Orthodontics is a branch of dentistry dealing with the improvement of occlusal conditions and facial aesthetics in both children and adults.
- nanomaterials
- orthodontics
- brackets
- wires
- antimicrobial effect
1. Introduction
Nanomaterials are widely used in modern clinical dentistry. They improve various properties, such as antimicrobial properties, durability of materials. These particles do not exceed 100 nm, due to they obtain a better ratio between the surface and mass. The larger the surface area of the material, the greater its reactivity. It is also easier to absorb them in the body, which can also result in high cytotoxicity [1]. Nanomaterials are used in many areas of dentistry, such as conservative dentistry, endodontics, oral, and maxillofacial surgery, periodontics, orthodontics, and prosthetics [2]. Orthodontics is a branch of dentistry dealing with the improvement of occlusal conditions and facial aesthetics in both children and adults. In cooperation with other specialists (such as dental surgeons, maxillofacial surgeons, periodontists), the orthodontist is able to significantly improve the patient’s quality of life [3]. Nanotechnology is used, among others, in brackets, archives, elastomeric ligatures, orthodontic adhesives. Improving the microbicidal properties, reducing friction and increasing the strength of the material are some of the advantages. However, a significant problem is the potential cytotoxicity of nanomaterials, therefore further research is needed [2].
The prolonged process of wearing orthodontic braces results in increased accumulation of dental plaque and eventually results in a greater risk of caries. Its development is generally associated with the activity of cariogenous bacteria due to prolonged dental plaque accumulation on teeth surfaces, deficiencies, avitaminosis, and diet. The demineralization process that starts the caries is called a white spot lesion (WSL), meaning, that decalcification of enamel surfaces adjacent to the orthodontic appliances is directly associated with orthodontic treatment [4]. Several studies confirm the accelerated accumulation of WLS in orthodontic treatments. Such tendency creates clinical problems leading to unacceptable esthetic alterations that, in some cases, might lead to conservative, restorative treatment. Research shows that more plaque can accumulate around composites compared to other restorative materials, which results in an increased percentage of secondary caries [5]. Moreover, resin composites do not have bacteriostatic properties.
Promising results in the prevention of pathological changes associated with orthodontic treatment are obtained through the use of nanotechnology. According to the European Commission states that: “Nanomaterial is defined as a natural, incidental, or manufactured material containing particles, in an unbound state or as an aggregate or as an agglomerate and where, for 50% or more of the particles in the number size distribution, one or more external dimensions is in the size range 1–100 nm. In specific cases and where warranted by concerns for the environment, health, safety, or competitiveness the number size distribution threshold of 50% may be replaced by a threshold between 1% and 50%” [6]. Implication of nanotechnology is beneficial to humans, it has been broadly used in the modern dentistry in in restorative dentistry as an additive nanoparticle with remineralizing properties in composite resins, dental adhesives, oral care products, in the control of bacterial biofilm as an antibacterial and antimineralizing additive in dental hygiene products such as toothpaste, mouth rinses, and composite resins. Nanotechnology is useful in the diagnosis of malignant and precancerous cavity diseases, periodontal diseases, and is also used in implantology—as a modification of the implant surface [7] and in the use of impression materials [8]. The development of technology gives better opportunities to both patient and orthodontist due to new physicochemical, mechanical and antibacterial properties of nanosized materials and can be used in coating orthodontic wires, elastomeric ligatures, and brackets, producing shape memory polymers and orthodontic bonding materials. Not only can we control biofilm formation, reduce bacterial activity and act anticariogenic, but also, through the desired tooth movement, shorten the treatment time.
2. Nano-Coatings in Orthodontic Archwires
Minimizing the frictional forces between the orthodontic wire and brackets has the potential to increase the desired tooth movement and thus shorten treatment time. In recent years, nanoparticles have been used as a component of dry lubricants. These solid-phase materials are capable of reducing the friction between two sliding surfaces without the need for a liquid medium. One of the many examples are Inorganic fullerene-like tungsten sulfide nanoparticles (IF-WS2) that are used as self-lubricating coatings for orthodontic stainless steel wires [9]. Friction tests simulating the performance of coated and uncoated wires were carried out on an Instron machine, scanning electron microscopy (SEM) and energy dispersive X-ray spectroscopy (EDS) analysis of the coated wires showed a clear impregnation of IF-WS2 nanoparticles in the Ni-P matrix.
