Biomarkers are molecules that are variable in their origin, nature, and mechanism of action; they are of great relevance in biology and also in medicine because of their specific connection with a single or several diseases. Biomarkers are of two types, which in some cases are operative with each other. Fluid biomarkers, started around 2000, are generated in fluid from specific proteins/peptides and miRNAs accumulated within two extracellular fluids, either the central spinal fluid or blood plasma. The switch of these proteins/peptides and miRNAs, from free to segregated within extracellular vesicles, has induced certain advantages including higher levels within fluids and lower operative expenses. Imaging biomarkers, started around 2004, are identified in vivo upon their binding by radiolabeled molecules subsequently revealed in the brain by positron emission tomography and/or other imaging techniques. A positive point for the latter approach is the quantitation of results, but expenses are much higher.
- neurons
- astrocytes
- Alzheimer’s and Parkinson’s diseases
- fluid and imaging biomarkers
- amyloid-β and tau
- miRNA
- extracellular vesicles
- exosomes and ectosomes
- PET
- radiotracers
- radiolabeled molecules
1. Introduction
Biomarkers are molecules that are highly variable in their origin, nature, and mechanism of action, and they are connected to or are directly involved to single or various peculiar diseases. At present, biomarkers, which are addressed to cells, organs, or structures, exist for almost all diseases, including cancers. Among them, neurodegenerative diseases are receiving the greatest attention. During the last 20 years, articles about their biomarkers published in known journals have reached a total of over 20,000, including about 4000 reviews. Investigations of their properties, going from specificity to the mechanisms of their action, are often used to clarify various aspects of pathogenesis. Such results often play roles in processes of medical relevance, such as diagnosis, prognosis, and also therapy, and they are useful for patients and also for clinical practice. However, the relevance of biomarkers in clinical practice is variable. Some of them are well known and widely used; for others, however, knowledge is still questioned due to, for example, their limited specificity. In this review such limitations are not further illustrated. The properties of biomarkers presented here are those of general significance, identified in the last few years. Information about additional aspects can be found in other publications [1][2][1,2].
Compared to biomarkers of other organs, biomarkers of the brain exhibit distinct properties [3][4][3,4]. Initial studies about two types, the fluid and the imaging biomarkers, were developed separately. Biomarkers of the first type appeared around 2000. They are collected not in vivo but in fluid, within either of two fluids taken from patients, the central spinal fluid (CSF) and the blood plasma [5][6][5,6]. Biomarkers of the second type were developed by the use of radiolabeled molecules. Upon penetration into the living brain, these molecules are bound with high specificity as revealed by positron emission tomography (PET) imaging. A biomarker study by the latter approach, addressed to amyloid-β (Aβ) plaques of Alzheimer’s disease (AD), was published in 2004 [7]. Since then, the in vivo studies of the imaging type have continued with growing success (see Section 5). Since the beginning of the two types of biomarker studies, the state of neurodegenerative diseases changed profoundly. In particular, biomarkers did recently revolutionize scientific and medical research by transforming drug trial design and also improving patient management in clinical practice [8].
So far, I have introduced the two types, i.e., fluid and imaging biomarkers. The in vivo imaging of the latter takes place upon their high affinity binding by radiolabeled specific molecules introduced in the brain. In contrast, fluid biomarkers are collected within (CSF) or away (blood) from the central nervous system. Yet, all fluid biomarkers are adequate to identify central molecules/processes, critical for patients suffering neurodegenerative diseases, not only AD but also Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), and other diseases. Initially, the disease identification was searched by the recovery in the fluids of free specific molecules. These molecules, however, are largely digested during their traffic, from the cells affected by the disease to the accumulation in the fluids. Thus, their identification was often difficult. The problem has been solved recently by changing the study from free molecules to cargo molecules segregated within extracellular vesicles (EVs). This change will be presented in detail in Section 3.
