Several organic and inorganic nanoplatforms that have been designed exploiting the distinctive features of the tumor microenvironment and tumor cells offer favorable physicochemical properties and pharmacokinetic profiles of a parent drug, with delivery of higher amounts of the drug to the pathological site and its controlled release, thereby improving the balance between its efficacy and toxicity. Advances to this front have included the design and construction of targeted nanoparticles by conjugating homing devices like peptide, ligand, and Fab on the surface of nanomaterials to navigate nanoparticle drug complexes towards the target tumor cell with minimal destruction of healthy cells. Furthermore, actively targeting nanoparticles can facilitate the delivery and cellular uptake of nanoparticle-loaded drug constructs via binding with specific receptors expressed aberrantly on the surface of a tumor cell. Herein, we present an overview of the principle of targeted delivery approaches, exploiting drug-nanoparticle conjugates with multiple targeting moieties to target specific receptors of breast cancer cells and highlighting therapeutic evaluation in preclinical studies. We conclude that an understanding of the translational gap and challenges would show the possible future directions to foster the development of novel targeted nanotherapeutics.
- Nanoparticles Targeting Receptors
- Breast cancer
- cancer drug delivery
- preclinical studies
- active targeting
1. Introduction
Globally, breast cancer is the most recurring malignancy and a foremost cause of cancer-related deaths in women, with the second highest incidence rate (11.6%) among all other cancers [1]. According to the WHO cancer profile 2020, 269,792 breast cancer cases were diagnosed in the year 2018 and 2,778,850 newly diagnosed cases are expected in 2040 (WHO 2020). There is an increasing rate of 3.19% of new cases recorded each year from 1980 to 2010 worldwide despite remarkable advances in cancer diagnosis and treatment [2]. This growing pattern warranted more concern about breast cancer diagnosis and management by medical scientists and health lawmakers [3]. Breast cancer is usually subdivided into two major classes: ductal and lobular carcinomas based on their histological constituents. Moreover, based on their molecular characteristics, like the expression of progesterone receptor (PR), estrogen receptor (ER), and human epidermal growth factor receptor 2 (HER2), breast cancers are further categorized into luminal A (ER+ PR+, and HER2-), luminal B (ER+/PR+ and HER2+/−), HER2 positive (ER−/PR− and HER2+), triple-negative/basal-like (ER−, PR−, and HER2−), and claudin-low [4][5][6]. Also, the American Joint Committee on Cancer (AJCC) defined eight stages of breast cancer based on tumor-node metastasis (TNM) [7][8]. Treatment modalities for breast cancer have been designed by taking into consideration the molecular portrait of heterogenicity, receptor expression, and stages of breast cancers to improve therapeutic performances. Early detected breast cancers are not lethal and curable in most of the cases (72–80%), while advanced-stage breast cancers are life-threatening and the leading cause of breast cancer-induced deaths owing to their metastasis to distant vital organs like the liver, lungs, brain, lymph nodes, and bone [9]. However, treatment has been designed aiming to increase life span with minimum unintended and undesirable side effects for improved quality of life. Current cancer treatment modalities are based on two major pillars, including localized treatment and systemic therapy. Surgical intervention is the first therapeutic option for early-stage nonmetastatic breast cancer patients. On the other hand, treatment options for locally advanced breast cancer include mastectomy or lumpectomy, chemotherapy, and high energy waves radiation therapy [10]. To date, systemic therapies including endocrine therapy, targeted therapy, and immunotherapy have been added based on the type and stage of breast cancer to get better therapeutic efficacy than the conventional ones. Although conventional treatment strategies are successful to some degree, their significant drawbacks like limited accessibility of a drug to distant tumor cells, higher therapeutic dose, nonspecific targeting, uneven biodistribution, and unwanted side effects, limit the efficiency of the therapy. Besides, multidrug resistance (MDR) of cancer cells against chemotherapeutic agents is another reason for chemotherapy failure. Chemoresistance may develop by modulating the influx or efflux of drugs, by activating survival pathways, or by augmenting DNA repair mechanisms to lessen the cytotoxic effects of the drug [1][11]. Therefore, the development of new modalities is desirable for cancer management that can specifically target cancer cells, thereby lowering the unwanted adverse effects with improved anticancer effects. In this regard, cancer nanomedicine has been introduced for the last few decades to promote the targeted delivery of chemotherapeutics to target tumor sites and to thus improve the therapeutic index. Nanoparticles (NPs) (10 to 400 nm) have added a new dimension in the drug delivery concept, providing an unprecedented opportunity to revolutionize cancer therapy and management. The immense potentiality of NPs as a drug carrier for specific identification and destruction of cancer cells led to an increased interest to study various biocompatible and biodegradable nanocarriers for the delivery of anticancer agents both in preclinical and clinical trials [12][13][14]. Considering the drawbacks of conventional therapies, NP-based drug delivery is a useful toolkit particularly for site-specific drug delivery, improved drug accumulation in tumor site due to the enhanced permeability and retention (EPR) effect, and the capability to bypass the MDR effects of the breast cancer cell [15][16][17][18]. In modern therapy, NPs can be further modified by equipping contrast agents, termed as theranostics for cancer diagnosis and treatment simultaneously [19]. In this review, we discuss different approaches to the targeted delivery of nanotherapeutics to cancer cells. We present a comprehensive review of the current applications and preclinical studies of various actively targeted nanoparticles for specific delivery of different chemotherapeutics agents used for the management of breast cancer. Finally, we shed light on the challenges and translational gap of receptor-targeted drug delivery and on the direction to future studies for its safer human use.
