Information and Communication Technology (ICT) solutions facilitate the monitoring and management of older people’s health to improve quality of life and physical activity with a decline in caregivers’ burden.
- ICT Healthcare Solutions
1. Introduction
In the field of healthcare advancement, ICT solutions may potentially play an important role in enhancing the quality of life of the aging population and allow their independent living. Integrated ICT solutions assist in the healthy and safe aging of older people and minimise health and social expenses. They are greatly sustained in developed countries aiming to improve the quality of life (QoL), ensure the sustainability of care of its aging population, and pursue the demographic crisis through applying ICT solutions for home care in the context of old age-related chronic diseases [1].
2. Different Categories of ICT Solutions
The range of ICT technologies varies between quite simple and very sophisticated ICT solutions, all having the common objective of improving the QoL of older people. Such ICT solutions can range from smart home systems and telehealth applications to reminder functions, fall detection/prediction/prevention systems, smartphones, etc. [2]. Figure 15 gives the different categories of ICT solutions.
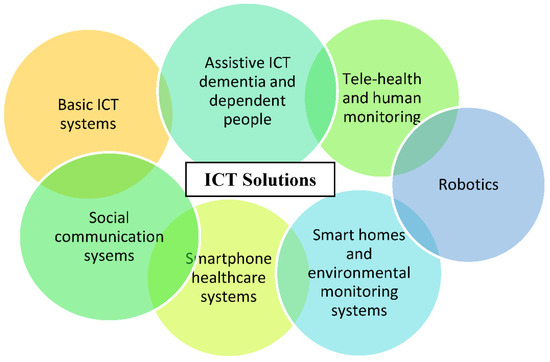
Older people already use a wide range of ICT solutions in their daily lives. Such ICT solutions that are home-based, as televisions and microwave ovens, as well as computer-based technologies as internet and emails are considered Basic ICT Technologies. Basic ICT solutions have a positive impact on the QoL of older people living in their homes [3]. For example, internet-based technologies allow changes in older people’s health behaviour using different interventions as self-help programs and customised health-related data presentation through matching personal data to reachable interventions.
Social Communication Systems as mobile phones allow older people to stay in touch with their family members, caregivers, and clinicians or care providers. Social communication systems benefit older people living in their own environment by permitting social interaction using ICT solutions as video calling, thus decreasing isolation and depression levels in the older population as well as affecting older people’s health and level of life satisfaction positively [4]. Despite the advantage of allowing remote social communication, it is feared that ICTs could elevate the feeling of loneliness of older people living in their own environment [5]. Video conferencing ICT systems are also considered social communication systems. An example of such a system is those supporting older people with chronic diseases. These systems provide access to older people’s support around the clock and deliver a user-centred social care system interconnected to tele-medicine processes [6].
Smartphone Healthcare Systems give older people the opportunity to access their own health data and collaborate in their own healthcare process through accepting services that improve their health behaviour. These systems provide older people with lifestyle guidance, fitness exercises, chronic disease management, as well as providing public health surveillance [7].
Smart Home Solutions and Environmental Monitoring Systems provide older people with a collection of procedures based on various devices and sensors displayed in their living environment. Such ICT solutions enable monitoring and management of older people’s health using telehealth applications with the aim of improving their QoL and supporting their physical independence. Examples of smart home solutions and environmental monitoring systems can be fall detection systems, daily activity monitoring systems, and medical condition monitoring with vital data analysis. Such solutions address clinical syndromes through providing assurance and emergency assistance to the user and thus reducing caregivers’ burden [8]. These systems allow the older user to be more involved in decision-making rather than being only the recipient of clinical decisions taken by clinicians [9].
Robotics is expected to play a major role in the healthcare of older people in the future [10]. Robots vary in the role they perform in helping the user to live actively and independently in their own environment. Robots fluctuate between service robots that support older people to perform daily activities and robots that act as social companions. Robotics is mainly applied in systems addressing mental health conditions since it has an impact on emotional, physiological, and social health [11].
Telehealth and Human Monitoring are addressed mainly to home hospice people and their caregivers. They provide different monitoring services such as functional services as sleep quality monitoring, safety services as detecting environmental hazards, physiological services as monitoring vital health parameters, and security services as alert alarms. Such monitoring technologies aim to increase the independence of the user through allowing real-time intervention just in time and provide him/her with acceptable support. Telehealth and human monitoring solutions enable the empowerment of the older user, the caregivers, and family members by permitting their involvement in the daily care process [12].
