Gastrointestinal (GI) endoscopy is the gold standard in the detection and treatment of early and advanced GI cancers. However, conventional endoscopic techniques are technically demanding and require visual-spatial skills and significant hands-on experience. GI endoscopy simulators represent a valid solution to allow doctors to practice in a pre-clinical scenario.
- GI endoscopy
- medical simulation
- medical education
- training
- gastroscopy
- colonoscopy
- simulators
1. Introduction
Medical simulators are artificial platforms that offer the opportunity to train clinical procedures in a non-patient care environment. The first endoscopic simulator is dated back to 1969 and was made up of a simple mannequin for sigmoidoscopy training [1]. Over the following fifty years, the technology advancements led to the development of several artificial platforms, targeting the training of a wide range of endoscopic procedures, including both the upper and the lower gastrointestinal (GI) tracts. Ranging from purely mechanical systems to more complex mechatronic devices and animal-based models, nowadays, a variety of opportunities are available for practicing cognitive and motor skills in endoscopy. For this reason, the American Society for Gastrointestinal Endoscopy (ASGE) has encouraged the use of simulators for GI endoscopy training [2].
Mastering endoluminal procedures requires a high level of visuomotor coordination, cognitive learning, and technical capabilities acquired through hands-on experience. The standard training system includes the mentoring of the trainee by an expert endoscopist. In this context, the novice progressively learns to manage a procedure by first assisting the expert clinician and later directly practicing on the patient [3]. However, this system implies several drawbacks. First, since endoscopy usually involves only one operator at a time, the trainee practices the procedure independently, even if under the supervision of mentors. This could increase the risks of causing discomfort or injuries on the patient, given the lack of experience of the operator [4]. Studies have shown an increased frequency of minor adverse events related to trainee procedures associated with patient’s dissatisfaction [5]. Moreover, in this context, if the novice encounters difficulties, the expert takes over the procedure, depriving the trainee of learning the specific task. Finally, this learning model leads to an increase of the length of the medical operation, negatively impacting on the costs and potentially prolonging the discomfort of the patient [4].
By contrast, simulators provide a risk-free solution for acquiring global competencies in medical practices at the trainee’s pace. Accordingly, as opposed to standard mentored supervision, simulation-based training allows trainees to repeatedly perform a specific set of skills without increasing the length of the clinical procedures and/or reducing the patient’s comfort and safety. Besides, these platforms could allow the standardization of the endoscopy related metrics and the assessment of technical skills [4,6][4][6]. This is particularly important for endoscopy since the outcome of the procedure is highly dependent on the skills and the experience of the operator [7,8][7][8]. Hence, the introduction of simulators in training programs would lead to evidence of the acquisition of the minimum competencies by the clinicians before operating on the patients [3,9][3][9]. In this context, the simulators would not only assess the minimum skills for trainees but could also serve to prove the maintenance of those skills to always guarantee high-quality patient care.
In the last decades, various studies have estimated the minimum number of procedures needed to achieve competence in GI endoscopy. These values range from 100–300 for colonoscopy [10,11][10][11] and around 200 for gastroscopy [12]. In this context, simulation-based training could reduce this number, speeding up the learning curve of the trainee [9].
2. Conventional/Standard simulators for training
Over the years, several types of simulators for GI endoscopy training have been developed. Starting from the tests on animal models, technological progress enabled the development of the current generation of advanced devices. In particular, the training platforms for GI endoscopy can be classified, according to the technology adopted, into i) physical simulators, ii) computerized simulators, and iii) animal models. The last category can be further differentiated into
in-vivo
and
ex-vivo
cases.
