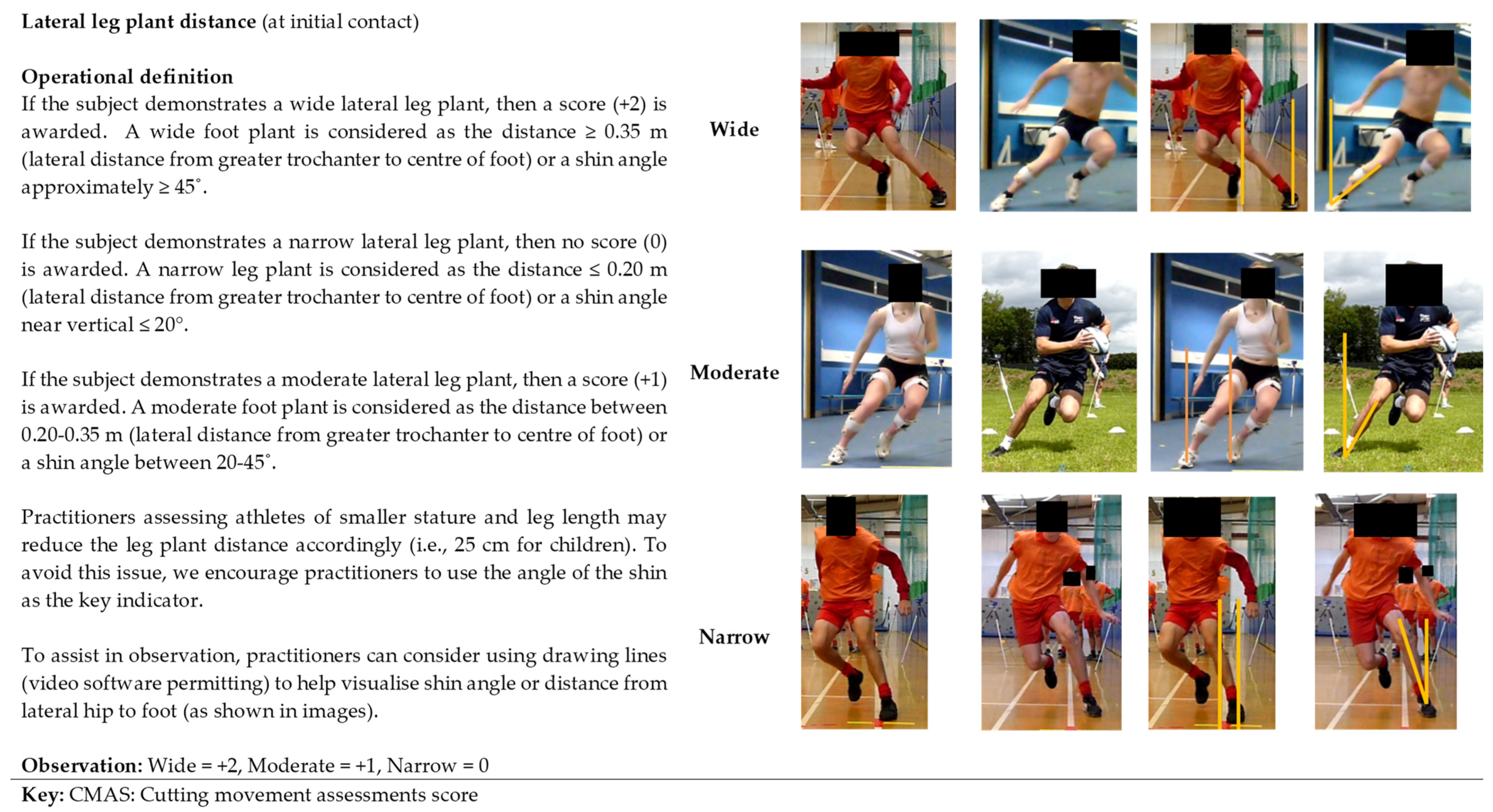
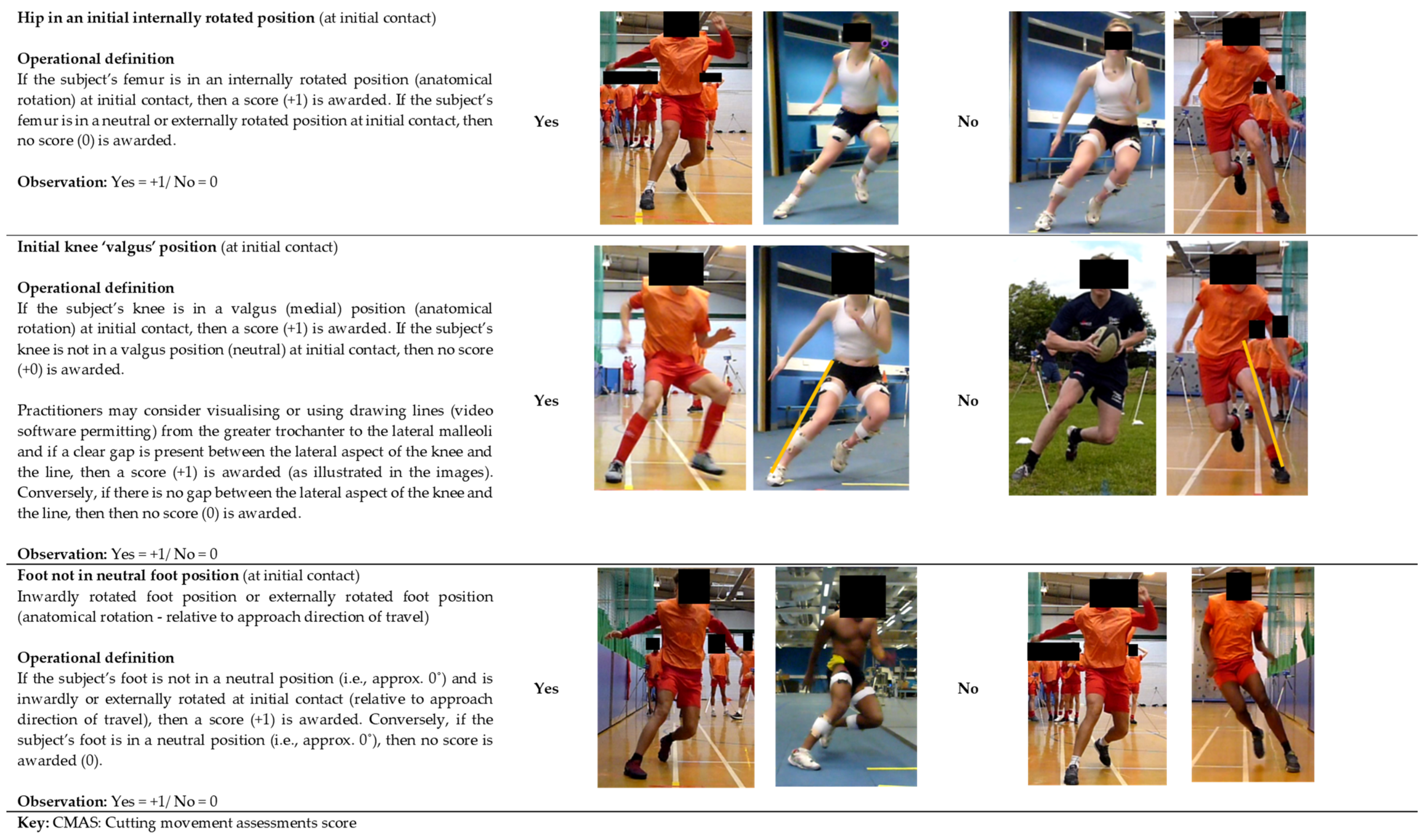
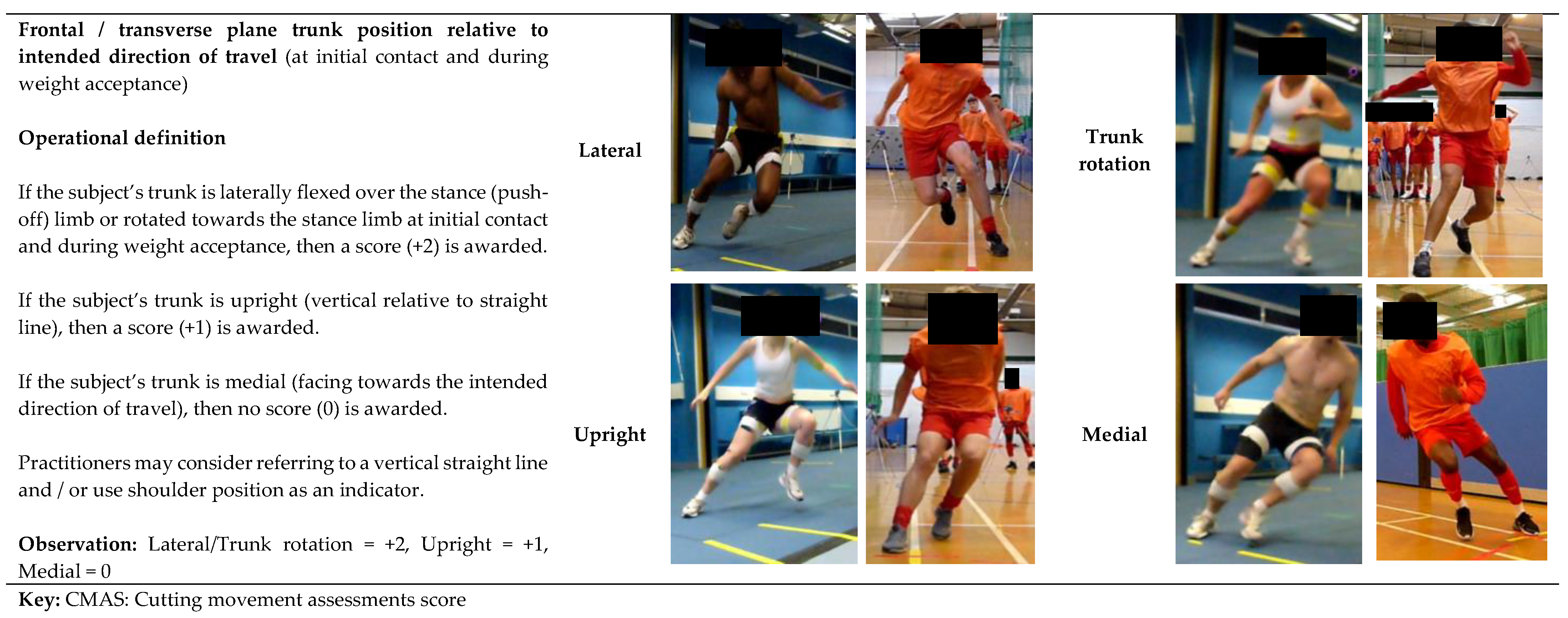
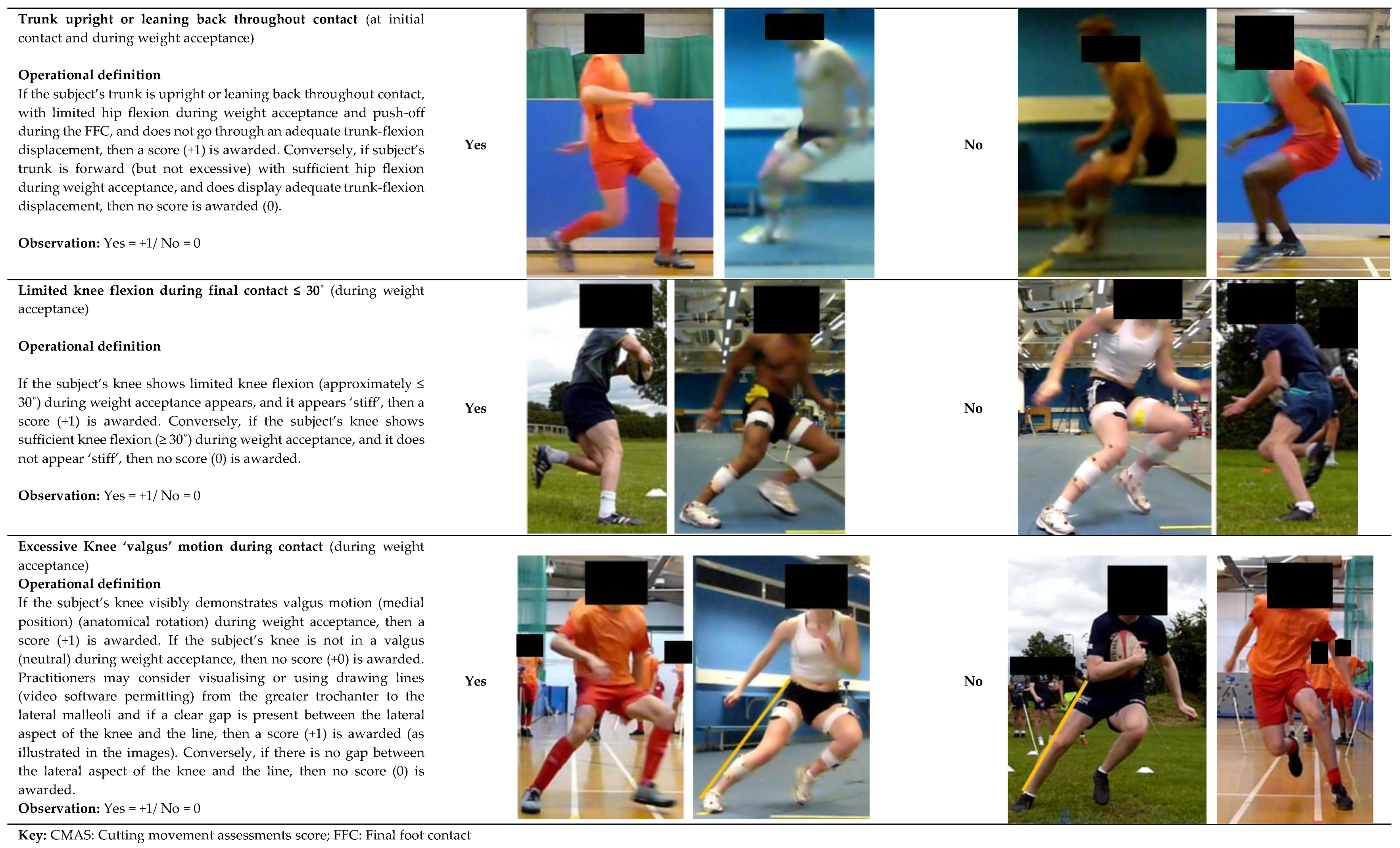
3. Introducing the Cutting Movement Assessment Score (CMAS)
The CMAS, initially developed and validated in 2017 [
76], is a 9-item qualitative screening tool () that assesses hip, knee, foot, and trunk postures during side-step cutting relating to the technical determinants of peak KAMs [
30,
31,
33,
40,
41,
42,
63,
64,
65,
68,
69,
93] () and non-contact ACL injury visual observations [
19,
24,
26]. A detailed rationale and operational definitions for these items are presented in a later section, but briefly these items relate to penultimate foot contact (PFC) braking strategy, and trunk, hip, knee, and foot postures and motions during the final “plant” step (). The CMAS involves filming athletes (ideally ≥100 Hz) during a side-step cutting task (30–90°) using cameras placed approximately at hip height in the sagittal plane, frontal plane, and if possible with an additional camera 20–45° relative to the cut. Video footage is retrospectively viewed in video analysis software, and the athlete’s cutting trial is screened using the CMAS screening tool. The majority (7-items) of the CMAS criteria follow a dichotomous scale (yes or no), with lateral leg plant distance and frontal/transverse plane trunk positioning involving a description classification, with 3 and 4 possible descriptors, respectively (). Athletes are awarded a score if they display any of the items of the CMAS criteria (), and greater scores are typically indicative of suboptimal technique and greater peak KAMs [
55,
76].