Atomic force microscopy (AFM) was used as a tool to assess the surface roughness of stainless steel (SS), beta-titanium (β-Ti), and nickel-titanium(NiTi) wires [10]. The surface roughness measurement of the AFM method confirmed the fact that the roughness of the measures on the effectiveness of sliding mechanics, the corrosion behavior, and aesthetics of orthodontic arches. The influence of decontamination and clinical exposure on the modulus of elasticity, hardness and surface roughness of SS and NiTi arches, and AFM paper coupled with a nanoindenter were assessed [11]. The results of the AFM popularity assessment that the decontamination regimen and clinical exposure had no statistically significant effect on NiTi wires, but had a statistically significant effect on SS wires. In a diagnostic study, the clinical significance of statistical studies, analysis, and testing of the arch equipment on orthodontic movement is not predicted.
2.1. Nano Coatings Reducing Friction on Orthodontic Archwires
Orthodontic arches are used to generate biomechanical forces that are transmitted through the brackets to move the teeth and correct malocclusion, spacing, or crowding. They are also used for retention purposes, i.e., to keep the teeth in their current position. Currently, orthodontic arches are made of non-precious metal alloys. The most common types of wire are SS, NiTi, and β-Ti alloy wires. In the case of sliding mechanics, friction between the wire and the lock is one of the major factors influencing tooth movement. When one moving object makes contact with another, friction occurs on the contact surface, which causes resistance to the movement of the teeth. This frictional force is proportional to the force with which the contacting surfaces are pressed against each other and is governed by the interface surface characteristics (smooth/rough, chemically reactive/passive, or lubricant modified). Minimizing the frictional forces between the orthodontic wire and brackets will accelerate the desired tooth movement and thus shorten the treatment time.
NiTi substrates can be coated with cobalt and a layer of IF-WS2 nanoparticles using the electrodeposition method. The coated substrates showed friction reduction of up to 66% when compared to the uncoated ones. The results of such studies may have potential applications in reducing friction when using NiTi orthodontic wires. On the other hand, allergic reactions in patients with nickel sensitivity may be the disadvantage of introducing nickel into this type of coating. Therefore, the effect of such NiP coatings on stainless steel and NiTi wires should be assessed for biocompatibility in animal models and further human trials.
2.2. Delivering Nanoparticles from an Elastomeric Ligature
Elastomeric ligatures can serve as a support scaffold to deliver nanoparticles that can be anti-cariogenic or anti-inflammatory. They may also carry embedded antibiotic drug molecules. The release of anti-cariogenic fluoride from elastomeric ligatures has already been described in the literature [12,13][12][13]. Research has shown that fluoride release is characterized by an initial burst of fluoride in the first few days followed by a logarithmic fall. The whole process is effective against common enamel demineralization around the orthodontic bracket during treatment [14].
2.3. Shape Memory Polymers (SMP) in Orthodontics
In the last decade, there has been a growing interest in the production of aesthetic orthodontic wires to complement brackets in the color of the teeth. Shape memory polymers (SMPs) are materials that can remember equilibrium shapes and then manipulate and fix them into a temporary or dormant shape under certain temperature and stress conditions. They can later relax to their original, stress-free state under thermal, electrical, or environmental conditions. This relaxation is related to the elastic deformation stored in the previous manipulation. Recovery of SMP into equilibrium shape can be accompanied by an appropriate and prescribed force, useful for orthodontic tooth movement, or a macroscopic change in shape that is useful in ligation mechanisms. Due to the ability of SMP to have two shapes, these devices meet requirements unattainable by modern orthodontic materials, allowing the orthodontist to insert them into the patient’s mouth more easily and comfortably [15].
When placed in the oral cavity, these polymers can be activated by body temperature or light-activated photoactive nanoparticles thereby causing tooth movement. SMP orthodontic wires can provide an improvement over traditional orthodontic materials as they provide lighter, more consistent forces which, in turn, can cause less pain to patients. Also, SMP materials are transparent, stainable, and stain-resistant, providing the patient with a more aesthetic apparatus during treatment. High percent elongation of the SMP apparatus (up to about 300%) allows for the application of continuous forces over a large range of tooth movement, and thus, fewer patient visits [16,17][16][17]. Future directions of research on shape—nanocomposite polymers with memory for the production of aesthetic orthodontic wires may have interesting potential in the research of orthodontic biomaterials.
2.4. Control of Oral Biofilms during Orthodontic Treatment
Nanoparticles have a larger surface area to volume ratio (per unit mass) compared to non-nano scale particles, interacting more closely with microbial membranes and providing a much larger surface area for antimicrobial activity. In particular, metal nanoparticles with a size of 1–10 nm showed the highest biocidal effect on bacteria [18]. Silver has a long history of use in medicine as an antibacterial agent [19]. The antimicrobial properties of nanoparticles have been exploited through the mechanism of joining dental materials with nanoparticles or coating the surface with nanoparticles to prevent adhesion of microbes to reduce biofilm formation [20,21][20][21]. It was found that resin composites containing fillers implanted with silver ions that release silver ions have an antibacterial effect on oral streptococci [22].