2.1 Mechanical simulators
Mechanical simulators (
i.e.,
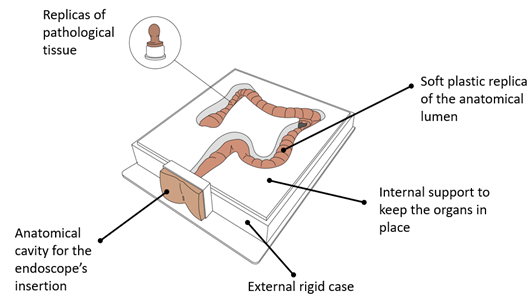
physical simulators), reproduce anatomical organs using a combination of soft and hard materials (
e.g., silicone). In such cases, cavities inside the replicated phantoms allow the insertion of a standard endoscope, mimicking the endoscopic procedure (See Figure 1). Consequently, the physical simulators aim at reproducing, with high fidelity, the mechanical and visual properties of the GI tract, focusing on an accurate selection of the appropriate materials, molds and surface textures. Even having the intrinsic advantage of providing natural tactile feedback, unfortunately, each platform offers only a limited set of training procedures, since each scenario needs to be physically reproduced. For this reason, the mechanical simulators are only suitable for early-stage training of GI endoscopy [19] .
silicone). In such cases, cavities inside the replicated phantoms allow the insertion of a standard endoscope, mimicking the endoscopic procedure (See Figure 1). Consequently, the physical simulators aim at reproducing, with high fidelity, the mechanical and visual properties of the GI tract, focusing on an accurate selection of the appropriate materials, molds and surface textures. Even having the intrinsic advantage of providing natural tactile feedback, unfortunately, each platform offers only a limited set of training procedures, since each scenario needs to be physically reproduced. For this reason, the mechanical simulators are only suitable for early-stage training of GI endoscopy [13].
Figure 1. Mechanical simulators for GI endoscopy: main components.
2.2 Computerized simulators for GI endoscopy
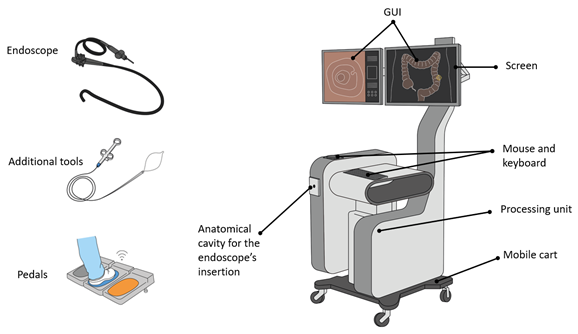
Considering what is accessible on the market, and besides mechanical simulators, another class of GI endoscopy training platforms are worth discussing. These devices, classified as computerized simulators (
i.e.,
Virtual Reality simulators), are mechatronic systems which combine standard endoscope handling, with virtual intraluminal scenarios. With that, it is possible to simulate a wide variety of endoscopic procedures and interventions (
e.g.,
gastroscopy, colonoscopy, polypectomy, bleeding control,
etc.). Thanks to these platforms, the movements of a physical endoscope are mapped in a virtual environment, reproducing the endoluminal view with endoscopic images [18] (See Figure 2). Having a wide variety of simulated cases, in addition to the opportunity of reproducing the same scenarios for all the trainees, is a great advantage for standardizing any type of training. All the platforms provide objective measurements of the quality of the performance such as the patient's pain level, the percentage of mucosa visualized, the time of the examination and the amount of air insufflated. This information allows tracking the learning curve of the users, as well as customizing the benchmarks for the assessment of the capabilities of individual trainees.
). Thanks to these platforms, the movements of a physical endoscope are mapped in a virtual environment, reproducing the endoluminal view with endoscopic images [14] (See Figure 2). Having a wide variety of simulated cases, in addition to the opportunity of reproducing the same scenarios for all the trainees, is a great advantage for standardizing any type of training. All the platforms provide objective measurements of the quality of the performance such as the patient's pain level, the percentage of mucosa visualized, the time of the examination and the amount of air insufflated. This information allows tracking the learning curve of the users, as well as customizing the benchmarks for the assessment of the capabilities of individual trainees.
Figure 2. Computerized simulators for GI endoscopy: main components.
