The demand to improve mental quality of life has increased along with the recent increase in interest in and awareness of mental health. Consequently, the concept of mental health services emerged, along with an increased demand to manage mental health using information and communication technology (ICT) such as mobile communication and social network services (SNS).
- mobile mental health
- application
- information and communication technology
1. Introduction
The World Health Organization (WHO) defined mobile health (m-Health) or mobile healthcare as medical and public health services provided through mobile devices including smartphones. In other words, mobile healthcare is the exchange of medical services between physicians and patients using IT and mobile devices, free from restrictions of time and space [1]. In that sense, the use of mobile apps for mental health management is expected to have various advantages [2]. In South Korea specifically, smartphone usage is approximately 90% and thus, interventions using readily available smartphones may grant excellent accessibility. It also offers economic advantages of reducing medical costs and can help overcome limitations of accessibility compared to the in-person cognitive behavioral therapy previously used for mental health management [3]. Furthermore, mobile apps enable user-friendly access through their various functions. Mental health-related mobile apps are referred to as “Mental Health apps (MHapps),” and their types and numbers are diverse [4]. Nevertheless, mental health apps that have insufficient medical evidence or are for commercial use are common, and it is to be expected that such apps will continue to be developed and distributed in the future. Therefore, in order to efficiently manage the mental health of citizens, the development and distribution of apps with proven effectiveness and reliability are needed. Mental health specialists, in particular, should demonstrate leadership in studying, evaluating, and integrating such apps [5]. Nonetheless, there is a lack of scoping review identifying trends in research and evidence-based app development and application on topics such as the effects of mental health apps. Thus, this study aimed to perform a scoping review of previous research on the application of mental health apps on the general adult population and systematically analyze the content, methods, and effectiveness of the proposed intervention programs.
2. Methods
A scoping review of various databases was conducted, as outlined below, to identify intervention studies that used mental health apps for the general adult population over the age of 18, with the purpose of presenting directions and possible research questions for future research. It consists of six steps of identifying the research question, identifying relevant studies, study selection, charting the data, collecting, summarizing, and reporting results and recommendations [6][7].
3. General Characteristics of the Literature
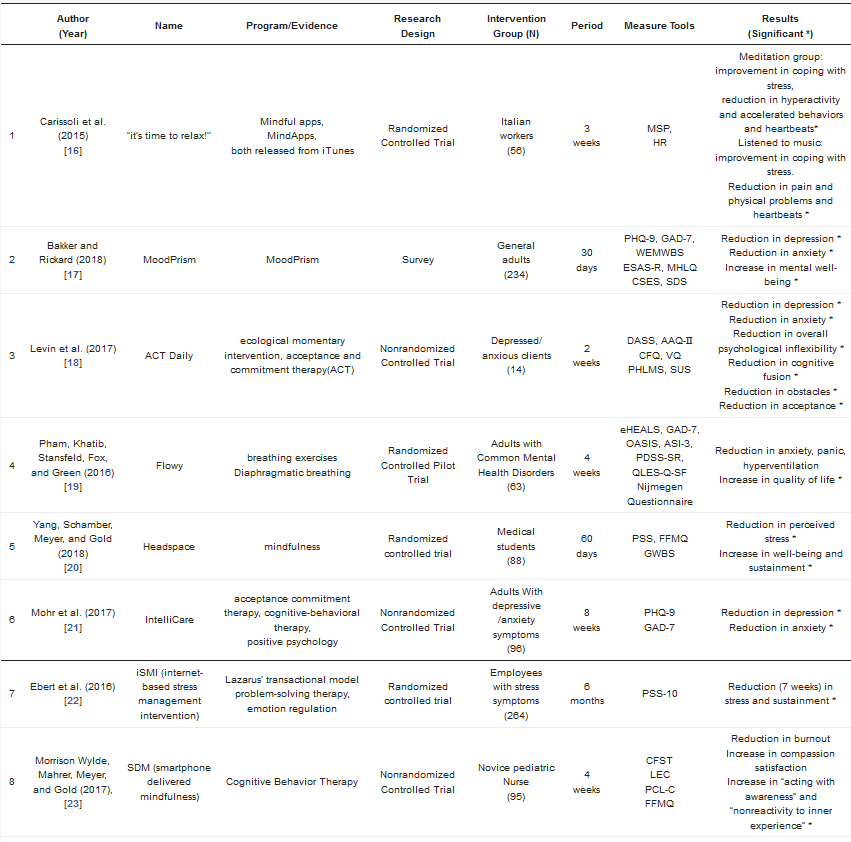
