Chronic thromboembolic pulmonary hypertension (CTEPH) is a specific type of pulmonary hypertension (PH) and the major component of Group 4 pulmonary hypertension (PH).
- chronic thromboembolic pulmonary hypertension
1. Introduction
The 6th world symposium on pulmonary hypertension (PH) in 2018 has defined PH as an elevated mean pulmonary artery pressure (mPAP) ≥ 20 mmHg at rest, pulmonary capillary wedge pressure < 15 mmHg, and pulmonary vascular resistance (PVR) ≥ 3 Wood Unit (WU) [1]. PH can be further subdivided into 5 groups (Table 1).Table 1. Different groups of pulmonary hypertension. Left column indicates group of pulmonary hypertension and right column shows the entity included.
| Group 1 | Pulmonary Arterial Hypertension (PAH) |
| Group 2 | Due to Left Heart Disease |
| Group 3 | Due to Chronic Lung Disease/Hypoxemia |
| Group 4 | Due to Pulmonary Arterial Obstructions |
| Group 5 | Multifactorial |
Chronic thromboembolic pulmonary hypertension (CTEPH) belongs to Group 4 of the PH classification. CTEPH is defined as an obstruction of the pulmonary arterial vasculature secondary to single or recurrent episodes of pulmonary embolism (PE) [2]. It is a distinct and infrequently diagnosed entity of PH that is progressive and can be fatal if left untreated.
2. Epidemiology
CTEPH occurs in a minority of the patients who fail to restore normal pulmonary perfusion after single or recurrent episodes of PE. It generally develops within the first year after PE and is an uncommon occurrence after about 2 years of an episode of PE [2]. The exact incidence of CTEPH is difficult to determine but it is estimated to be prevalent in around 0.5–5% of patients that have an acute PE [3][4][5][6]. It has been reported in as many as 11.6% of patients with a history of recurrent PE [7] (Table 2).Table 2. Studies estimating incidences of chronic thromboembolic pulmonary (CTEPH) after pulmonary embolism (PE).
Determining an accurate incidence of CTEPH after PE is challenging because of inconsistencies in reporting. An international registry for CTEPH from North America and Europe reported that up to 75% of patients with CTEPH had a definite proceeding episode of PE [8]. In contrast, data from Japan reported antecedent PE in around 15–33% of patients with CTEPH [9][10]. Studies from Japan have shown 80% female preponderance, while those from North America and Europe have reported around 49.9% incidence in females [8][9]. The nonspecific presentation of the disease, underutilization of the guideline-recommended ventilation-perfusion (V/Q) scan for screening, and lack of expertise in interpreting nuclear and radiological studies have made it difficult to quantify the burden of CTEPH more uniformly across the world.
3. Pathophysiology of CTEPH
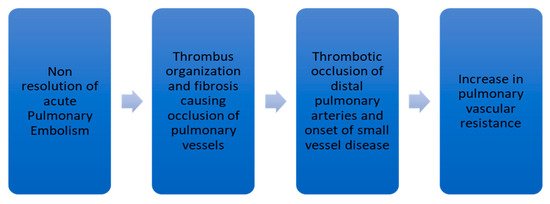
The current understanding of the pathophysiology of CTEPH indicates a more complex phenomenon than mere chronic obstruction of pulmonary vascular bed by unresolved thrombus and subsequent right ventricular (RV) dysfunction. Chronic obstruction of proximal pulmonary vessels by fibrotic clots, development of small vessel disease, and progressive diffuse remodeling of the pulmonary vasculature collectively represent the pathophysiology of CTEPH [10][11].Nonresolution of thrombus after PE occurs only in a minority of patients. This leads to failure in the restoration of normal hemodynamics in the pulmonary circulatory system. In acute PE, fresh red clots made of red blood cells and fibrin mesh are easily detachable from the wall of the pulmonary vessels. In contrast, chronic clots are yellow-colored and composed of abundant inflammatory cells, elastin, and collagen fibers [10][12]. Further organization of the chronic clot impairs blood flow and leads to CTEPH development. This organization and fibrosis represent the characteristic bands and webs in a pulmonary angiogram [13]. Simonneau G. et al. [10] and Lang IM et al. [14] have summarized the pathophysiology of CTEPH as depicted in Figure 1.