2.3 . Animal models
Animal models have been widely exploited for training in medical procedures. For endoscopic applications, the literature dates the first ERCP simulation on a live canine model in 1974 [31]. Overall, both live animals and explanted organs have been used for practicing in GI endoscopic procedures. However, high costs and ethical concerns related to the
Animal models have been widely exploited for training in medical procedures. For endoscopic applications, the literature dates the first ERCP simulation on a live canine model in 1974 [15]. Overall, both live animals and explanted organs have been used for practicing in GI endoscopic procedures. However, high costs and ethical concerns related to the
in-vivo
cases, and the logistic issues in collecting and storing
ex-vivo specimens, limit their use. As a matter of fact, animals are mainly adopted for advanced training in therapeutic procedures, and for reproducing complex techniques such as hemostasis [32,33], EUS [34–37], ERCP [38,39] and ESD [40–44].
specimens, limit their use. As a matter of fact, animals are mainly adopted for advanced training in therapeutic procedures, and for reproducing complex techniques such as hemostasis [16][17], EUS [18][19][20][21], ERCP [22][23] and ESD [24][25][26][27][28].
References
- Hd, M. A New System for Teaching Proctosigmoidoscopic Morphology. Am. J. Gastroenterol. 1969, 52, 65–69.
- Cohen, J.; Bosworth, B.P.; Chak, A.; Dunkin, B.J.; Early, D.S.; Gerson, L.B.; Hawes, R.H.; Haycock, A.V.; Hochberger, J.H.; Hwang, J.H.; et al. Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) on the Use of Endoscopy Simulators for Training and Assessing Skill. Gastrointest. Endosc. 2012, 76, 471–475.
- Adler, D.G.; Bakis, G.; Coyle, W.J.; Degregorio, B.; Dua, K.S.; Lee, L.S.; McHenry, L.; Pais, S.A.; Rajan, E.; Sedlack, R.E.; et al. Principles of Training in GI Endoscopy. Gastrointest. Endosc. 2012, 75, 231–235.
- Sedlack, R.E. The State of Simulation in Endoscopy Education: Continuing to Advance toward Our Goals. Gastroenterology 2013, 144, 9–12.
- Bini, E.J.; Firoozi, B.; Choung, R.J.; Ali, E.M.; Osman, M.; Weinshel, E.H. Systematic Evaluation of Complications Related to Endoscopy in a Training Setting: A Prospective 30-Day Outcomes Study. Gastrointest. Endosc. 2003, 57, 8–16.
- Khan, R.; Plahouras, J.; Johnston, B.C.; Scaffidi, M.A.; Grover, S.C.; Walsh, C.M. Virtual Reality Simulation Training for Health Professions Trainees in Gastrointestinal Endoscopy. Cochrane Database Syst. Rev. 2018, 2018.
- Chen, S.C.; Rex, D.K. Endoscopist Can Be More Powerful than Age and Male Gender in Predicting Adenoma Detection at Colonoscopy. Am. J. Gastroenterol. 2007, 102, 856–861.
- Barclay, R.L.; Vicari, J.J.; Doughty, A.S.; Johanson, J.F.; Greenlaw, R.L. Colonoscopic Withdrawal Times and Adenoma Detection during Screening Colonoscopy. N. Engl. J. Med. 2006, 355, 2533–2541.
- Siau, K.; Hawkes, N.D.; Dunckley, P. Training in Endoscopy. Curr. Treat. Options Gastroenterol. 2018, 16, 345–361.
- Ekkelenkamp, V.E.; Koch, A.D.; De Man, R.A.; Kuipers, E.J. Training and Competence Assessment in GI Endoscopy: A Systematic Review. Gut 2016, 65, 607–615.
- Ward, S.T.; Mohammed, M.A.; Walt, R.; Valori, R.; Ismail, T.; Dunckley, P. An Analysis of the Learning Curve to Achieve Competency at Colonoscopy Using the JETS Database. Gut 2014, 63, 1746–1754.