Initially, each neurodegenerative disease was considered dependent on a single specific biomarker, such as Aβ for AD and α-synuclein for PD. Now it is clear that these two, as well as many other biomarkers, are not fully specific but expressed also by patients of other neurodegenerative diseases [9]. Multispecificity of biomarkers requires caution in their operation. Caution is necessary also with another type of problem. Initially considered specific and efficient, some biomarkers have been found to be hardly reproducible, thus inappropriate for research and clinical practice [8]. A final important consideration refers to the age dependence of disease investigation/treatment. Specific biomarkers have been applied not only to mature patients, but also to patients at early stages of disease. By novel and innovated methods, it could be established whether patients at risk of long-term diseases, such as AD or dementia, can be treated only upon full development of their symptoms, or also when symptoms are absent or still at an early stage [10][11][10,11].
2. Fluids
In the Introduction, I already mentioned the two ways leading to the generation of neural biomarkers, i.e., the first based on the analysis of peripheral fluids containing appropriate molecules, the second in vivo, based on the imaging by PET labeling of specific brain molecules. How is it that fluids are essential for the first, very important approach? Two of their properties need to be emphasized. First, molecules of interest for their recognition as biomarkers need to be present in the biological fluids of human body; second, the analysis of fluids, with ensuing isolation of molecules, is less expensive, much easier, and does not disrupt the body compared to the in vivo analysis of tissues. In other words, the fluids are advantageous in the development of biomarkers.
In the body of mammal animals, including humans, there are 8 types of external fluids. For our purposes, however, only two are relevant: the CSF and the blood plasma. Molecules and the small organelles EVs, released from brain cells such as neurons, and astrocytes and microglia, navigate in the extracellular fluid space from which they are easily transferred to the CSF [3] (step 2 in Figure 1). At the arachnoid villi, the EVs of the CSF can move to venous blood within large vacuoles (step 4 in Figure 1). In addition, the molecules and EVs have been shown to traffic through the blood–brain barrier [12][13][12,13] (step 3 in Figure 1). The latter is the structure known to reduce/exclude the traffic of many other molecules and organelles to and from the brain.
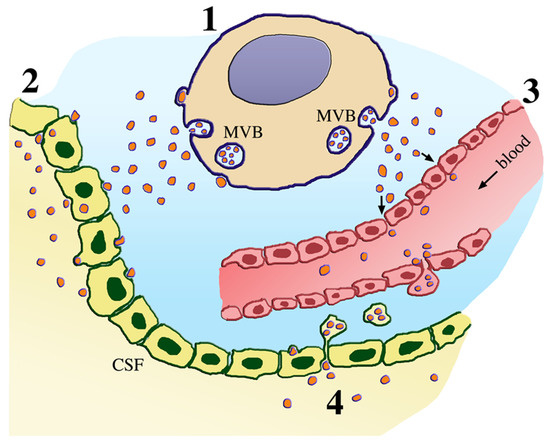
Figure 1. Traffic of extracellular vesicles (EVs) released by a neural cell. The neural cell at the top (cytoplasm of grain color, marked 1) releases the two types of EVs, the small exosomes by exocytosis of multivesicular bodies (MVB), and the larger ectosomes by shedding of plasma membrane rafts. Upon release, the vesicles navigate in the extracellular fluid (light blue). Their targeting relevant for fluid biomarker generation can be accumulate either to the central spinal fluid (CSF) of the ventricular system (left, peach color, marked 2) or as shown by the arrows to the blood (right, red-pink color, marked 3). Additional CSF-to-blood EV transfer occurs by large vacuoles operative at the arachnoid villi (bottom, marked 4). Thus, molecules and EVs can move from the extracellular space and the CSF to the blood plasma. In the case of neurodegenerative diseases, the molecules and EVs of such origin account for significant fractions of the total transferred to the fluids.
Recent studies have shown that biomarkers of the two fluids, CSF and blood plasma, are employed approximately with the same frequency. The choice of one fluid, however, is not due to a negative evaluation of the other. In recent reviews, both are reported as valid [12][14][12,14]. Rather, the choice appears to depend on advantages existing in either fluid. High levels of molecules and EVs are present in CSF (Figure 1), which is more invasive and requires more expenses than the blood for biomarker generation. Yet, the CSF fluid has made it possible to have processes of low concentrated proteins, for example, those of the COVID-19 disease reported this year in patients exhibiting neurological symptoms, evident of cerebral infection [15]. In the blood, plasma withdrawal can be large, frequently repeated, and not expensive. However the levels of molecules/EVs in this fluid are lower than in the CSF. The transfer of various EVs across the blood–brain barrier (BBB) has been shown to be different, with ensuing variability of the plasma levels [16]. In many cases, however, they have emerged in the study of neurodegenerative diseases, with enormous potential as a diagnostic, evaluation of therapeutics, and treatment tool.