Figure 2. Knee abduction moment (KAM) deterministic model. Adapted from [
93]; GRF: Ground reaction force; COD: Change of direction; ML: Medial-lateral; HBF: Horizontal braking force; FFC: Final foot contact.
Table 1. Cutting Movement Assessment Score Tool (CMAS).
In the preliminary validation study by Jones et al. [
76], using 3D motion and two 2D cameras (30 Hz) to record video data for qualitative screening, a strong association between CMAS and peak KAM (
ρ = 0.633;
p < 0.001) was demonstrated during a 60–90° cut. More recently, Dos’Santos [
55] expanded on the preliminary study by investigating a greater sample size (41 vs. 8), using an extra camera placed 45° to the cut at a higher sampling rate (100 Hz vs. 30 Hz), and also slightly modified the CMAS (provided extra details) details to the CMAS screening tool. Substantiating the preliminary findings [
76], a very large (
ρ = 0.796,
p < 0.001) relationship was observed between CMAS and peak KAM for participant average data [
55]. In addition, athletes were divided into high (~7) and low (~3) CMAS groups (top 33% and bottom 33%), where cutting kinetics and kinematics were compared. Importantly, athletes with higher CMASs demonstrated “higher-risk” postures and knee joint loads connected with ACL injury risk compared to athletes with lower CMASs. These included significantly (moderate to very large effect sizes) greater mean vertical braking forces, greater peak KAAs, greater initial foot progression angles, greater lateral foot plant distances, and greater knee flexion (KFM), knee internal rotation (KIRM), and KAMs [
55].
Later analysis in the study by Dos’Santos et al. [
55], revealed that when statistical analysis was performed for all pooled trials, female trials, and male trials, large, large, and very large associations were observed between CMAS and peak KAMs (
Supplementary Materials), respectively [
93]. Additionally, in terms of cutting mechanics, greater peak and mean vertical braking forces, greater peak and initial KAAs, and lower peak knee flexion angle and range of motion, greater initial foot progression angles, greater lateral trunk flexion, greater lateral foot plant distances, and greater multiplanar knee joint moments were displayed during trials with higher CMASs (≥7) compared to lower CMASs (≤3) [
93]. To the best of our knowledge, the LESS is the only other qualitative screening tool that has been validated against the gold standard of 3D motion analysis with respect to knee joint moments [
74] and subsequent surrogates of ACL injury risk. Thus, the CMAS would appear to have validity and be a rigorous enough method to potentially identify athletes who generate high peak KAMs (and multiplanar knee joint loads) and potential ACL injury risk. This method requires only three high-speed cameras and video analysis software (which in most cases is free), which is a cost- and time-effective alternative to 3D motion analysis, and is a field-based method for practitioners.
4. CMAS Methodological Procedures
The CMAS is applicable to side-step cuts of 30–90° with published literature using the CMAS during 60–90° [
76], 70° [
94], and 90° cuts [
55], and in unpublished observations, we have also used the CMAS during 45° cuts. Ideally, CMAS screening should take place on the same surface that the athlete performs their sport on (e.g., court, synthetic field-turf, grass) and where possible athletes should wear sport-specific footwear to improve ecological validity [
95,
96,
97]. If athletes hold an implement in their sport (e.g., ball or racket), practitioners may consider screening cutting trials where athletes hold the implement to improve ecological validity. Anecdotally, we have had a positive experience screening ball-carrying 45° cutting in rugby union players. Nevertheless, it is advised that athletes tuck-in loose clothing, and ideally wear tight fitting clothing to make it easier to screen and observe movement quality and postures. Although the aim of the CMAS is to profile movement quality, practitioners may consider assessing performance using timing gates positioned at a start and finish line to obtain cutting completion time to monitor and standardise performance.