Ahn et al. [16] compared an experimental composite adhesive (ECA) containing silica nanofillers and silver nanoparticles with two conventional composite adhesives and a resin-modified glass ionomer (RMGI) to investigate the surface characteristics, physical properties, and antimicrobial activity against cariogenic streptococci. The results suggest that the ECAs had rougher surfaces than conventional adhesives due to the addition of silver nanoparticles. Bacterial adhesion to ECA was lower than to traditional adhesives, which was not affected by saliva. Bacterial suspensions containing ECA show slower growth of bacteria than those containing conventional adhesives. There is no significant difference in the shear bond strength and fracture strength of the bond between ECA and conventional adhesives.
3. Nanomaterials in Orthodontics
Nanomaterials versatility allows them to be used in many situations during orthodontic clinical treatment, as can be seen in Table 1.
Table 1. Nanomaterials application in dentistry.
| Nanomaterial | Method of Use | Application | References | |||
|---|---|---|---|---|---|---|
| Silver NPs (AgNPs) | Applied as a coating agent on titanium | Implants | [40,41] | [23][24] | ||
| Zinc oxide NPs (ZnONPs) | Incorporated into dental resins | Resin composite adhesives | [42,43] | [25][26] | ||
| Chitosan NPs | Conjugated with silver nanoparticles | Resin composites adhesives | [44,45] | [27][28] | ||
| Copper (I) oxide NPs (Cu | 2 | ONPs) | Antimicrobial effect in resin adhesives | Resin composites adhesives | [46] | [29] |
| Titanium (IV) oxide NPs (TiO | 2 | NPs) | Nanotubes on titanium surfaces and incorporated with ZnONPs | Implants | [47,48] | [30][31] |
| Gold NPs (AuNPs) | Modified gold nanoparticles (AuDAPT) coated onto orthodontic aligners | Antimicrobial coated aligner | [49] | [32] | ||
| Carbonate hydroxyapatite nanocrystal | Antibacterial and antidemineralizing properties | Toothpastes, mouthwashes and composite resins | [50] | [33] | ||
| Amorphous Calcium Phosphate (ACP) | Antibacterial and antidemineralizing properties | Antibacterial and antidemineralizing properties | [51] | [34] | ||
| Novel Poly(l-lactic acid) (PLLA)/Multi-walled carbon nanotubes (MWNTs)/hydroxyapatite (HA) nanofibrous scaffolds | Polymer solution FOR entire-tooth regeneration |
Dental Surface applications | [52] | [35] | ||
| Bioactive peptide—Amphiphile nanofibers | Branched peptide Amphiphile molecules containing the peptide motif Arg-Gly-Asp, or “RGD” |
Dental surface applications | [53] | [36] |
Friction is one of the major factors present during retraction or alignment of teeth during orthodontic treatment. One of the methods to overcome high friction is the application of higher forces during treatment. Such action can have one significant disadvantage- undesirable anchorage loss [54][37]. On the other hand, there are other methods of overcoming unwanted friction, including alteration of the bracket design or wire shape and size. At last, there is a possibility of nanoparticle coating addition. To benefit from the antibacterial properties of nanoparticles, there are two main strategies in orthodontics to reduce biofilm formation. One strategy focuses on coating the surface of orthodontic brackets or wires with nanoparticles [55][38]. The other is about combining nanoparticles with orthodontic adhesives or acrylic materials. The advantages of nanocomposite materials include excellent optical properties, easy handling, and excellent polishability [24][39]. Moreover, nanofillers can reduce the surface roughness of orthodontic adhesives, which is one of the most important factors in bacterial adhesion [25][40], as can be seen in Figure 2.
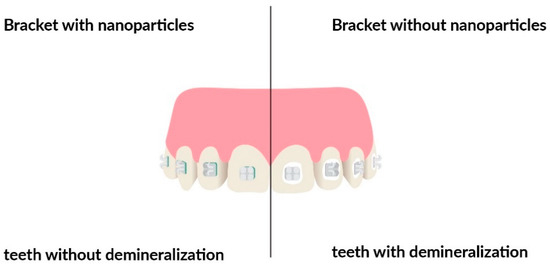
Figure 2. Comparison of teeth demineralization development with and without nanoparticles’ covered brackets.
