Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 4 by Karina Chen and Version 3 by Karina Chen.
The use of silver preparations in medicine is becoming increasingly popular.
- silver (I) complex
- ophthalmic diseases
- eye drops
- eye ointment
- Ocular Rosacea
- drops stabilization
1. Silver in Ophthalmology
1.1. History of Silver as an Antibacterial Agent
The first mention of the use of silver in medicine comes from ancient times. Hippocrates probably already used silver preparations for the treatment of ulcers and to promote wound healing. Soluble silver (I) compounds, such as silver (I) nitrate, were first used empirically as a blood-purifying agent and date back to 702–705 AD [1]. Later, silver (I) salts were used as an antimicrobial agent to treat infectious diseases, including syphilis and gonorrhea, brain infections, epilepsy, mental illness, nicotine addiction and gastroenteritis [2].
The widest use of silver in medicine took place in the 1880s. In these years, the first silver plate was implanted during cranioplasty, and the use of eye drops with silver (I) nitrate solution was started to prevent childhood blindness and reduce gonococcal ophthalmia neonatorum [3]. Mandatory ophthalmic prophylaxis in newborns with drops of silver (I) nitrate, as in Credé’s method, was accepted in many countries throughout the world until the 1970s, and in some areas it still remains a routine part of perinatal care today [4][5]. Over the years, the use of silver (I) preparations in ophthalmology has been significantly extended to treat corneal ulcers, interstitial keratitis, blepharitis and dacryocystitis [6].
1.2. Toxicology
The toxicology of silver is not well documented, and much of the available information concerning the release of Ag (I) from medical devices and other products intended for human use has been ambiguous. The few publications with experimental results in animal models have also been inconsistent. However, although they are insufficient in predicting human risk from silver exposure, they do provide relevant information on cytotoxicity, intracellular management of Ag (I) and excretion routes [7].
Studies of silver metabolism indicate that soluble silver (I) compounds are more easily absorbed as a result of their ability to bind to proteins, DNA and RNA. Soluble silver (I) compounds can be quickly absorbed into the bloodstream, deposited throughout the body and then reduced by light to metallic silver [8]. Acute symptoms of overexposure to silver (I) nitrate are decreased blood pressure, diarrhea, stomach irritation and decreased respiration. Chronic symptoms from prolonged intake of low doses of silver (I) salts are fatty degeneration of the liver and kidneys and changes in blood cells [9]. Soluble silver (I) compounds are also capable of accumulating in small amounts in the brain and in muscles [10].
The literature reports that long-term inhalation or ingestion of soluble silver (I) compounds or colloidal silver may cause necrosis of conjunctival epithelial cells, argyria and/or argyrosis [10][11][12]. Moreover, irritation, conjunctival scars, corneal opacity and symblepharon have been noted [13]. In clinical practice, the diagnosis of eye argyrosis may not be easy due to the rarity of this disease. Differential diagnosis should include other keratopathies (e.g., pre-Descemet dystrophy and X-linked ichthyosis) as well as other causes of abnormal eye pigmentation, such as malignant melanomas, deposition of heavy metals (iron and copper) or drugs (ciprofloxacin and amiodarone) [14][15].
The recent results of experimental studies did not show significant toxic effects of Ag-NPs and AgNO3 in doses up to 1 mg kg-1 of rat body weight. The distribution of Ag in organs was similar in both studied groups of treated rats. The total Ag content in organs was significantly lower in rats treated with Ag-NPs, but in this group, it was found to be more toxic in terms of biochemical and hematological parameters than in rats treated with AgNO3 [16]. Ag-NPs probably caused reactive oxygen species and oxidative damage, which would confirm oxidative stress as an additional possible mechanism of Ag-NPs’ toxicity [16]. Other studies have shown lower toxicity of Ag-NPs compared to AgNO3, which was attributed to the coatings that stabilize nanoparticles and thus reduce their toxicity [17].
2. Application of Silver Compounds in Ophthalmology
Nowadays, silver metal and silver nanoparticles are used as gels or films for medical device coatings and the reduction of bacterial adhesion to the surfaces of implants [18]. In ophthalmology, the use of nano-silver (nAg) for covering corneal prosthetic devices (KPros) has been sought to prevent Pseudomonas aeruginosa and Staphylococcus aureus biofilm formation as a protection against perioperative and early postoperative infections [19]. Intrastromal administration of highly biocompatible gelatin-capped silver nanoparticles (G-Ag NPs) has been a promising, dual-functional (antimicrobial and antiangiogenic) nanotherapy for the treatment of Staphylococcus aureus-induced bacterial keratitis in rabbits [20].