2. Insights of NP-Based Targeted Drug Delivery
Extensive research on cancer therapeutics introduce several new paradigms to surmount conventional treatment drawbacks over the years. Upon systemic administration, chemotherapeutic drugs have to face several hurdles like premature degradation before reaching the target site, uneven biodistribution, and failure to discriminate healthy and cancer cells in addition to the requirement for their larger and repeated administration [20][21][22][23]. These barriers are considered responsible for severe unwanted side effects and high treatment costs of conventional chemotherapy [24][25]. Thus, a new way of delivering drugs specifically into a target tumor cell is a prerequisite to maximizing therapeutic efficacy and patient compliance. Emerging as a leading contender in the field of targeted drug delivery, NP-based therapeutics comprise therapeutic molecules such as small molecule drugs, peptides/proteins, and nucleic acids (genes and siRNAs) encapsulated into or associated with nanomaterials like liposomes [26][27], polymeric NPs [28][29], and inorganic NPs [30][31]. Since August 2014, 74 completed clinical trials and 57 trails with the status of “active” or “recruited” have been listed in clinicaltrials.gov, over 40,000 citations have been recorded in PubMed on NP-based drug delivery [21][32][33][34][35], and many more are on several stages of drug pipelines [17][36][37][38]. Preclinical studies showed NPs with loaded genes or drug-enhanced antitumor effects with an improved pharmacokinetic profile compared to free drugs [39][40][41] by virtue of the unique physicochemical properties of NPs, including loading capacity for both hydrophobic and hydrophilic drugs, ease of functionalization with targeting moieties and hydrophilic molecules, stability and extended half-lives in the systemic circulation, facilitated tumor accumulation due to their small particle size and EPR effect, enhanced cellular internalization via endocytosis, and quick and sustained release of the drugs in response to various intracellular (e.g., acidic pH) and extracellular (e.g., magnetic field, laser) stimuli [42][43][44]. Additionally, the size, conformation, and surface properties of NPs navigate the trajectory dynamics of the NP-loaded drug complex and are considered fundamental driving forces for improved delivery efficiency [45][46][47]. The passive targeting of NPs capitalizes on the anatomical variances of cancerous tissues. In solid tumors, rapid and abnormal angiogenesis results in an anomalous tumor microenvironment characterized by hyperpermeable tumor vasculature, poor lymphatic drainage, and unorganized extracellular matrix (ECM), allowing the nanocarriers to specifically penetrate through the fenestrate blood vessels and to be retained in the tumor tissue through the EPR effect [48][49][50]. The physicochemical properties and plasma half-life of NPs are considered the main factor for effective passive targeting, taking advantage of the EPR effect. A study showed that NPs with size range of 10–200 nm are enough to avoid clearance by the kidney and reticuloendothelial system (RES) and to facilitate maximum extravasation in the tumor site, whereas NPs with a surface charge slightly negative or neutral are considered ideal for avoiding protein corona effects [51][52][53][54][55]. However, passive targeting regulates tumor accumulation without triggering cellular entry, and a recent meta-study showed less than 1% of injected NPs accumulated in the targeted tumor site even with a high EPR effect in the xenografted tumor [56]. Besides, the idea of the EPR effect does not apply to all tumors. On the other hand, active targeting utilizes homing devices like ligands on the surface of NPs to let them target specifically for binding with specific receptors explicitly expressed on cancerous cells (
). The combined effects of EPR and active targeting might increase the retention of drug-loaded NPs at the target tumor site and thus promote cellular drug uptake through receptor-mediated endocytosis (
). In the last 10 years, more than 40,000 studies on active targeting of NPs have been reported, with few of them in the clinical trial [17][37][38]. A large number of targeting ligands including proteins, polysaccharide, nucleic acid, peptides, antibodies, and endogenous hormone have been employed for the construction of actively targeting NPs [57][58][59][60]. Usually, NPs can be functionalized with the targeting moiety by either chemical conjugation or a physical adsorption process. Modification of NPs with specific ligands targeting unique and overexpressed receptors or antigens on tumor cells is supposed to deliver the drug to the target tumor cells without hampering normal cells. Few studies reported that dual receptor-targeting strategies, multivalent binding, and use of a higher density of ligands are beneficial for maximizing binding affinity [61][62]. Despite having substantial successful preclinical studies, active targeting suffers from several limitations like poor penetration of the abnormal tumor microenvironment, relative hypoxia, an unknown endosomal escape mechanism, and relatively complex manufacturing steps for large-scale production. These shortcomings could be resolved by applying adjuvant therapy like vascular normalizing agents and other agents, such as TNF-α and angiotensin-II. Additionally, pH-responsive carbonate apatite (CA) (
) and strontium sulfite NPs could be employed to ensure quick release of the drugs from the NPs and subsequent endosomal escape of the free drugs at early endosomal stage [30]. A schematic diagram in
shows how fibronectin-coated CA NPs could facilitate specific-integrin-targeted drug delivery to cancer cells.