3.1. Silver Nanoparticles (AgNPs) Coating
Some studies have proposed silver nanoparticles as the most effective type of metal nanoparticles for preventing the growth of Streptococcus mutans [56][41]. Recently, silver nanoparticles (AgNPs) have been shown to be materials with excellent anti-microbial properties in a wide variety of microorganisms. In the orthodontic field, studies have incorporated AgNPs (17 nm) into orthodontic elastomeric modules, orthodontic brackets, and wires, and others, against a wide variety of bacterial species concluding that these orthodontic appliances with AgNPs could potentially combat the dental biofilm decreasing the incidence of dental enamel demineralization during and after the orthodontic treatments [57,58][42][43]. AgNPs can significantly inhibit the bacterial adherence of the S. mutans strain on the surfaces of the orthodontic bracket and wire appliances finding that the smaller AgNP samples demonstrated statistically to have the most important S. mutans antiadherence activities for orthodontic brackets and wires when compared to NiTi (nickel–titanium) and SS (stainless steel wires) [59][44]. It is also confirmed by several studies, that coverage of AgNPs in human dentin prevents biofilm formation on the surface of the dentin, together with bacterial growth inhibition [58,60,61][43][45][46]. In order for AGNPs to be a stable suspension able to limit the agglomeration, they should have zeta potential values ranging between +30 and −30 mV [62,63][47][48]. Bürgers et al. [64][49] confirms, that smaller AgNPs have the ability to release more silver ions, which promotes their antimicrobial effect, while the histological effect of AgNPs generally focuses on inhibition of microbial metabolism, leading to impaired production of extracellular polysaccharides and specific bacterial processes leading to its general dysfunction [65][50]. These studies confirm, that AgNP-coated brackets can help to decrease the spot lesions appearance during orthodontic treatment, and may be even useful in compromised patients with immune deficiency, diabetes, or elevated risk of endocarditis [66][51]. In addition to silver, many other nanoparticles like chitosan, copper, zinc, hydroxyapatite, and silicon dioxide can be added to composites in order to reduce bacterial activity and growth.
3.2. Chitosan
Chitosan is a naturally acquired polysaccharide that is formed by the deacetylation of chitin. It is a non-toxic, biodegradable, biocompatible, and has antibacterial properties [67][52], on Agregatibacter actinomycetemcomitans, Porphyromonas Gingivalis, and Streptococcus mutans [68,69][53][54]. Chitosan additionally has inhibiting action against fungi. This material’s application as an antibacterial chemical agent in mouthwashes is limited due to its reduced solubility in water. Nonetheless, its characteristics are highly desirable in dental materials. Chitosan could be maintained inside the materials in the oral cavity due to its insolubility in water. Histologically, inhibition is caused by inactivation of the enzyme, the substitution of lipopolysaccharides, metal ions, and formation of acidic polymer like teichoic acid. Chitosan, due to its low solubility and melting temperature, can be maintained in the oral cavity for a long period of time, unlike CHX which is released and disappears in the early phase.
3.3. Copper Oxide
It was proved by Yassaei et al. [70][55], that no significant difference was found between silver and copper oxide (CuO) nanoparticles, but it was noted that a curing time increased with the use of copper material when compared to the silver one. The former is cheaper and additionally both physically and chemically more stable than the latter. CuO nanoparticles affect Streptococcus mutans bacteria in a similar way as silver particles do [56][41]. It was confirmed in other studies [4], that copper and copper-zinc nanoparticles had a significant inhibitory effect on the studied microbes. According to other studies, CuO is able to decrease biofilm formation from 70 up to 80% [71][56]. Moreover, the similar results were achieved when CuO particles were incorporated into adhesive materials [72][57]. Additionally, nanoparticles like CuO can act as nano-fillers and enhance the shear bond strength of adhesive.
3.4. Nitrogen-Doped Titanium Dioxide (N-Doped TiO2) Brackets
The activation of N-doped TiO2 leads to the formation of OH. Free radicals, superoxide ions (O2), hydrogen peroxide (H2O2), and peroxyl radicals (HO2). These chemicals exert antimicrobial activity, also reacting with lipids, enzymes, and proteins. According to Poosti et al. [73][58], TiO2 nanoparticles of size 21 ± 5 nm can be blended to light cure orthodontic composite paste in 1, 2, and 3% and all these concentrations have similar antibacterial effects. Salehi et al. [74][59] proved, that nitrogen-doped TiO2 brackets have shown better antimicrobial activity when compared to the uncoated stainless steel brackets. Adding TiO2 to adhesives enhances its antibacterial activity without compromising its mechanical properties [75][60]. Nitrogen-doped TiO2 brackets were also reported to present antibacterial activity against normal oral pathogenic bacteria [76][61].