As there were articles analyzed up until 2013 [8], articles from studies conducted after 2010 were included in the search. The general characteristics of the final 14 articles selected to analyze the effectiveness of mental health apps in adults, are as shown in Table 1. There was one article published between 2010 and 2015 (7.1%) [9] and 13 articles published after 2016 (92.9%) [10][11][12][13][14][15][16][17][18][19][20][21][22], which made up most of the selected papers. The study designs of the selected articles were one research study (7.1%) [10], 10 RCTs (Randomized Controlled Trial) (71.4%) [9][12][13][15][17][18][19][20][21][22], and three NRCTs (Nonrandomized Controlled Trial) (21.4%) [10][13][15]. In terms of the intervention subjects, there were various types, with three studies on normal adults (21.4%) [10][17][18], three studies on symptomatic cases (21.4%) [11][12][14], two workers (14.3%) [9][15], two nurses (14.3%) [16][22], one soldier (7.1%) [19], and three students (21.4%) [13][20][21]. The duration of intervention varied from 2 to 24 weeks, with nine studies less than four weeks long (64.3%), three 8-week studies (21.4%) [13][14][19], one 12-week study (7.1%) [18], and one 24-week study (7.1%) [15]. Over 60% of the selected studies lasted for less than four weeks [9][10][11][12][16][17][20][21][22].
4. Summary of the Literature
One study [10] analyzed the effects of a mobile app (MoodPrism) through hierarchical regression analysis. MoodPrism is a self-monitoring app that examines the impact of subjects’ emotional self-awareness on their mental health. A program involving 234 participants demonstrated an impact of 18%, 20%, and 37% on depression, anxiety, and mental well-being, respectively (Table 1).Table 1. Characteristics and outcomes of selected 14 studies.
| Author (Year) |
Name | Program/Evidence | Research Design |
Intervention Group (N) | Period | Measure Tools | Results (Significant *) |
|
|---|---|---|---|---|---|---|---|---|
| 1 | Carissoli et al. (2015) [16] |
“it’s time to relax!’’ | Mindful apps, MindApps, both released from iTunes |
Randomized Controlled Trial | Italian workers (56) |
3 weeks | MSP, HR |
Meditation group: improvement in coping with stress, reduction in hyperactivity and accelerated behaviors and heartbeats* Listened to music: improvement in coping with stress. Reduction in pain and physical problems and heartbeats * |
| 2 | Bakker and Rickard (2018) [17] |
MoodPrism | MoodPrism | Survey | General adults (234) |
30 days | PHQ-9, GAD-7, WEMWBS ESAS-R, MHLQ CSES, SDS |
Reduction in depression * Reduction in anxiety * Increase in mental well-being * |
| 3 | Levin et al. (2017) [18] |
ACT Daily | ecological momentary intervention, acceptance and commitment therapy(ACT) | Nonrandomized Controlled Trial | Depressed/ anxious clients (14) |
2 weeks | DASS, AAQ-Ⅱ CFQ, VQ PHLMS, SUS |
Reduction in depression * Reduction in anxiety * Reduction in overall psychological inflexibility * Reduction in cognitive fusion * Reduction in obstacles * Reduction in acceptance * |
| 4 | Pham, Khatib, Stansfeld, Fox, and Green (2016) [19] |