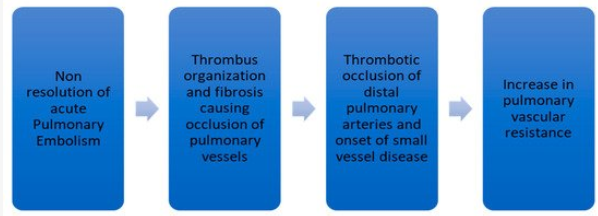
Figure 1. Flow diagram showing the pathophysiology of CTEPH.
1. Introduction
| Group 1 | Pulmonary Arterial Hypertension (PAH) | ||
| Group 2 | Due to Left Heart Disease | ||
| Group 3 | Due to Chronic Lung Disease/Hypoxemia | ||
| Group 4 | Due to Pulmonary Arterial Obstructions | ||
| Group 5 | Multifactorial | ||
| February 2017 | Metanalysis of patients with PE followed up for CTEPH. Sample size n: 4047 patients from 16 studies | -CTEPH incidence was 3.2% (95% CI 2–4.4) of 999 patients who survived after PE ≥ 2 years (4 studies) -Pooled CTEPH incidence 0.56% (95% CI 0.1–1.0) (3 studies) -In survivors without major comorbidities, incidence was 2.8% in 1775 patients (9 studies) |
|
| Miniati M et al. [4] | September 2006 | Prospective study of 320 patients with proven PE follow-up for a median duration of 2.1 years | 4 out of 320 patients with proven PE (1%) developed CTEPH |
| Klok FA et al. [5] | January 2010 | Cohort screening study in 866 patients with acute PE studied between January 2001 and July 2007 |
| Investigators | Year of Publication | Type of Study | Main Results |
|---|---|---|---|
| Ende-Verhaar YM et al. [3] | February 2017 | Metanalysis of patients with PE followed up for CTEPH. Sample size n: 4047 patients from 16 studies | -CTEPH incidence was 3.2% (95% CI 2–4.4) of 999 patients who survived after PE ≥ 2 years (4 studies) -Pooled CTEPH incidence 0.56% (95% CI 0.1–1.0) (3 studies) -In survivors without major comorbidities, incidence was 2.8% in 1775 patients (9 studies) |
| Miniati M et al. [4] | September 2006 | Prospective study of 320 patients with proven PE follow-up for a median duration of 2.1 years | 4 out of 320 patients with proven PE (1%) developed CTEPH |
| Klok FA et al. [5] | January 2010 | Cohort screening study in 866 patients with acute PE studied between January 2001 and July 2007 | CTEPH incidence was 0.57% (95% CI, 0.02–1.2%) in all-cause PE and 1.5% (95% CI, 0.08–3.1%) in provoked PE |
| Pengo V. [6] | May 2004 | Prospective follow-up of 223 patients with acute PE for median duration of 94.3 months. Follow-up ventilation-perfusion scan and pulmonary angiography done in patients suspected to have CTEPH | CTEPH incidence was 1% (95% CI, 0.0–2.4) at 6 months, 3.1% (95% CI, 0.7–5.5) at 1 year, and 3.8% (95 CI, 1.1–6.5) at 2 years |
| Berghaus TM [7] | December 2011 | Cohort screening study of 43 survivors of recurrent PE | CTEPH in 5 patients (11.6%) patients with recurrent PE |
2. Epidemiology
| Investigators | Year of Publication | Type of Study | Main Results |
|---|---|---|---|
| Ende-Verhaar YM et al. [3] | |||
| CTEPH incidence was 0.57% (95% CI, 0.02–1.2%) in all-cause PE and 1.5% (95% CI, 0.08–3.1%) in provoked PE | |||
| Pengo V. [6] | May 2004 | Prospective follow-up of 223 patients with acute PE for median duration of 94.3 months. Follow-up ventilation-perfusion scan and pulmonary angiography done in patients suspected to have CTEPH | CTEPH incidence was 1% (95% CI, 0.0–2.4) at 6 months, 3.1% (95% CI, 0.7–5.5) at 1 year, and 3.8% (95 CI, 1.1–6.5) at 2 years |
| Berghaus TM [7] | December 2011 | Cohort screening study of 43 survivors of recurrent PE | CTEPH in 5 patients (11.6%) patients with recurrent PE |
3. Pathophysiology of CTEPH