3.5. Zinc Oxide (ZnO)
It has been observed, that as the concentration of ZnO increases, the antimicrobial activity also increases, followed by shear bond strength reduction. It is important to underline, that ZnO and CuO coated brackets have been observed with better antimi-crobial characteristics on Streptococcus mutans than when the brackets were coated with CuO nanoparticles alone [77][62]. Kachoei et al. [78][63], Behroozian et al. [79][64] and Goto et al. [80][65] proved, that following ZnO nanoparticle coating, the frictional forces be-tween archwires and brackets significantly decreased. Because of that effect, these na-noparticles offer new opportunities in overcoming the unwanted friction forces, better anchorage control, and reduced risk of resorption.
References
- Song, W.; Ge, S. Application of Antimicrobial Nanoparticles in Dentistry. Molecules 2019, 24, 1033.
- Sharan, J.; Singh, S.; Lale, S.V.; Mishra, M.; Koul, V.; Kharbanda, O.P. Applications of nanomaterials in dental science: A review. J. Nanosci. Nanotechnol. 2017, 17, 2235–2255.
- Gkantidis, N.; Christou, P.; Topouzelis, N. The orthodontic-periodontic interrelationship in integrated treatment challenges: A systematic review. J. Oral Rehabil. 2010, 37, 377–390.
- Behnaz, M.; Dalaie, K.; Mirmohammadsadeghi, H.; Salehi, H.; Rakhshan, V.; Aslani, F. Shear bond strength and adhesive remnant index of orthodontic brackets bonded to enamel using adhesive systems mixed with tio 2 nanoparticles. Dental Press J. Orthod. 2018, 23, 43.e1–43.e7.
- Sevinç, B.A.; Hanley, L. Antibacterial activity of dental composites containing zinc oxide nanoparticles. J. Biomed. Mater. Res. Part B Appl. Biomater. 2010, 94, 22–31.
- Boverhof, D.R.; Bramante, C.M.; Butala, J.H.; Clancy, S.F.; Lafranconi, W.M.; West, J.; Gordon, S.C. Comparative assessment of nanomaterial definitions and safety evaluation considerations. Regul. Toxicol. Pharmacol. 2015, 73, 137–150.
- Chieruzzi, M.; Pagano, S.; Moretti, S.; Pinna, R.; Milia, E.; Torre, L.; Eramo, S. Nanomaterials for tissue engineering in dentistry. Nanomaterials 2016, 6, 134.
- Feng, X.; Chen, A.; Zhang, Y.; Wang, J.; Shao, L.; Wei, L. Application of dental nanomaterials: Potential toxicity to the central nervous system. Int. J. Nanomed. 2015, 10, 3547–3565.
- Redlich, M.; Katz, A.; Rapoport, L.; Wagner, H.D.; Feldman, Y.; Tenne, R. Improved orthodontic stainless steel wires coated with inorganic fullerene-like nanoparticles of WS2 impregnated in electroless nickel-phosphorous film. Dent. Mater. 2008, 24, 1640–1646.
- Bourauel, C.; Fries, T.; Drescher, D.; Plietsch, R. Surface roughness of orthodontic wires via atomic force microscopy, laser specular reflectance, and profilometry. Eur. J. Orthod. 1998, 20, 79–92.
- Alcock, J.P.; Barbour, M.E.; Sandy, J.R.; Ireland, A.J. Nanoindentation of orthodontic archwires: The effect of decontamination and clinical use on hardness, elastic modulus and surface roughness. Dent. Mater. 2009, 25, 1039–1043.
- Doherty, U.B.; Benson, P.E.; Higham, S.M. Fluoride-releasing elastomeric ligatures assessed with the in situ caries model. Eur. J. Orthod. 2002, 24, 371–378.
- Miura, K.K.; Ito, I.Y.; Enoki, C.; Elias, A.M.; Matsumoto, M.A.N. Anticariogenic effect of fluoride-releasing elastomers in orthodontic patients. Braz. Oral Res. 2007, 21, 228–233.
- Nalbantgil, D.; Oztoprak, M.O.; Cakan, D.G.; Bozkurt, K.; Arun, T. Prevention of demineralization around orthodontic brackets using two different fluoride varnishes. Eur. J. Dent. 2013, 7, 41–47.
- Jung, Y.C.; Cho, J.W. Application of shape memory polyurethane in orthodontic. J. Mater. Sci. Mater. Med. 2010, 21, 2881–2886.
- Meng, Q.; Hu, J. A review of shape memory polymer composites and blends. Compos. Part A Appl. Sci. Manuf. 2009, 40, 1661–1672.