Flowy | breathing exercises Diaphragmatic breathing |
Randomized Controlled Pilot Trial | Adults with Common Mental Health Disorders (63) |
4 weeks | eHEALS, GAD-7, OASIS, ASI-3, PDSS-SR, QLES-Q-SF Nijmegen Questionnaire |
Reduction in anxiety, panic, hyperventilation Increase in quality of life * |
| 5 | Yang, Schamber, Meyer, and Gold (2018) [20] |
Headspace | mindfulness | Randomized controlled trial | Medical students (88) |
60 days | PSS, FFMQ GWBS |
Reduction in perceived stress * Increase in well-being and sustainment * |
| 6 | Mohr et al. (2017) [21] |
IntelliCare | acceptance commitment therapy, cognitive-behavioral therapy, positive psychology |
Nonrandomized Controlled Trial | Adults With depressive /anxiety symptoms (96) |
8 weeks | PHQ-9 GAD-7 |
Reduction in depression * Reduction in anxiety * |
| 7 | Ebert et al. (2016) [22] |
iSMI (internet- based stress management intervention) |
Lazarus’ transactional model problem-solving therapy, emotion regulation |
Randomized controlled trial | Employees with stress symptoms (264) |
6 months |
PSS-10 | Reduction (7 weeks) in stress and sustainment * |
| 8 | Morrison Wylde, Mahrer, Meyer, and Gold (2017), [23] |
SDM (smartphone delivered mindfulness) | Cognitive Behavior Therapy | Nonrandomized Controlled Trial | Novice pediatric Nurse (95) |
4 weeks |
CFST LEC PCL-C FFMQ |
Reduction in burnout Increase in compassion satisfaction Increase in “acting with awareness” and “nonreactivity to inner experience” * |
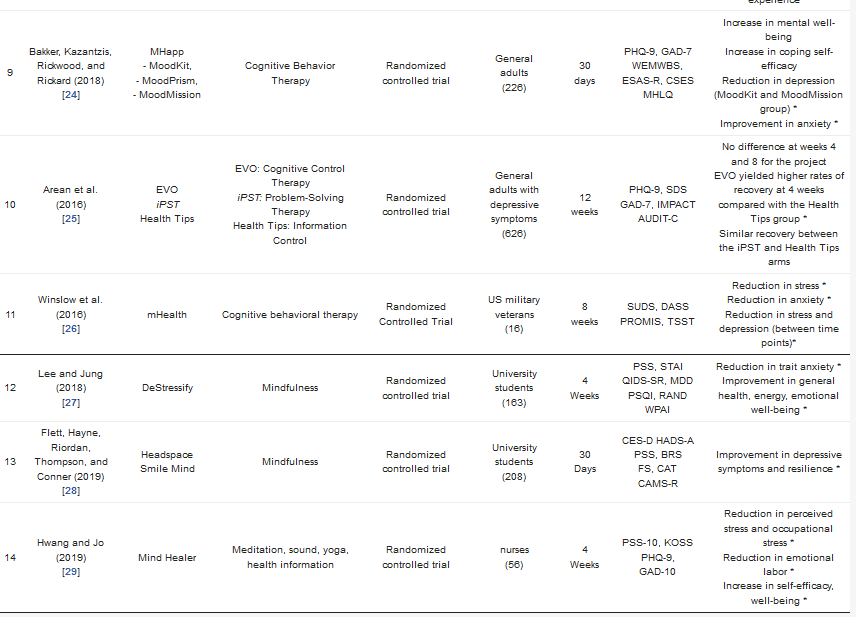
| 9 | Bakker, Kazantzis, Rickwood, and Rickard (2018) [24] |
MHapp - MoodKit, - MoodPrism, - MoodMission |
Cognitive Behavior Therapy |
Randomized controlled trial | General adults (226) |
30 days |
PHQ-9, GAD-7 WEMWBS, ESAS-R, CSES MHLQ |
Increase in mental well-being Increase in coping self-efficacy Reduction in depression (MoodKit and MoodMission group) * Improvement in anxiety * |
| 10 | Arean et al. (2016) [25] |
EVO iPST Health Tips |
EVO: Cognitive Control Therapy iPST: Problem-Solving Therapy Health Tips: Information Control |
Randomized controlled trial | General adults with depressive symptoms (626) |
12 weeks |
PHQ-9, SDS GAD-7, IMPACT AUDIT-C |
No difference at weeks 4 and 8 for the project EVO yielded higher rates of recovery at 4 weeks compared with the Health Tips group * Similar recovery between the iPST and Health Tips arms |
| 11 | Winslow et al. (2016) [26] |
mHealth | Cognitive behavioral therapy | Randomized Controlled Trial | US military veterans (16) |
8 weeks | SUDS, DASS PROMIS, TSST |
Reduction in stress * Reduction in anxiety * Reduction in stress and depression (between time points)* |
| 12 | Lee and Jung (2018) [27] |
DeStressify | Mindfulness | Randomized controlled trial | University students (163) |
4 Weeks |
PSS, STAI QIDS-SR, MDD PSQI, RAND WPAI |
Reduction in trait anxiety * Improvement in general health, energy, emotional well-being * |
| 13 | Flett, Hayne, Riordan, Thompson, and Conner (2019) [28] |
Headspace Smile Mind |
Mindfulness | Randomized controlled trial | University students (208) |
30 Days |
CES-D HADS-A PSS, BRS FS, CAT CAMS-R |