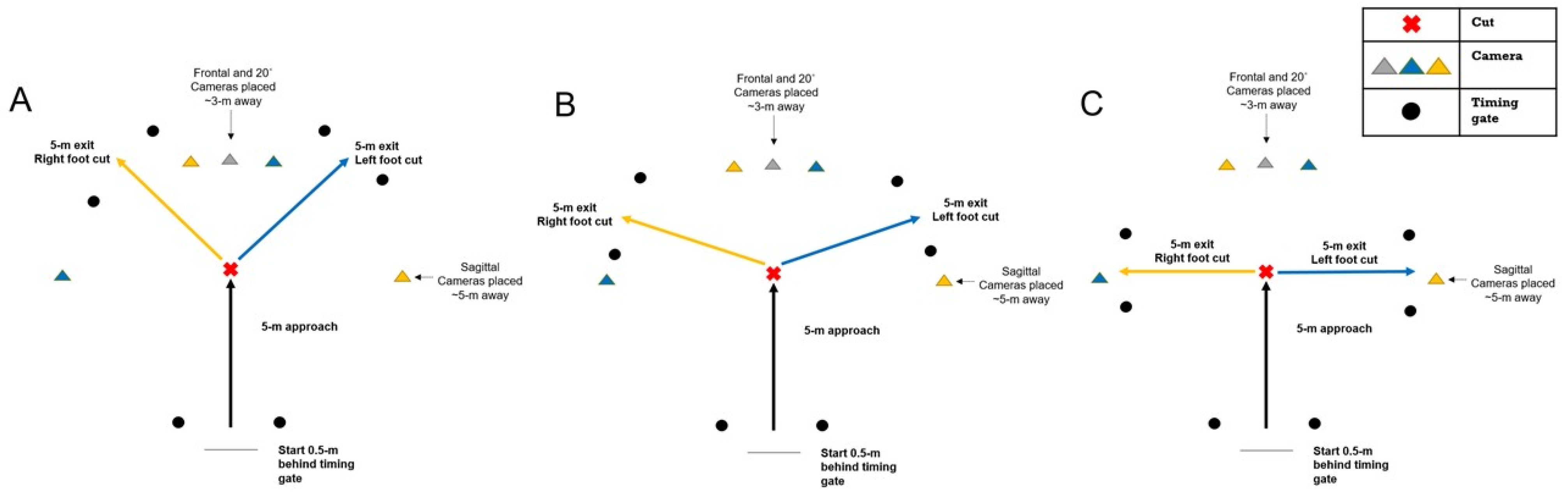
provides a schematic representation of the CMAS for administering during 45°, 70°, and 90° cuts. As a minimum recommendation, practitioners are encouraged to use 2 high-speed cameras for qualitative screening positioned on tripods placed at approximate hip height at least 3 metres away in the frontal plane and 5 metres away in the sagittal plane away from the cutting zone. However, to accommodate athletes who pre-rotate during the cut, and to reduce parallax error, practitioners are strongly encouraged to position an additional camera 20–45° to the cut to assist in more accurate qualitative screening. Although published research placed the third camera at 45° [
55,
94], we have recently had better observations of CMAS trials with a camera positioned at 20°. This approach has tended to reduce parallax error because the subjects who pre-rotate are more perpendicular to the 20° camera in contrast to 45° camera observations. As such, this has made subsequent screening of relevant criteria easier and is therefore our preferred method going forward. As previously stated, practitioners should ideally use high-speed cameras for qualitative screening, sampling at a minimum 100 Hz. Access to high-speed cameras for practitioners is becoming increasingly accessible as most smartphone and tablet technology have high-speed cameras as default features. Nonetheless, when using high-speed cameras for the CMAS, practitioners should ensure that there is sufficient lighting to permit accurate qualitative screening.
Figure 3. Schematic representation of the CMAS protocol. (A): 45° cut; (B): 70° cut; (C): 90° cut. Yellow cameras indicate camera placement for right foot cuts, blue cameras indicate camera placement for left foot cuts, grey camera used for both left and right cuts.
It is encouraged that practitioners evaluate 2–3 cutting trials per limb for each athlete during the cutting trials, typically during a cut which contains a 5-m entry and exit. However, practitioners are free to adjust entry and exit distances at their own discretion in context of their populations’ sporting demands. From our experience, we have been able to collect CMAS video footage (along with completion times) for 6 trials (3 trials per limb) in groups of athletes as large 12 in less than 15 min, highlighting the simplicity and application for large mass screening in contract to 3D motion analysis.