Assistive ICT for Dementia and Dependent People provides older people with chronic diseases as dementia with more independence, safety, social communication, and an enhancement in activity performance. Thus, such solutions improve the QoL of older people living in their own environment. Older people using these systems are provided support in different areas of delivery of information. The provided support can be concerning their dementia symptoms, social interaction, health monitoring, and general safety. This type of ICT solution can increase its users’ self-confidence and reduce levels of social isolation. These systems are proven to increase the feeling of safeness and reduce the feeling of fear and anxiety in older people with dementia [13].
3. Development of ICT Solutions
The main four themes that emerged throughout the development process of ICT solutions are: technology acceptance and readiness, novel patient monitoring and smart home technologies, intelligent algorithm and software engineering, and robotics technologies [14], as presented in Figure 2.
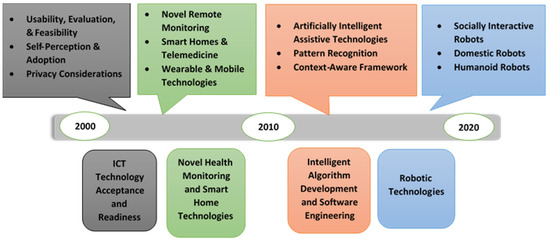
ICT Technology Acceptance and Readiness involves studies that took place in the early 2000s and is considered to be the first era of technology research for the aging society. In this phase, researchers examined older people’s acceptance of monitoring technologies using non-wearable sensors such as electronic health systems and smart home-based technologies using bed, motion, kitchen safety, and fall detection [15][16]. In addition to older people’s acceptability, other studies investigated the usefulness, feasibility, and privacy of assistive tele-monitoring systems [17][18].
Novel Health Monitoring and Smart Home Technology are more sophisticated ICT systems that emerged after the year 2000. This type of system uses both wearable and non-wearable sensors. Such systems rely on interaction between sensors, mobile devices, cloud servers, and supervised machine learning approaches, novel protocols over SMS to allow communication between the older user and caregivers [2][3]. It was recognised that the blending of telemonitoring intervention with smart home technologies enhanced older people’s skills in problem solving and self-efficiency in managing their medical conditions [4].
Intelligent Algorithm Development and Software Engineering became of great interest for research after 2010. This period is the second era of technology research for the aging society. In this phase, researchers explored the development of prototype systems, the establishment of new sensor-based smart home technologies, assistive robots’ development, and the conceptualisation of new AI and machine learning solutions. This development in technology led researchers to the capability of developing new sophisticated AI algorithms and advanced context acquisition methods for advanced analysation and automation of complex tasks [19]. An example of different intelligent algorithms is those involved in collecting data about the user’s environment and can predict potential problems for better decision-making (data mining algorithms). Examples of software development include the usage of context-aware middleware that can sense and respond to the user’s environment, the employment of pyroelectric sensors and infrared optoelectronic components with the aim of detecting electromagnetic radiation, and analysing the collected data to monitor and manage user’s daily activity [5][6][7].
Robotics Technologies emerged around 2010. There are various robotic technologies that affect older people’s healthcare. They vary between advanced AI robotic technologies and simple assistive robotic activities [7][8]. Telepresence robots, companion robots, home automation and domestic assistive robots, rehabilitation and health monitoring robots, and reminder robots are examples of robotic systems that can be integrated with older people’s healthcare monitoring and management solutions. It is revealed that the development and multidisciplinary nature of robotic systems played an important role in providing better interaction with the aging population as well as contributing to therapeutic benefits [19].
Over the last decade, different ICT solutions concentrating on AI and machine learning or focusing on the development of context-aware and adaptive technology rapidly emerged. The systems concentrating on AI and machine learning and using sensors and smart home devices have the aim of investigating user perception, barriers, and novel system development. Other systems focusing on the development of a context-aware technology have the aim of being integrated into any environment, collecting information from different sensors and devices concerning temperature, geographic location, and user preference as well as delivering relevant data based on the older user’s unique set of variables. Sapci et al. [14] announced that the use of AI and sophisticated algorithms in the healthcare monitoring and management of older people can improve the accuracy and progress of the analytical techniques performed, thus making the monitoring and management process faster and more accurate.
4. Examples of ICT Solutions
ICT solutions can help older people to manage their chronic conditions on a day-to-day basis. The use of ICT solutions can handle age-related physical and cognitive impairments aiming to prolong the functional capacity of older people, delay their institutionalisation, and increase their autonomy and participation in society.
Employment of ICT solutions for the early detection of chronic conditions enables older people’s self-management of personal health records and use of a management tool that integrates different aspects of an older person’s healthcare, including medical, social, and emotional issues. Older people with chronic conditions living in their own environment can be provided with adequate medical care and guaranteed health services through the use of efficient ICT networks [20].