Improvement in depressive symptoms and resilience * |
| 14 | Hwang and Jo (2019) [29] |
Mind Healer | Meditation, sound, yoga, health information |
Randomized controlled trial | nurses (56) |
4 Weeks |
PSS-10, KOSS PHQ-9, GAD-10 |
Reduction in perceived stress and occupational stress * Reduction in emotional labor * Increase in self-efficacy, well-being * |
5. Experimental Research Using Mobile Apps
There were 13 intervention studies using mobile apps [9][11][12][13][14][15][16][17][18][19][20][21][22]. The purposes of such mobile app interventions varied, including stress management, reduction of anxiety, reduction in depression, increase in well-being, and provision of feedback on mental health apps. The intervention period also varied, ranging from 2 to 24 weeks in duration. More specifically, there was one 2-week study [11], one 3-week study [9], three 30-day studies [10][13][17][21], two 4-week studies [12][16][20][22], two 8-week studies [14][19], one 12-week study [18], and one 24-week study [15].For studies in which the purpose of the intervention was to provide feedback on the application of mental health apps, the results were measured in several ways. The result variables from the measurements of the effectiveness of the mobile app are as follows—13 articles on stress [9][10][11][13][14][15][16][17][18][19][20][21][22], nine articles on depression [10][11][14][17][18][19][20][21][22], 10 articles on anxiety [10][11][12][14][17][18][19][20][21][22], and five articles on well-being [10][13][17][20][22]. Furthermore, quality of life [12][13], self-efficacy [10][17][22], alcohol dependency [18], hyperventilation [12], sleep quality [20], work productivity [20], resilience [21], fatigue [16], mental health literacy [10][17], and emotional labor [22] were examined, and five articles [10][11][16][19][22] explored the accessibility and functional characteristics of the mobile applications (Table 1).
6. Mobile App Programs and Theoretical Evidence
The mobile apps used in the studies were, “It’s time to relax!” [9], “MoodPrism” [10], “ACT Daily” [11], “Flowy” [12], “Headspace” [13], “IntelliCare” [14], “internet-based stress management intervention (iSMI)” [15], “smartphone delivered mindfulness (SDM)” [16], “Mhapp (MoodKit, MoodPrism, MoodMission)” [17], “Cognitive Control App” [18], “mHealth” [19], “DeStressify” [20], “Headspace & Smiling Mind” [21], and “Mind Healer” [22]. Of the 14 articles, the most used apps were based on mindful meditation, used in five studies [9][13][16][20][21] (35.7%). Four studies used [16][17][18][19] cognitive behavioral therapy apps; one study [15] used a complex program involving problem-solving, relaxation, and acceptance tolerance therapy based on stress theory; one study [11] used an acceptance tolerance therapy app based on ecological momentary intervention (EMI); and another study [22] used a complex program involving meditation, yoga, and sound. There were two studies in which theoretical evidence was not provided, each using a breathing exercise app [12] and a mood-monitoring app [10].