New applications of silver in ocular disease diagnosis and treatment are still being sought. The high usefulness of silver-amplified immunochromatography for detection of adenoviral conjunctivitis has been demonstrated [21].
It has also been reported that Ag-NPs are a potential alternative, and may even be better than mitomycin C, as an adjunctive therapy in glaucoma surgery to reduce fibroblast proliferation and bleb fibrosis after trabeculectomy [22].
The strong therapeutic effect of biologically synthesized silver nanoparticles against vascular endothelial growth factor (VEGF) has been proven. Ag-NPs, as inhibitors of tyrosine kinase Src and AKT/PI3K pathways, are able to inhibit further routes of angiogenesis from proliferative diabetic retinopathy and age-related macular degeneration in rodent eye models and, therefore, appear to be a promising treatment for many retinal diseases in humans [23][24][25].
The incorporation of Ag-NPs into silicone-hydrogel contact lenses allows for significant inhibition of bacterial growth and reduction of biofilm formation, with additional reinforcement of some of the mechanical properties [26].
3. Silver (I) Complex with Metronidazole in Ophthalmology
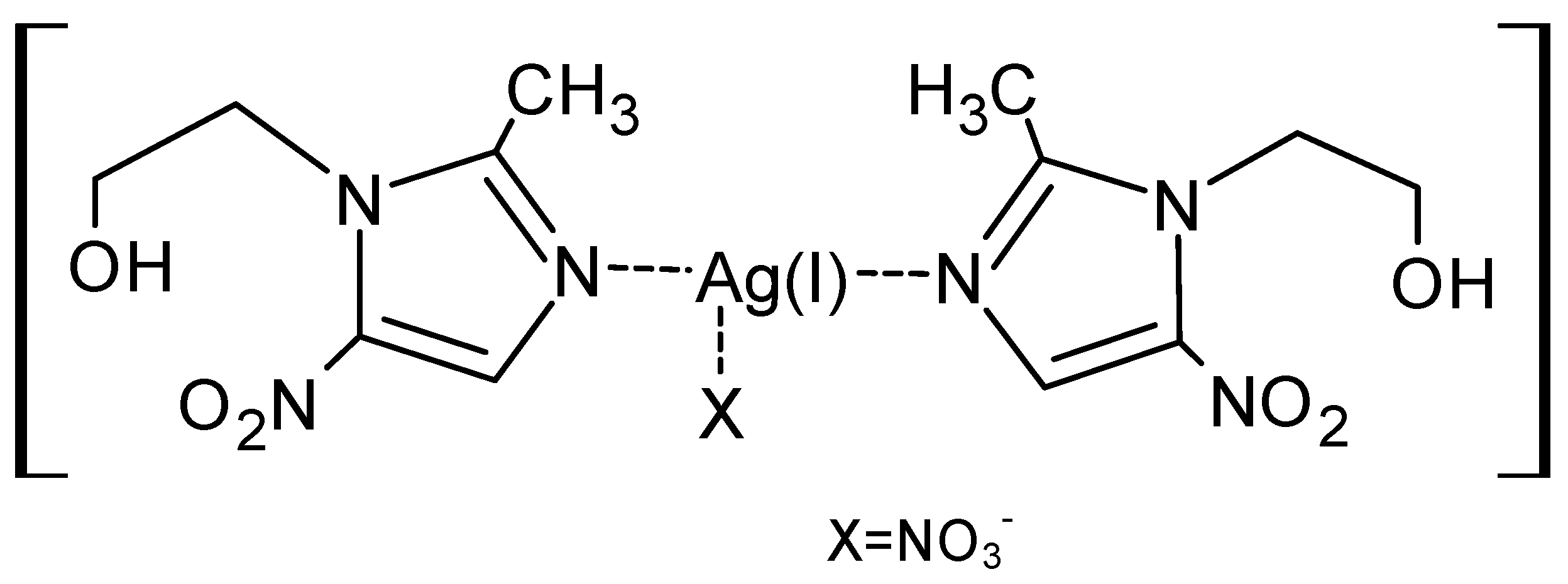
Research on the use of new silver preparations combined with other active substances in ophthalmology is developing much more vigorously [78][27]. Numerous studies showed greater stability of metal ion complexes compared to metal ion salts [27] [28]and lower toxicity due to the possibility of using lower concentrations of silver ions in complexes [78][27].The widest and best-known use of silver in medicine has been in combination with sulfadiazine (AgSD), where it becomes a topical antibacterial agent for the treatment of burns [79][29] and fungal keratitis [80,81][30][31]. The action of AgSD also demonstrates strong antibacterial potential against E. coli, Staph. aureus, Klebsiella sp. and Pseudomonas sp. [16][32].In terms of biological performance, studies in vitro, as well as in vivo, on retinal pigment epithelium with endophthalmitis in mouse and rabbit models confirm the cellular biocompatibility and antibacterial function of silver complex nanomaterials. The addition of photodynamic therapy with Ag-NPs as well as AuAgCu2O-bromfenac sodium nanoparticles allows the antibacterial effect to be strengthened against Escherichia coli, Staphylococcus aureus and methicillin-resistant S. aureus for synergistic treatment of post-cataract surgery endophthalmitis [82,83][33][34].Ag-NPs conjugated with oleic acid or vildagliptin exhibit antiacanthamoebic activity that can be therapeutically applied against Acanthamoeba castellanii, an opportunistic pathogen that is associated with blinding eye keratitis and a rare but fatal central nervous system infection [84,85][35][36].In our previous paper, we described, for the first time in the literature, the action of a metronidazole complex with well-soluble silver (I) salts in the form of drops and ointment in the treatment of ocular rosacea [86][37]. The use of a well-soluble silver (I) complex with metronidazole (Figure 1) reduced the side effects of silver (I) nitrate used alone and the costs and complications of standard antibiotic therapy. The use of two clinically proven drugs and combining them into a complex compound does not only result in additive synergy. As we have shown in our previous work, the action of the complex compound overcomes bacterial resistance [2738].Figure 1. Silver (I) nitrate complex with metronidazole [Ag(MTZ)2]NO3.
The antimicrobial effectiveness of silver preparations in ophthalmic diseases has been documented by many researchers. Complex silver (I) compounds seem to be a promising alternative to standard therapy and are, therefore, also considered as new generation antibiotics. Most silver (I) preparations are clinically used for topical applications. Few experimental results indicate the usefulness of intraocular or systemic administration of silver (I) preparations as an alternative or additional therapy in infectious and angiogenic eye diseases. New forms of silver (I) products will certainly find application in the treatment of many ophthalmic diseases. One of the most important features of the silver (I) complex is its capacity to break down bacterial resistance. It is very helpful to maintain the appropriate characteristics of the dosage form, e.g., pH and chemical, physical and pharmaceutical stabilities.
References
- Hill, W.R.; Pillsbury, D.M. Argyria—The Pharmacology of Silver; Williams & Wilkins: Baltimore, MD, USA, 1939.
- Alexander, J.W. History of the medical use of silver. Surg. Infect. 2009, 10, 289–292.
- Rollings, N.B. Georgia Arbuckle Fix: Silver dollar surgeon. Am. Hist. Illus. 1985, 20, 20–21.
- Moore, D.L.; MacDonald, N.E. Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Preventing ophthalmia neonatorum. Paediatr. Child Health 2015, 20, 93–96.
- Silva, L.R.; Gurgel, R.Q.; Lima, D.R.; Cuevas, L.E. Current usefulness of Credé’s method of preventing neonatal ophthalmia. Ann. Trop. Paediatr. 2008, 28, 45–48.
- Roe, A.L. Collosol argentum and its ophthalmic uses. Br. Med. J. 1915, 16, 104.
- Lansdown, A.B. A pharmacological and toxicological profile of silver as an antimicrobial agent in medical devices. Adv. Pharmacol. Sci. 2010, 2010, 910686.
- Jongerius, O.; Jongeneelen, F.I. Occupational Exposure Limits (Criteria Document for Metallic Silver); Commission of the European Communities: Brussels, Belgium, 1992.
- Venugopal, B.; Lucky, T.D. Metal. Toxicity in Mammals; Plenum Press: New York, NY, USA, 1978; Volume 2, pp. 86–99.