- Leng, J.; Lan, X.; Liu, Y.; Du, S. Shape-memory polymers and their composites: Stimulus methods and applications. Prog. Mater. Sci. 2011, 56, 1077–1135.
- Allaker, R.P. Critical review in oral biology & medicine: The use of nanoparticles to control oral biofilm formation. J. Dent. Res. 2010, 89, 1175–1186.
- Hill, W. Argyria; the Pharmacology of Silver; The Williams & Wilkins Company: Baltimore, MD, USA, 1939.
- Moolya, N.; Sharma, R.; Shetty, A.; Gupta, N.; Gupta, A.; Jalan, V. Orthodontic bracket designs and their impact on microbial profile and periodontal disease: A clinical trial. J. Orthod. Sci. 2014, 3, 125.
- Monteiro, D.R.; Gorup, L.F.; Takamiya, A.S.; Ruvollo-Filho, A.C.; de Camargo, E.R.; Barbosa, D.B. The growing importance of materials that prevent microbial adhesion: Antimicrobial effect of medical devices containing silver. Int. J. Antimicrob. Agents 2009, 34, 103–110.
- Yamamoto, K.; Ohashi, S.; Aono, M.; Kokubo, T.; Yamada, I.; Yamauchi, J. Antibacterial activity of silver ions implanted in SiO2 filler on oral streptococci. Dent. Mater. 1996, 12, 227–229.
- Venugopal, A.; Muthuchamy, N.; Tejani, H.; Anantha-Iyenga-Gopalan; Lee, K.P.; Lee, H.J.; Kyung, H.M. Incorporation of silver nanoparticles on the surface of orthodontic microimplants to achieve antimicrobial properties. Korean J. Orthod. 2017, 47, 3–10.
- Padovani, G.C.; Feitosa, V.P.; Sauro, S.; Tay, F.R.; Durán, G.; Paula, A.J.; Durán, N. Advances in Dental Materials through Nanotechnology: Facts, Perspectives and Toxicological Aspects. Trends Biotechnol. 2015, 33, 621–636.
- Kasraei, S.; Sami, L.; Hendi, S.; AliKhani, M.-Y.; Rezaei-Soufi, L.; Khamverdi, Z. Antibacterial properties of composite resins incorporating silver and zinc oxide nanoparticles on Streptococcus mutans and Lactobacillus. Restor. Dent. Endod. 2014, 39, 109.
- Arun, D.; Adikari Mudiyanselage, D.; Gulam Mohamed, R.; Liddell, M.; Monsur Hassan, N.M.; Sharma, D. Does the Addition of Zinc Oxide Nanoparticles Improve the Antibacterial Properties of Direct Dental Composite Resins? A Systematic Review. Materials (Basel) 2020, 14, 40.
- Targino, A.G.R.; Flores, M.A.P.; Dos Santos, V.E.; De Godoy Bené Bezerra, F.; De Luna Freire, H.; Galembeck, A.; Rosenblatt, A. An innovative approach to treating dental decay in children. A new anti-caries agent. J. Mater. Sci. Mater. Med. 2014, 25, 2041–2047.
- Kalaivani, R.; Maruthupandy, M.; Muneeswaran, T.; Hameedha Beevi, A.; Anand, M.; Ramakritinan, C.M.; Kumaraguru, A.K. Synthesis of chitosan mediated silver nanoparticles (Ag NPs) for potential antimicrobial applications. Front. Lab. Med. 2018, 2, 30–35.
- Vargas-Reus, M.A.; Memarzadeh, K.; Huang, J.; Ren, G.G.; Allaker, R.P. Antimicrobial activity of nanoparticulate metal oxides against peri-implantitis pathogens. Int. J. Antimicrob. Agents 2012, 40, 135–139.
- Liu, W.; Su, P.; Chen, S.; Wang, N.; Ma, Y.; Liu, Y.; Wang, J.; Zhang, Z.; Li, H.; Webster, T.J. Synthesis of TiO2 nanotubes with ZnO nanoparticles to achieve antibacterial properties and stem cell compatibility. Nanoscale 2014, 6, 9050–9062.
- Sodagar, A.; Akhoundi, M.S.A.; Bahador, A.; Jalali, Y.F.; Behzadi, Z.; Elhaminejad, F.; Mirhashemi, A.H. Effect of TiO2 nanoparticles incorporation on antibacterial properties and shear bond strength of dental composite used in orthodontics. Dental Press J. Orthod. 2017, 22, 67–74.
- Zhang, M.; Liu, X.; Xie, Y.; Zhang, Q.; Zhang, W.; Jiang, X.; Lin, J. Biological Safe Gold Nanoparticle-Modified Dental Aligner Prevents the Porphyromonas gingivalis Biofilm Formation. ACS Omega 2020, 5, 18685–18692.