- “IntelliCare” [14] is an app developed with the purpose of reducing depression or anxiety caused by sleep disorders, social isolation, or lack of physical activity, based on acceptance and commitment, conscious behavior, optimism, and problem-solving techniques.
- “iSMI (Internet-based stress management intervention)” [15] is an internet-based stress management program aimed to reduce stress, comprised of eight modules using problem-solving, relaxation, and acceptance tolerance therapy. Through adherence monitoring by an E-coach and presenting feedback pertaining to the user’s needs, an opportunity for the user to develop self-guided health promotion and behavioral change is provided.
- “Mhapp (MoodKit, MoodPrism, MoodMission)” [17] is a study involving the use of 3 apps—“MoodKit” and “MoodMission” are apps designed to manage depression, anxiety, and stress based on cognitive behavioral therapy. Upon analyzing mood, activity, values, and sentiment, it provides individualized goals that the user can choose and work towards.
- “Cognitive Control App” [18] is an app designed for the user to actively self-regulate behavior through choosing appropriate activities and refusing activities deemed inappropriate. It uses Cognitive Control Therapy (EVO), Problem-Solving Therapy App (iPST), Information Control (Health Tips) apps to facilitate both problem-solving abilities and provision of health information.
- “mHealth” [19] is a mobile app with a combination approach involving wearables and cognitive behavioral therapy to reduce stress, depression, anxiety, and rage, developed to compensate for limitations observed in traditional approaches involving only cognitive behavioral therapy, such as dropout and loss, as well as the shortage of objective data between user experience and cognitive behavioral therapy sessions. Additionally, it provides objective data for the users and providers by identifying the user’s condition through cardiovascular and electrodermal input from wearable devices, enabling the detection of psychological stress.
- “Mind Healer” [22] is an app developed for workers and the general adult population to manage stress and involves a psychological test and a PPG sensor that measures heart rate, enabling users to measure their mental health status, thus increasing workers’ self-awareness. Additionally, if stress, anxiety, or depression is detected, a short-term healing program is offered, providing breathing, meditation, music, and yoga practices for healing and management of mental health. By also providing materials for mental health education, the app enables users to promote mental health by themselves.
7. Effectiveness of Mental Health Interventions using Mobile Apps
2. Methods
3. General Characteristics of the Literature
4. Summary of the Literature
5. Experimental Research Using Mobile Apps
6. Mobile App Programs and Theoretical Evidence
-
“IntelliCare” [21] is an app developed with the purpose of reducing depression or anxiety caused by sleep disorders, social isolation, or lack of physical activity, based on acceptance and commitment, conscious behavior, optimism, and problem-solving techniques.
-
“iSMI (Internet-based stress management intervention)” [22] is an internet-based stress management program aimed to reduce stress, comprised of eight modules using problem-solving, relaxation, and acceptance tolerance therapy. Through adherence monitoring by an E-coach and presenting feedback pertaining to the user’s needs, an opportunity for the user to develop self-guided health promotion and behavioral change is provided.
-
“Mhapp (MoodKit, MoodPrism, MoodMission)” [24] is a study involving the use of 3 apps—“MoodKit” and “MoodMission” are apps designed to manage depression, anxiety, and stress based on cognitive behavioral therapy. Upon analyzing mood, activity, values, and sentiment, it provides individualized goals that the user can choose and work towards.
-
“Cognitive Control App” [25] is an app designed for the user to actively self-regulate behavior through choosing appropriate activities and refusing activities deemed inappropriate. It uses Cognitive Control Therapy (EVO), Problem-Solving Therapy App (iPST), Information Control (Health Tips) apps to facilitate both problem-solving abilities and provision of health information.
-
“mHealth” [26] is a mobile app with a combination approach involving wearables and cognitive behavioral therapy to reduce stress, depression, anxiety, and rage, developed to compensate for limitations observed in traditional approaches involving only cognitive behavioral therapy, such as dropout and loss, as well as the shortage of objective data between user experience and cognitive behavioral therapy sessions. Additionally, it provides objective data for the users and providers by identifying the user’s condition through cardiovascular and electrodermal input from wearable devices, enabling the detection of psychological stress.