- Fung, M.C.; Bowen, D.L. Silver products for medical indications: Risk-benefit assessment. J. Toxicol. Clin. Toxicol. 1996, 34, 119–126.
- Zheng, J.; Zhang, K.; Liu, Y.; Wang, Y. Fatal acute arsenic poisoning by external use of realgar: Case report and 30 years literature retrospective study in China. Forensic Sci. Int. 2019, 300, e24–e30.
- Gulbranson, S.H.; Hud, J.A.; Hansen, R.C. Argyria following the use of dietary supplements containing colloidal silver protein. Cutis 2000, 66, 373–374.
- Claessens, D.; Zeitz, P.F.; Beckers, H. Blaugraue Verfärbung von Haut und Bindehaut [Bluish-gray discoloration of skin and conjunctiva]. Ophthalmologe 2020, 117, 66–68.
- Sarnat-Kucharczyk, M.; Pojda-Wilczek, D.; Mrukwa-Kominek, E. Diagnostic methods in ocular argyrosis: Case report. Doc. Ophthalmol. 2016, 133, 129–138.
- Pala, G.; Fronterré, A.; Scafa, F.; Scelsi, M.; Ceccuzzi, R.; Gentile, E.; Candura, S.M. Ocular argyrosis in a silver craftsman. J. Occup. Health 2008, 50, 521–524.
- Qin, G.; Tang, S.; Li, S.; Lu, H.; Wang, Y.; Zhao, P.; Li, B.; Zhang, J.; Peng, L. Toxicological evaluation of silver nanoparticles and silver nitrate in rats following 28 days of repeated oral exposure. Environ. Toxicol. 2017, 32, 609–618.
- Cvjetko, P.; Milošić, A.; Domijan, A.M.; Vinković Vrček, I.; Tolić, S.; Peharec Štefanić, P.; Letofsky-Papst, I.; Tkalec, M.; Balen, B. Toxicity of silver ions and differently coated silver nanoparticles in Allium cepa roots. Ecotoxicol. Environ. Saf. 2017, 137, 18–28.
- Leitão, J.H.; Sousa, S.A.; Leite, S.A.; Carvalho, M.F.N.N. Silver Camphor Imine Complexes: Novel Antibacterial Compounds from Old Medicines. Antibiotics 2018, 7, 65.
- Riau, A.K.; Aung, T.T.; Setiawan, M.; Yang, L.; Yam, G.H.F.; Beuerman, R.W.; Venkatraman, S.S.; Mehta, J.S. Surface Immobilization of Nano-Silver on Polymeric Medical Devices to Prevent Bacterial Biofilm Formation. Pathogens 2019, 8, 93.
- Luo, L.J.; Lin, T.Y.; Yao, C.H.; Kuo, P.Y.; Matsusaki, M.; Harroun, S.G.; Huang, C.C.; Lai, J.Y. Dual-functional gelatin-capped silver nanoparticles for antibacterial and antiangiogenic treatment of bacterial keratitis. J. Colloid Interface Sci. 2019, 536, 112–126.
- Fujimoto, T.; Hanaoka, N.; Konagaya, M.; Kobayashi, M.; Nakagawa, H.; Hatano, H.; Tsukahara-Kawamura, T.; Uchio, E.; Kaneko, H. Evaluation of a silver-amplified immunochromatography kit for adenoviral conjunctivitis. J. Med. Virol. 2019, 91, 1030–1035.
- Butler, M.R.; Prospero Ponce, C.M.; Weinstock, Y.E.; Orengo-Nania, S.; Chevez-Barrios, P.; Frankfort, B.J. Topical silver nanoparticles result in improved bleb function by increasing filtration and reducing fibrosis in a rabbit model of filtration surgery. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4982–4990.
- Kalishwaralal, K.; BarathManiKanth, S.; Pandian, S.R.K.; Deepak, V.; Gurunathan, S. Silver nano—A trove for retinal therapies. J. Control. Release 2010, 145, 76–90.
- Pershadsingh, H.A.; Moore, D.M. PPARγ agonists: Potential as therapeutics for neovascular retinopathies. PPAR Res. 2008, 164273.
- Gurunathan, S.; Lee, K.J.; Kalishwaralal, K.; Sheikpranbabu, S.; Vaidyanathan, R.; Eom, S.H. Antiangiogenic properties of silver nanoparticles. Biomaterials 2009, 30, 6341–6350.