Once video footage data are collected, video footage should ideally be viewed in a software which enables videos to be played at various speeds, frame-by-frame, while a software which can open multiple video windows, create photo-sequences, and also contains drawing tools is also advantageous. We have used Kinovea software (0.8.15 for Windows, Bordeaux, France), which is free, and we have found this software to be more than adequate for qualitative screening purposes; however, practitioners are free to select an alternative video software at their own discretion. From our experience, qualitative screening of one trial takes ~3 min. However, given the subjective nature of qualitative screening, it is strongly encouraged that practitioners within sports science, sports medicine, and clinical departments are familiar and adequately trained using the CMAS and other qualitative screening tools. This is to ensure that high levels of intra- and inter-rater reliability are obtained, and more importantly so that the athlete obtains accurate, consistent, and reliable evaluations [
57,
58]. By this, it is strongly encouraged that practitioners within their departments perform their own in-house training and collect pilot video footage where they discuss and agree on “low-risk” and “high-risk” movement patterns. These should be consensually agreed by all coaches, practitioners, and potential raters within the department, team, or institution. Practitioners unfamiliar with the CMAS may consider receiving training and education from practitioners’ experienced in qualitative screening and knowledgeable in COD biomechanics. We have had recent success whereby the lead researcher has facilitated a one hour-training session and created manuals for raters outlining how to grade the cutting trials using the CMAS, and to establish and uniformly agree on “low-risk” and “high-risk” movement patterns. Subsequently we have observed high levels of intra- and inter-rater reliability [
55,
76,
94].
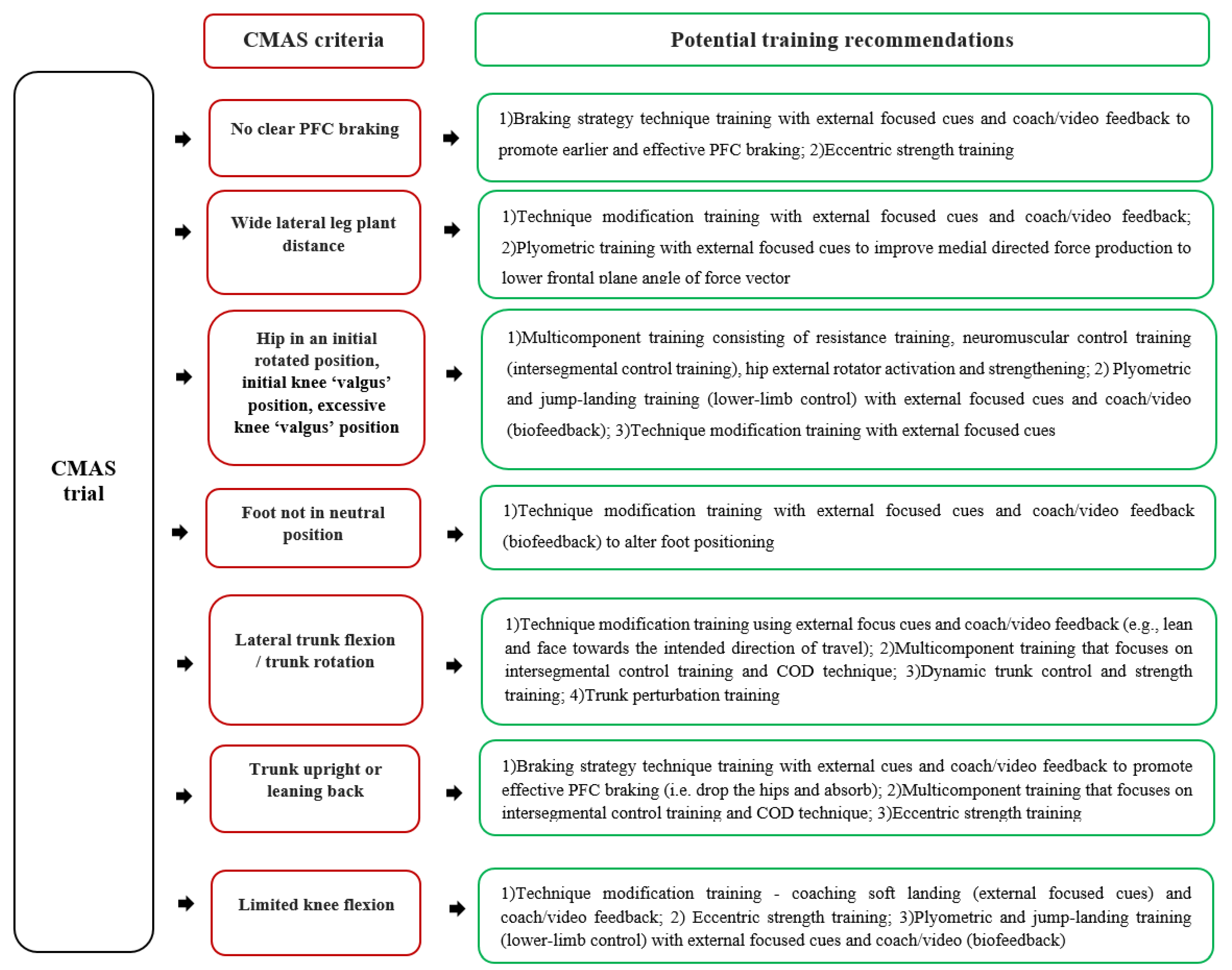
6. Practical Applications: Interpreting CMAS Score and the CMAS Training Recommendations Decision Tree
As strong relationships between CMAS and peak KAMs have been observed [
55,
76,
93], a higher total score is generally indicative of suboptimal technique and greater non-contact ACL injury risk. Additionally, “higher-risk” cutting postures connected with ACL injury risk were demonstrated by participants and trials with “high” CMASs (~7) compared to participants and trials with “low” CMASs (~3) [