-
“Mind Healer” [29] is an app developed for workers and the general adult population to manage stress and involves a psychological test and a PPG sensor that measures heart rate, enabling users to measure their mental health status, thus increasing workers’ self-awareness. Additionally, if stress, anxiety, or depression is detected, a short-term healing program is offered, providing breathing, meditation, music, and yoga practices for healing and management of mental health. By also providing materials for mental health education, the app enables users to promote mental health by themselves.
7. Effectiveness of Mental Health Interventions using Mobile Apps
The use of an intervention app based on the stress model by 264 workers demonstrated a significant reduction in stress after seven weeks of use, which was maintained in follow-up observations from seven weeks to six months of use [15]. Furthermore, in a study involving the distribution of 626 normal adults into three groups, each using a Cognitive Control Therapy app, a Problem-solving Therapy app, and an Information Control app, no significant differences were observed between weeks 4 and 8, but a higher recovery rate was observed in the group using the Cognitive Control Therapy app at four weeks compared to the group using a health information app [18]. When individual with mental health disorders was subject to using apps that provided a 4-week training program on breathing, a significant improvement in quality of life was reported, along with reductions in anxiety, panic, and hyperventilation, though the observed differences were not significant [12]. In the case of the study on the IntelliCare app [14], in which interventions on commitment to acceptance, cognitive behavioral therapy, and positive psychology were provided to 96 adults, significant reductions were observed in both depression and anxiety. A 2-week intervention using an app providing EMI-based Acceptance and Commitment Therapy in 14 depressed and anxious patients demonstrated significant reductions in anxiety, psychological inflexibility, cognitive fusion, obstacle, and acceptance [11]. A study involving an 8-week provision of cognitive behavioral therapy through an app to 35 American soldiers demonstrated significant reductions in stress, anxiety, and depression [19], and when cognitive behavioral therapy was provided to 226 normal adults through an app, improvements in emotional well-being and self-efficacy in coping were observed, along with reduced anxiety. In the Moodkit and Moodmission groups, especially, significant reductions in depression were reported [17]. When cognitive control therapy was provided to normal adults with depressive symptoms for 12 weeks, significantly higher rates of recovery were observed after four weeks, compared to the control group [18]. When cognitive behavioral therapy was provided to 95 newly appointed pediatric nurses for 4 weeks, significant increases were observed in acting with awareness and nonreactivity to inner experience, along with reduced in burnout and increased compassion satisfaction. Additionally, in a 4-week trial of the Mind Healer app in workers, significant reductions were observed in stress and emotional labor, while significant improvements were observed in well-being and self-efficacy following app use
References
- Carissoli, C.; Villani, D.; Riva, G. Does a meditation protocol supported by a mobile application help people reduce stress? Suggestions from a controlled pragmatic trial. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 46–53.
- Bakker, D.; Rickard, N. Engagement in mobile phone app for self-monitoring of emotional wellbeing predicts changes in mental health: MoodPrism. J. Affect. Disord. 2018, 227, 432–442.
- Levin, M.E.; Haeger, J.; Pierce, B.; Cruz, R.A. Evaluating an Adjunctive Mobile App to Enhance Psychological Flexibility in Acceptance and Commitment Therapy. Behav. Modif. 2017, 41, 846–867.
- Pham, Q.; Khatib, Y.; Stansfeld, S.; Fox, S.; Green, T. Feasibility and Efficacy of an mHealth Game for Managing Anxiety: “Flowy” Randomized Controlled Pilot Trial and Design Evaluation. Games Health J. 2016, 5, 50–67.
- Yang, E.; Schamber, E.; Meyer, R.M.L.; Gold, J.I. Happier Healers: Randomized Controlled Trial of Mobile Mindfulness for Stress Management. J. Altern. Complement. Med. 2018, 24, 505–513.
- Mohr, D.C.; Tomasino, K.N.; Lattie, E.G.; Palac, H.L.; Kwasny, M.J.; Weingardt, K.; Schueller, S.M. IntelliCare: An Eclectic, Skills-Based App Suite for the Treatment of Depression and Anxiety. J. Med Internet Res. 2017, 19, e10.