Such ICT solutions involve continuous remote monitoring of older people for the management of different health conditions as hypertension and blood pressure and improve the prediction of new health conditions, as well as older person’s obedience.
ICT solutions permitting older person-centred care for diabetes mellitus involve blood glucose monitoring by telemonitoring systems, internet applications, and mobile devices. Such ICT solutions includes smart algorithms to control blood glucose levels as decision-making processors.
ICT solutions allowing older person-centred care for chronic heart diseases provide the potential for health ambulatory monitoring and enable remote coordinated care by healthcare providers. The scope of advance monitoring includes electronic weight scales, blood pressure (BP) meters, thermometers, as well as accelerometers for activity-monitoring and sleep-monitoring devices.
ICT solutions enabling older person-centred care for chronic obstructive pulmonary disease (COPD) include video or telephone links with healthcare providers either in real time or using store-and-forward technologies, internet-based telecommunication systems with healthcare providers, wired and wireless telemonitoring of physical parameters such as spirometry, respiratory rate, blood pressure, or oxygen saturation, pulmonary rehabilitation solutions with home-based video conferencing-supervised exercises and counselling, and telemonitoring of older people on home mechanical ventilation (HMV).
ICT solutions permitting older person-centred care for stroke mainly address physical care, consultation, and education. Such solutions provide monitoring services through integrating measurement devices, innovative interaction paradigms, customised motorial/cognitive neuro-rehabilitation treatments, continuous health status monitoring, cloud, and interoperable information systems.
ICT solutions allowing older person-centred care for cognitive impairment can support autonomous outdoor mobility, empowering participation in social events of older people with mild dementia. Such functionality is supported by assistive technology devices (ATDs), typically in the form of wearable devices which contain hardware and software that create a location-based service using global positioning system (GPS), cellular, and other signals.
Fall prevention intervention ICT solutions include fall detection and prevention ICT services to help older people live independently in their own environment by providing assistive support to clinical decisions. These ICT solutions concentrate on reducing fall risks and help older people to overcome them. Hamm et al. [21] parcelled fall prevention ICT solutions into four categories.
Pre-fall prevention intervention ICT solutions are ICT solutions targeting older people at risk of falling but who have not experienced any falling event yet. Such ICT solutions focus on the functional ability of the older user, supporting older people at risk of falling with services such as targeted physical activities and educational programs. These solutions have the aim of overcoming various intrinsic fall risk factors as balance, muscle strength and cognitive decline, and vision [22][23][24]. In this category of ICT solutions, gaming consoles as Wii and Xbox are deployed. For this reason, this category of fall prevention ICT solutions was excluded from the review.
Post-fall prevention intervention ICT solutions are ICT solutions focusing on older people who have previously experienced a fall by providing support to eliminate their risk of encountering future falls [14]. This category of fall prevention ICT solutions includes diagnostic assessment functions aiming to deliver re-active intervention to its users. These solutions include fall prediction solutions in this review.
Fall injury prevention intervention ICT solutions are ICT solutions that aim to enable assistive communication between older people and their care providers or clinicians. These systems include fall detection systems in this review. Fall injury prevention intervention ICT solutions target three main intervention types: activity monitoring, fall detection, and medical assistance. These solutions include fall detection solutions in this review.
Cross-fall prevention intervention ICT solutions are ICT solutions that support older people by delivering a blend of the previously mentioned fall interventions. This combination of different interventions has the aim of helping older people to manage their health conditions and to live independently in their own environment, using different ICT services that permit assistive collaboration between all older people, caregivers, and care providers. This category of ICT solutions includes fall prevention solutions in this review.
References
- Swartz, M.K. The PRISMA Statement: A Guideline for Systematic Reviews and Meta-Analyses. J. Pediatr. Health Care 2011, 25, 1–2.
- Siegel, C.; Dorner, T.E. Information technologies for active and assisted living—Influences to the quality of life of an ageing society. Int. J. Med. Inform. 2017, 100, 32–45.
- Matlabi, H.; Parker, S.; McKee, K.J. The contribution of home-based technology to older people’s quality of life in extra care housing. BMC Geriatr. 2011, 11, 68.
- Hensel, B.K.; Parkeroliver, D.; Demiris, G. Videophone Communication Between Residents and Family: A Case Study. J. Am. Med. Dir. Assoc. 2007, 8, 123–127.
- Sävenstedt, S.; Sandman, P.; Zingmark, K. The duality in using information and communication technology in elder care. J. Adv. Nurs. 2006, 56, 17–25.