- Roveri, N.; Battistella, E.; Foltran, I.; Foresti, E.; Iafisco, M.; Lelli, M.; Palazzo, B.; Rimondini, L. Synthetic biomimetic carbonate-hydroxyapatite nanocrystals for enamel remineralization. In Proceedings of the Advanced Materials Research; Trans Tech Publications: Cham, Switzerland, 2008; Volume 47–50, Part 2. pp. 821–824.
- Chen, C.; Weir, M.D.; Cheng, L.; Lin, N.J.; Lin-Gibson, S.; Chow, L.C.; Zhou, X.; Xu, H.H.K. Antibacterial activity and ion release of bonding agent containing amorphous calcium phosphate nanoparticles. Dent. Mater. 2014, 30, 891–901.
- Ladd, M.R.; Lee, S.J.; Stitzel, J.D.; Atala, A.; Yoo, J.J. Co-electrospun dual scaffolding system with potential for muscle-tendon junction tissue engineering. Biomaterials 2011, 32, 1549–1559.
- Huang, Z.; Sargeant, T.D.; Hulvat, J.F.; Mata, A.; Bringas, P.; Koh, C.Y.; Stupp, S.I.; Snead, M.L. Bioactive nanofibers instruct cells to proliferate and differentiate during enamel regeneration. J. Bone Miner. Res. 2008, 23, 1995–2006.
- Batra, P. Nanoparticles and their Applications in Orthodontics. Adv. Dent. Oral Health 2016, 2.
- Borzabadi-Farahani, A.; Borzabadi, E.; Lynch, E. Nanoparticles in orthodontics, a review of antimicrobial and anti-caries applications. Acta Odontol. Scand. 2014, 72, 413–417.
- Eliades, T.; Zinelis, S.; Bourauel, C.; Eliades, G. Manufacturing of Orthodontic Brackets: A Review of Metallurgical Perspectives and Applications. Recent Patents Mater. Sci. 2010, 1, 135–139.
- Ogiński, T.; Kawala, B.; Mikulewicz, M.; Antoszewska-Smith, J. A Clinical Comparison of Failure Rates of Metallic and Ceramic Brackets: A Twelve-Month Study. BioMed Res. Int. 2020, 2020.
- Bapat, R.A.; Chaubal, T.V.; Joshi, C.P.; Bapat, P.R.; Choudhury, H.; Pandey, M.; Gorain, B.; Kesharwani, P. An overview of application of silver nanoparticles for biomaterials in dentistry. Mater. Sci. Eng. C 2018, 91, 881–898.
- Hernández-Gómora, A.E.; Lara-Carrillo, E.; Robles-Navarro, J.B.; Scougall-Vilchis, R.J.; Hernández-López, S.; Medina-Solís, C.E.; Morales-Luckie, R.A. Biosynthesis of silver nanoparticles on orthodontic elastomeric modules: Evaluation of mechanical and antibacterial properties. Molecules 2017, 22, 1407.
- Mhaske, A.R.; Shetty, P.C.; Bhat, N.S.; Ramachandra, C.S.; Laxmikanth, S.M.; Nagarahalli, K.; Tekale, P.D. Antiadherent and antibacterial properties of stainless steel and NiTi orthodontic wires coated with silver against Lactobacillus acidophilus—an in vitro study. Prog. Orthod. 2015, 16.
- Espinosa-Cristóbal, L.F.; López-Ruiz, N.; Cabada-Tarín, D.; Reyes-López, S.Y.; Zaragoza-Contreras, A.; Constandse-Cortéz, D.; Donohué-Cornejo, A.; Tovar-Carrillo, K.; Cuevas-González, J.C.; Kobayashi, T. Antiadherence and antimicrobial properties of silver nanoparticles against streptococcus mutans on brackets and wires used for orthodontic treatments. J. Nanomater. 2018, 2018.
- Besinis, A.; Hadi, S.D.; Le, H.R.; Tredwin, C.; Handy, R.D. Antibacterial activity and biofilm inhibition by surface modified titanium alloy medical implants following application of silver, titanium dioxide and hydroxyapatite nanocoatings. Nanotoxicology 2017, 11, 327–338.
- Besinis, A.; De Peralta, T.; Handy, R.D. Inhibition of biofilm formation and antibacterial properties of a silver nano-coating on human dentine. Nanotoxicology 2014, 8, 745–754.