- Ward, S.T.; Hancox, A.; Mohammed, M.A.; Ismail, T.; Griffiths, E.A.; Valori, R.; Dunckley, P. The Learning Curve to Achieve Satisfactory Completion Rates in Upper GI Endoscopy: An Analysis of a National Training Database. Gut 2017, 66, 1022–1030.
- Gerson, L.B.; Van Dam, J. Technology Review: The Use of Simulators for Training in GI Endoscopy. Gastrointest. Endosc. 2004, 60, 992–1001.
- Triantafyllou, K. Virtual Reality Simulators for Gastrointestinal Endoscopy Training. World J. Gastrointest. Endosc. 2014, 6, 6–12.
- 3D Colonoscope Training Simulator NKS. KYOTO KAGAKU. Available online: https://www.kyotokagaku.com/en/products_data/mw24/ (accessed on 10 March 2021).
- Colonoscopy (Lower GI Endoscopy) Simulator Type II LM-107: KOKEN CO.,LTD. Available online: https://www.kokenmpc.co.jp/english/products/life_simulation_models/medical_education/lm-107/index.html (accessed on 10 March 2021).
- EGD (EsophagoGastroDuodenoscopy) Simulator LM-103: KOKEN CO.,LTD. Available online: https://www.kokenmpc.co.jp/english/products/life_simulation_models/medical_education/lm-103/index.html (accessed on 10 March 2021).
- Noar, M.D. Robotics Interactive Endoscopy Simulation of ERCP/Sphincterotomy and EGD. In Endoscopy; Endoscopy: Thieme, Stuttgart, Germany, 1992; Volume 24, pp. 539–541.
- Williams, C.B.; Baillie, J.; Gillies, D.F.; Borislow, D.; Cotton, P.B. Teaching Gastrointestinal Endoscopy by Computer Simulation: A Prototype for Colonoscopy and ERCP. Gastrointest. Endosc. 1990, 36, 49–54.
- GI Mentor. Simbionix. Available online: https://simbionix.com/simulators/gi-mentor/ (accessed on 7 August 2020).
- EndoVR Endoscopy Training Simulator. CAE Healthcare. Available online: https://caehealthcare.com/surgical-simulation/endovr/ (accessed on 7 August 2020).
- EndoSim VR laparoscopic. EndoSim®. Surgical Science. Available online: https://surgicalscience.com/systems/endosim/?gclid=CjwKCAjw97P5BRBQEiwAGflV6YvrWL9WGSHmdOvKUTidTGsVugPUBzQ5Ov6DmXxl7E0RQKb_2Iq6XRoCnlMQAvD_BwE (accessed on 7 August 2020).
- MedVision. Available online: https://www.medvisiongroup.com/endovision.html (accessed on 7 August 2020).
- ENDO-X-MEDICAL-X-PDF Catalogs. Technical Documentation. Available online: https://pdf.medicalexpo.com/pdf/medical-x/endo-x/112986-160332.html (accessed on 10 March 2021).
- Simulators for Healthcare Training. Medical-X. Available online: https://medical-x.com/ (accessed on 10 March 2021).
- Haycock, A.; Koch, A.D.; Familiari, P.; van Delft, F.; Dekker, E.; Petruzziello, L.; Haringsma, J.; Thomas-Gibson, S. Training and Transfer of Colonoscopy Skills: A Multinational, Randomized, Blinded, Controlled Trial of Simulator versus Bedside Training. Gastrointest. Endosc. 2010, 71, 298–307.
- GI Mentor Platforms. Simbionix. Available online: https://simbionix.com/simulators/gi-mentor/gi-mentor/ (accessed on 10 March 2021).
- Falkenstein, D.B.; Abrams, R.M.; Kessler, R.E.; Jones, B.; Johnson, G.; Zimmon, D.S. Endoscopic Retrograde Cholangiopancreatography in the Dog: A Model for Training and Research. Gastrointest. Endosc. 1974, 21, 25–26.