Summing up, both fluids are employed for biomarker generation. However, the choices depend on their distinct properties. The processes of biomarker generation, previously defined of liquid biopsy [13], have been shown to identify not only the fluid molecules but also the brain pathologic EVs inaccessible in vivo. In addition, fluids have offered unique opportunities, as seen from recent clinical trials, to improve the quality and applicability of results.
3. From Molecules to Extracellular Vesicles
Neurodegenerative diseases are heterogeneous disorders characterized by a progressive and severe cognitive and functional decline leading to the progressive loss of function and death of neuronal cells. Due to the complexity of their diagnosis, early detection and treatments are difficult to recognize, and this is critical for the development of successful therapies. In addition, current diagnostic approaches are often poorly effective. Thus, their therapeutic effects are limited [16]. For several years, progress in diagnosis and therapy has been searched by molecules, such as proteins and nucleotides, via the generation of biomarkers, specific in the diagnosis and possibly in the therapy of the diseases investigated. However, during their traffic and maintenance within the fluids, the molecules were extensively digested by proteases and ribonucleases. Thus, the attempts based on free proteins and nucleotides remained with limited success. The attempt changed considerably when the search for biomarkers started to be made by the use of EVs containing the molecules of interest within their lumen (Figure 1). Now it is clear that when segregated within EVs, the molecules are protected, making them suitable candidates for noninvasive biomarkers [16][17][18][16,17,18].
EVs are small vesicles of two types released by all cells. The first, widely called exosomes, are produced and accumulated within a vacuole of endosomal nature, the multivesicular body (MVB); the second, the ectosomes, are released by shedding of rafts, directly from the plasma membrane (Figure 1). Interestingly, the two EV types share similar properties. Their membranes are different from the two membranes of origin; their cargoes, segregated within their lumen, contain peculiar molecules, namely many proteins, many nucleotides, most often the noncoding miRNAs, lipids, and others. EVs of neuronal and astrocytic origin, when harvested from blood, can be used to interrogate brain pathologic processes. Moreover, in the case of proteins involved in the development of neurodegeneration, their segregation within EVs and even more their transfer to the fluids decrease the levels within the cells and can thus alter the disease progression [17].
Isolation from CSF or blood plasma of specific brain-cell-derived EVs, confirmed by neural markers [12], is theoretically simple. Thus, the approach has been successful recently and offers great promises for the near future [17][18][17,18]. The EVs, released by neurons, and astrocytes and microglia o of patients affected by neurodegenerative disease, can be identified by specific biomarkers found in their cargoes, such as Aβ and phosphorylated tau in AD, α-synuclein in PD, and the transactive response DNA/RNA binding protein of 43kDa (TDP-43) in ALS [13][19][20][21][22][13,19,20,21,22] (Table 1). Other biomarkers investigate the subclinical declines of the diseases, for example, the decline of middle age in AD. This can be done with tau and insulin signaling biomarkers [23][24][23,24]. A problem considered is that of multiple dementias, only some are connected to neurodegenerative diseases such as AD and PD. Among the proteins of EVs from specific neurodegenerative diseases, some have been recently shown to concern synaptic and axon injury, inflammations, stress responses and other defects [14][25][26][27][28][14,25,26,27,28]. Other dementias that are independent of neurodegenerative diseases still need identification of their specific biomarkers [29].
Table 1. Gene expression and disease specificity of proteins/biomarkers.