- Ebert, D.D.; Lehr, D.; Heber, E.; Riper, H.; Cuijpers, P.; Berking, M. Internet- and mobile-based stress management for employees with adherence-focused guidance: Efficacy and mechanism of change. Scand. J. Work Environ. Health 2016, 42, 382–394.
- Morrison Wylde, C.; Mahrer, N.E.; Meyer, R.M.L.; Gold, J.I. Mindfulness for Novice Pediatric Nurses: Smartphone Application Versus Traditional Intervention. J Pediatr. Nurs. 2017, 36, 205–212.
- Bakker, D.; Kazantzis, N.; Rickwood, D.; Rickard, N. A randomized controlled trial of three smartphone apps for enhancing public mental health. Behav. Res. Ther. 2018, 109, 75–83.
- Arean, P.A.; Hallgren, K.A.; Jordan, J.T.; Gazzaley, A.; Atkins, D.C.; Heagerty, P.J.; Anguera, J.A. The use and effectiveness of mobile apps for depression: Results from a fully remote clinical trial. J. Med. Internet Res. 2016, 18, e330.
- Winslow, B.D.; Chadderdon, G.L.; Dechmerowski, S.J.; Jones, D.L.; Kalkstein, S.; Greene, J.L.; Gehrman, P. Development and Clinical Evaluation of an mHealth Application for Stress Management. Front. Psychiatry 2016, 7, 130.
- Lee, R.A.; Jung, M.E. Evaluation of an mHealth App (DeStressify) on university students’ mental health: Pilot trial. JMIR Ment. Health 2018, 5, e2.
- Flett, J.A.; Hayne, H.; Riordan, B.C.; Thompson, L.M.; Conner, T.S. Mobile mindfulness meditation: A randomised controlled trial of the effect of two popular apps on mental health. Mindfulness 2019, 10, 863–876.
- Hwang, W.J.; Jo, H.H. Evaluation of the Effectiveness of Mobile App-Based Stress-Management Program: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4270.
- Ebert, D.D.; Lehr, D.; Heber, E.; Riper, H.; Cuijpers, P.; Berking, M. Internet- and mobile-based stress management for employees with adherence-focused guidance: Efficacy and mechanism of change. Scand. J. Work Environ. Health 2016, 42, 382–394.
- Morrison Wylde, C.; Mahrer, N.E.; Meyer, R.M.L.; Gold, J.I. Mindfulness for Novice Pediatric Nurses: Smartphone Application Versus Traditional Intervention. J Pediatr. Nurs. 2017, 36, 205–212.
- Bakker, D.; Kazantzis, N.; Rickwood, D.; Rickard, N. A randomized controlled trial of three smartphone apps for enhancing public mental health. Behav. Res. Ther. 2018, 109, 75–83.
- Arean, P.A.; Hallgren, K.A.; Jordan, J.T.; Gazzaley, A.; Atkins, D.C.; Heagerty, P.J.; Anguera, J.A. The use and effectiveness of mobile apps for depression: Results from a fully remote clinical trial. J. Med. Internet Res. 2016, 18, e330.
- Winslow, B.D.; Chadderdon, G.L.; Dechmerowski, S.J.; Jones, D.L.; Kalkstein, S.; Greene, J.L.; Gehrman, P. Development and Clinical Evaluation of an mHealth Application for Stress Management. Front. Psychiatry 2016, 7, 130.
- Lee, R.A.; Jung, M.E. Evaluation of an mHealth App (DeStressify) on university students’ mental health: Pilot trial. JMIR Ment. Health 2018, 5, e2.
- Flett, J.A.; Hayne, H.; Riordan, B.C.; Thompson, L.M.; Conner, T.S. Mobile mindfulness meditation: A randomised controlled trial of the effect of two popular apps on mental health. Mindfulness 2019, 10, 863–876.
- Hwang, W.J.; Jo, H.H. Evaluation of the Effectiveness of Mobile App-Based Stress-Management Program: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 4270.