- Tuan, T.Q.; Van Son, N.; Dung, H.T.K.; Luong, N.H.; Thuy, B.T.; Van Anh, N.T.; Hoa, N.D.; Hai, N.H. Preparation and properties of silver nanoparticles loaded in activated carbon for biological and environmental applications. J. Hazard. Mater. 2011, 192, 1321–1329.
- Vanitha, G.; Rajavel, K.; Boopathy, G.; Veeravazhuthi, V.; Neelamegam, P. Physiochemical charge stabilization of silver nanoparticles and its antibacterial applications. Chem. Phys. Lett. 2017, 669, 71–79.
- Bürgers, R.; Eidt, A.; Frankenberger, R.; Rosentritt, M.; Schweikl, H.; Handel, G.; Hahnel, S. The anti-adherence activity and bactericidal effect of microparticulate silver additives in composite resin materials. Arch. Oral Biol. 2009, 54, 595–601.
- Espinosa-Cristóbal, L.F.; Martinez-Castanon, G.A.; Téllez-Déctor, E.J.; Niño-Martínez, N.; Zavala-Alonso, N.V.; Loyola-Rodríguez, J.P. Adherence inhibition of Streptococcus mutans on dental enamel surface using silver nanoparticles. Mater. Sci. Eng. C 2013, 33, 2197–2202.
- PRIME PubMed | Nanosilver Coated Orthodontic Brackets: In Vivo Antibacterial Properties and Ion Release. Available online: (accessed on 13 July 2020).
- Kim, J.-S.; Shin, D.-H. Inhibitory effect on Streptococcus mutans and mechanical properties of the chitosan containing composite resin. Restor. Dent. Endod. 2013, 38, 36.
- Inhibitory Effect of Water-Soluble Chitosan on Growth of Streptococcus Mutans—PubMed. Available online: (accessed on 14 July 2020).
- Ikinci, G.; Şenel, S.; Akincibay, H.; Kaş, S.; Erciş, S.; Wilson, C.G.; Hincal, A.A. Effect of chitosan on a periodontal pathogen Porphyromonas gingivalis. Int. J. Pharm. 2002, 235, 121–127.
- Yassaei, S.; Nasr, A.; Zandi, H.; Motallaei, M.N. Comparison of antibacterial effects of orthodontic composites containing different nanoparticles on Streptococcus mutans at different times. Dental Press J. Orthod. 2020, 25, 52–60.
- Eshed, M.; Lellouche, J.; Matalon, S.; Gedanken, A.; Banin, E. Sonochemical coatings of ZnO and CuO nanoparticles inhibit streptococcus mutans biofilm formation on teeth model. Langmuir 2012, 28, 12288–12295.
- The Effect of CuO Nanoparticles on Antimicrobial Effects and Shear Bond Strength of Orthodontic Adhesives—PubMed. Available online: (accessed on 16 July 2020).
- Poosti, M.; Ramazanzadeh, B.; Zebarjad, M.; Javadzadeh, P.; Naderinasab, M.; Shakeri, M.T. Shear bond strength and antibacterial effects of orthodontic composite containing TiO2 nanoparticles. Eur. J. Orthod. 2013, 35, 676–679.
- Salehi, P.; Babanouri, N.; Roein-Peikar, M.; Zare, F. Long-term antimicrobial assessment of orthodontic brackets coated with nitrogen-doped titanium dioxide against Streptococcus mutans. Prog. Orthod. 2018, 19, 35.
- Ahn, S.J.; Lee, S.J.; Kook, J.K.; Lim, B.S. Experimental antimicrobial orthodontic adhesives using nanofillers and silver nanoparticles. Dent. Mater. 2009, 25, 206–213.
- Cao, B.; Wang, Y.; Li, N.; Liu, B.; Zhang, Y. Preparation of an orthodontic bracket coated with an nitrogen-doped TiO2-xNy thin film and examination of its antimicrobial performance. Dent. Mater. J. 2013, 32, 311–316.
- Kachoei, M.; Eskandarinejad, F.; Divband, B.; Khatamian, M. The effect of zinc oxide nanoparticles deposition for friction reduction on orthodontic wires. Dent. Res. J. (Isfahan) 2013, 10, 499–505.
- Behroozian, A.; Kachoei, M.; Khatamian, M.; Divband, B. The effect of ZnO nanoparticle coating on the frictionalresistance between orthodontic wires and ceramic brackets. J. Dent. Res. Dent. Clin. Dent. Prospects 2016, 10, 106–111.
- Goto, M.; Kasahara, A.; Tosa, M. Low-friction coatings of zinc oxide synthesized by optimization of crystal preferred orientation. Tribol. Lett. 2011, 43, 155–162.
- Rossouw, P.E. Friction: An overview. Semin. Orthod. 2003, 9, 218–222.