- Mourad, R.; Helaly, F.; Darwesh, O.; Sawy, S.E. Antimicrobial and physicomechanical natures of silver nanoparticles incorporated into silicone-hydrogel films. Cont. Lens Anterior Eye 2019, 42, 325–333.
- Kalinowska-Lis, U.; Felczak, A.; Chęcińska, L.; Zawadzka, K.; Patyna, E.; Lisowska, K.; Ochocki, J. Synthesis, characterization and antimicrobial activity of water-soluble silver(i) complexes of metronidazole drug and selected counter-ions. Dalton Trans. 2015, 44, 8178–8189.Radko, L.; Stypuła-Trębas, S.; Posyniak, A.; Żyro, D.; Ochocki, J. Silver (I) Complexes of the Pharmaceutical Agents Metronidazole and 4-Hydroxymethylpyridine: Comparison of Cytotoxic Profile for Potential Clinical Application. Molecules 2019, 24, 1949.
- Żyro, D.; Śliwińska, A.; Szymczak-Pajor, I.; Stręk, M.; Ochocki, J. Light Stability, Pro-Apoptotic and Genotoxic Properties of Silver (I) Complexes of Metronidazole and 4-Hydroxymethylpyridine against Pancreatic Cancer Cells In Vitro. Cancers 2020, 12, 3848.
- Modak, S.M.; Sampath, L.; Fox, C.L.J. Combined topical use of silver sulfadiazine and antibiotics as a possible solution to bacterial resistance in burn wounds. J. Burn Care Rehabil. 1988, 9, 359–363.
- FlorCruz, N.V.; Evans, J.R. Medical interventions for fungal keratitis. Cochrane Database Syst. Rev. 2015, 9, CD004241.
- Mohan, M.; Gupta, S.K.; Kalra, V.K.; Vajpayee, R.B.; Sachdev, M.S. Topical silver sulphadiazine—A new drug for ocular keratomycosis. Br. J. Ophthalmol. 1988, 72, 192–195.
- Rai, M.K.; Deshmukh, S.D.; Ingle, A.P.; Gade, A.K. Silver nanoparticles: The powerful nanoweapon against multidrug-resistant bacteria. J. Appl. Microbiol. 2012, 112, 841–852.
- Chen, H.; Yang, J.; Sun, L.; Zhang, H.; Guo, Y.; Qu, J.; Jiang, W.; Chen, W.; Ji, J.; Yang, Y.W.; et al. Synergistic Chemotherapy and Photodynamic Therapy of Endophthalmitis Mediated by Zeolitic Imidazolate Framework-Based Drug Delivery Systems. Small 2019, 15, e1903880.
- Ye, Y.; He, J.; Qiao, Y.; Qi, Y.; Zhang, H.; Santos, H.A.; Zhong, D.; Li, W.; Hua, S.; Wang, W.; et al. Mild temperature photothermal assisted anti-bacterial and anti-inflammatory nanosystem for synergistic treatment of post-cataract surgery endophthalmitis. Theranostics 2020, 10, 8541–8557.
- Anwar, A.; Abdalla, S.A.O.; Aslam, Z.; Shah, M.R.; Siddiqui, R.; Khan, N.A. Oleic acid-conjugated silver nanoparticles as efficient antiamoebic agent against Acanthamoeba castellanii. Parasitol. Res. 2019, 118, 2295–2304.
- Anwar, A.; Siddiqui, R.; Raza Shah, M.; Khan, N.A. Antidiabetic Drugs and Their Nanoconjugates Repurposed as Novel Antimicrobial Agents against Acanthamoeba castellanii. J. Microbiol. Biotechnol. 2019, 29, 713–720.
- Waszczykowska, A.; Żyro, D.; Jurowski, P.; Ochocki, J. Effect of treatment with silver (I) complex of metronidazole on ocular rosacea: Design and formulation of new silver drug with potent antimicrobial activity. J. Trace Elem. Med. Biol. 2020, 61, 126531.
- Kalinowska-Lis, U.; Felczak, A.; Chęcińska, L.; Zawadzka, K.; Patyna, E.; Lisowska, K.; Ochocki, J. Synthesis, characterization and antimicrobial activity of water-soluble silver(i) complexes of metronidazole drug and selected counter-ions. Dalton Trans. 2015, 44, 8178–8189.
More