55,
93]. As such, practitioners can use scores of ≥7, 4–6, and ≤3 as initial benchmarks to classify athletes with high, moderate, and low CMASs [
55,
93], respectively. However, practitioners should note that suboptimal and unsafe technique may still be displayed during trials with low CMASs; therefore, it is advised to focus on the CMAS criteria where athletes scored deficits [
57,
76]. For example, an athlete with a low CMAS may still display “high-risk” cutting deficits, such as knee valgus, lateral trunk flexion, limited knee flexion, or hip internal rotation. Therefore, in this scenario, the athlete would still warrant specific injury risk mitigation training and conditioning. In addition, it is worth noting that some CMAS criteria are associated with faster performance [
41,
43,
67,
70]. For instance, a wide lateral leg plant is displayed to generate greater medio-lateral propulsive forces and subsequent exit velocity [
41,
42], while reduced knee flexion is associated with shorter ground contact time [
43,
67]. Thus, practitioners must be mindful and acknowledge the trade-off between knee joint loading (injury risk) and performance when screening and modifying cutting mechanics.
A low CMAS score generally indicates an ability to performance a cutting task well against the prescribed CMAS criteria, in a closed, controlled environment. Further work is needed to assess both scoring during tasks in a sport-specific, open skill environment to determine if performance transitions (scores) to these environments. Additionally, it is worth highlighting that the CMAS is based on postures associated with ACL injury risk, but the CMAS is indicating relative risk of injury and we are by no means are stating that athletes with greater scores will definitely sustain an ACL injury. Nevertheless, practitioners are recommended to use the CMAS as a regular monitoring tool to assist in identifying “high-risk” cutting deficits in their athletes. This can be used to inform and help develop individualised training programmes to modify the specific deficits and mitigate potential ACL injury risk [
59,
60,
140]. Readers are encouraged to read specific reviews regarding training strategies to mitigate non-contact ACL injury [
45,
46,
48,
141,
142]; thus, a brief overview is presented in the CMAS training recommendations decision tree ().
Figure 9. CMAS training recommendations decision tree adapted from previous research [
45,
46,
48,
141,
142].