- Levy, S.; Steele, G. End-of-Life and Living Technologies, The role of Telemedicine in palliative care of children and young people. In Proceedings of the 5th International ICST Conference on Pervasive Computing Technologies for Healthcare, Dublin, Ireland, 23–26 May 2011.
- Boulos, M.N.K.; Wheeler, S.; Tavares, C.; Jones, R.B. How smartphones are changing the face of mobile and participatory healthcare: An overview, with example from eCAALYX. Biomed. Eng. Online 2011, 10, 1–14.
- Frisardi, V.; Imbimbo, B.P. Gerontechnology for demented patients: Smart homes for smart aging. J. Alzheimer Dis. 2011, 23, 143–146.
- Demiris, G.; Thompson, H. Smart homes and ambient assisted living applications: From data to knowledge-empowering or overwhelming older adults? Contribution of the IMIA Smart Homes and Ambiant Assisted Living Working Group. Yearb. Med. Inform. 2011, 6, 51–57.
- Bemelmans, R.; Gelderblom, G.J.; Jonker, P.; De Witte, L. Socially Assistive Robots in Elderly Care: A Systematic Review into Effects and Effectiveness. J. Am. Med. Dir. Assoc. 2012, 13, 114–120.e1.
- Chang, S.-M.; Sung, H.-C. (Christina) The effectiveness of seal-like robot therapy on mood and social interactions of older adults: A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2013, 11, 68–75.
- Chou, C.-C.; Chang, C.-P.; Lee, T.-T.; Chou, H.-F.; Mills, M.E. Technology Acceptance and Quality of Life of the Elderly in a Telecare Program. CIN Comput. Inform. Nurs. 2013, 31, 335–342.
- Lauriks, S.; Reinersmann, A.; Van Der Roest, H.G.; Meiland, F.; Davies, R.J.; Moelaert, F.; Mulvenna, M.D.; Nugent, C.; Dröes, R.-M. Review of ICT-based services for identified unmet needs in people with dementia. Ageing Res. Rev. 2007, 6, 223–246.
- Sapci, A.H.; Sapci, H.A.; Yang, R.; Du, Y. Innovative Assisted Living Tools, Remote Monitoring Technologies, Artificial Intelligence-Driven Solutions, and Robotic Systems for Aging Societies: Systematic Review. JMIR Aging 2019, 2, e15429.
- Rougier, C.; Meunier, J.; St-Arnaud, A.; Rousseau, J. Robust Video Surveillance for Fall Detection Based on Human Shape Deformation. IEEE Trans. Circuits Syst. Video Technol. 2011, 21, 611–622.
- National Center for Chronic Disease Prevention and Health Promotion. The State of Aging & Health in America 2013; CDC: Atlanta, GA, USA, 2013.
- Koshmak, G.; Loutfi, A.; Linden, M. Challenges and Issues in Multisensor Fusion Approach for Fall Detection: Review Paper. J. Sens. 2016, 2016, 1–12.
- Sakr, G.E.; Elhajj, I.H.; Huijer, H.A.-S. Support Vector Machines to Define and Detect Agitation Transition. IEEE Trans. Affect. Comput. 2010, 1, 98–108.
- Rashidi, P.; Mihailidis, A. A Survey on Ambient-Assisted Living Tools for Older Adults. IEEE J. Biomed. Health Inform. 2013, 17, 579–590.
- Scalvini, S.; Baratti, D.; Assoni, G.; Zanardini, M.; Comini, L.; Bernocchi, P. Information and communication technology in chronic diseases: A patient’s opportunity. J. Med. Pers. 2013, 12, 91–95.
- Hamm, J.; Money, A.; Atwal, A.; Paraskevopoulos, I. Fall prevention intervention technologies: A conceptual framework and survey of the state of the art. J. Biomed. Inform. 2016, 59, 319–345.
- Montero-Odasso, M.; Verghese, J.; Beauchet, O.; Hausdorff, J.M. Gait and Cognition: A Complementary Approach to Understanding Brain Function and the Risk of Falling. J. Am. Geriatr. Soc. 2012, 60, 2127–2136.
- Ferreira, B.N.; Guimarães, V.; Ferreira, H.S. Smartphone based fall prevention exercises. In Proceedings of the 2013 IEEE 15th International Conference on e-Health Networking, Applications and Services (Healthcom 2013), Lisbon, Portugal, 9–12 October 2013; pp. 643–647.
- Ambrose, A.F.; Paul, G.; Hausdorff, J.M. Risk factors for falls among older adults: A review of the literature. Maturitas 2013, 75, 51–61.