Genes | Proteins/Biomarkers | Diseases | ||||||
|---|---|---|---|---|---|---|---|---|
APP | amyloid precursor protein/Aβ * | AD | ||||||
PSEN1 | presenilin1 * | AD | ||||||
PSEN2 | presenilin2 | AD | ||||||
MAPT | tau * | AD, PD, DLB, FTD | ||||||
C9orf72 | C9orf72 * | FTD, ALS | ||||||
GRN | progranulin * | FTD, ALS | ||||||
VCP | valosin-containing protein * | ALS, FTD, PD | ||||||
TARDBP | TDP-43 * | ALS | ||||||
FUS | fused in sarcoma (FUS) | ALS | ||||||
HTT | huntingtin * | HD | ||||||
SNCA | α-synuclein * | PD, DLB, AD | ||||||
GBA | β-glucocerebrosidase | PD, DLB | ||||||
ApoE | apolipoprotein-E | AD (risk factor) | ||||||
TREM2 | TREM2 | AD (risk factor) |
In addition to many proteins, EVs include in their cargo various types of nucleotides, with predominance of miRNAs. The latter are members of a noncoding family involved in various functions, the best known being translational gene expression. Within fluids, miRNAs investigated have been numerous. Whether or not they play the role of biomarkers has been discussed. Positive evidence, analogous to that of proteins, has been recently reported but without precise identification of many miRNAs involved [30][31][32][33][30,31,32,33]. Interestingly, biomarkers of miRNA origin were shown active in the ALS disease [31]. Another positive conclusion has been found, but it concerns children, healthy and patients of their diseases [33]. Additional studies have focused on a new form of noncoding RNA, namely circular RNA (circRNA), known to traffic within EVs. At present, however, the function of these RNAs is unknown. CircRNAs might be involved in age-related diseases [34][35][34,35]. RNAs of this type may also operate in neuropsychiatric disorders [35].
4. AD and Its Multiple Fluid Biomarkers
AD is the neurodegenerative disease of greatest importance for two reasons, namely its much larger number of patients (at least 50 million worldwide) and the many scientists committed to its investigation. The choice of this disease has been made to illustrate its general properties. The task is to provide a current landscape, largely common to PD [21][29][36][21,29,36] but not always to other neurodegenerative diseases (see, for example, [9][17][28][31][32][9,17,28,31,32]).
A property common to many neurodegenerative diseases is heterogeneity. Various factors are considered as possible con-causes of its starting. Among these are oxidative stress, neural network dysfunctions, and defects in protein regulation and degradation. In the case of AD, two additional factors need to be considered, i.e., inflammation and immune dysregulation [37]. Such defects are expected to induce alterations in neurons, synapses, axons, and possibly also on glial cells. As already assumed in Section 3, some of these factors have been recognized by the identification of the corresponding biomarkers. For other defects, however, biomarkers are not available yet. Although incomplete, the present knowledge appears of interest to establish the properties of some AD heterogeneous forms, such as responses to treatments. The study of multiple biomarkers, identified during the last months, might be sufficient to characterize at clinical level various aspects of AD, including diagnosis and prognosis [38][39][40][38,39,40]. Heterogeneity exists also for tau. The fraction inducing tau biomarkers in the CSF was found to stage Alzheimer’s disease, and this is potentially useful for tau-directed therapeutics [41]. Other proteins, such as mesenchymal stem cells and exosomes, appear of considerable potential for therapy. The role of some other properties, including heterogeneity, remains to be established [42][43][42,43].
An additional approach relevant for AD diagnosis and therapy has been recently reported based on two different miRNAs that are active as EV biomarkers in the blood plasma. Although not identical, the evaluation of the two miRNAs could be considered in parallel. Effects in AD patients, induced by increased miRNA levels in the blood, were revealed by neuronal viability and neuroinflammation followed by a mini-mental state examination. Additional effects were investigated also in fluid, using well-known neural cells such as SH-SY5Y cells, affected by Aβ treatment and evaluated in terms of proliferation, apoptosis, and neuroinflammation. Interestingly, significant upregulation of the first miRNA, miR-485-3p, was shown in patients and cell models, accompanied by severity of DA in vivo and in fluid [44]. The response induced by the second miRNA, miR-331-3p, appears the opposite. Both in vivo and in fluid, the increased miRNA induced significant and persistent attenuation of AD [45]. The two types of results induced by these miRNA opened the possibility of new, promising therapies based on the two biomarkers investigated [44][45][44,45].
In conclusion, the actions by EV biomarkers based on multiple properties of proteins and miRNAs have recently offered ample chances of both nature and specificity, showing enormous potential as diagnostic, evaluation and treatment tools. Their new results allow researchers to test hypotheses by proof of concept studies at the preclinical phase, with further opportunities to develop therapeutic discoveries in neurodegenerative diseases [46].