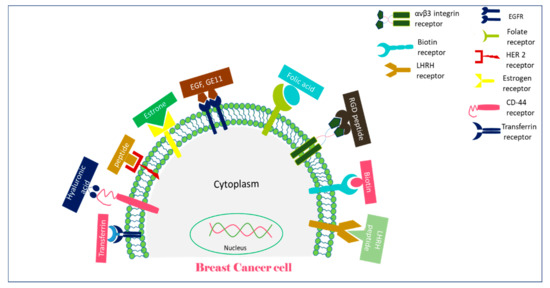
A schematic representation of receptors overexpressed on breast cancer cells and their targeting moieties for targeted breast cancer therapy.
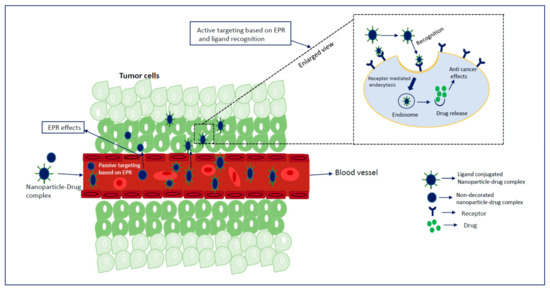
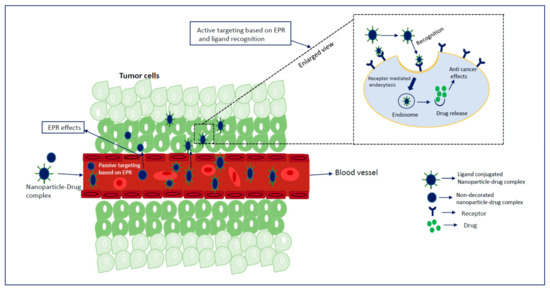
Combination strategy for drug targeting to a solid tumor using nanoparticles (NPs): after entering the systemic circulation, NPs are passively targeted and accumulated in the target tumor site by virtue of the enhanced permeability and retention (EPR) effect. Active targeting is achieved by decorating the surface of NPs with a targeting moiety and by capitalizing the advantages of aberrantly expressed receptors on the surface of tumor cells and EPR effects, resulting in improved drug delivery through receptor-mediated endocytosis.
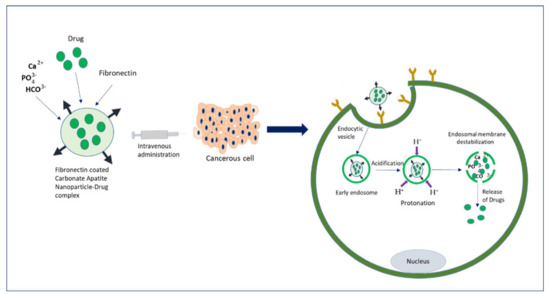
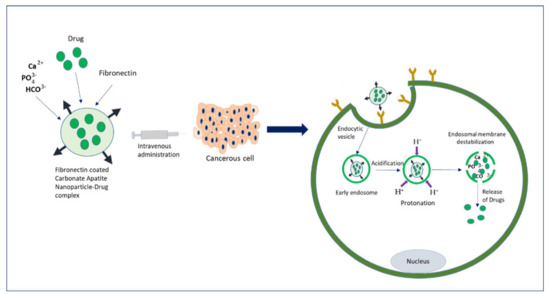
An overview of the drug delivery mechanism of fibronectin-coated pH-sensitive carbonate apatite (CA) NPs to the cancer cells expressing the fibronectin-specific integrin: upon systemic administration, drug-NP complexes are internalized into the target cell through specific integrin-mediated endocytosis. The acidic environment of an early endosome causes dissolution of the endocytosed NPs, resulting in their dissolution and release of the drugs, an event that might lead to endosomal membrane destabilization through accumulated ion-induced osmotic pressure, triggering quick release of drugs into the cytosol.
References
- Pashayan, N.; Antoniou, A.C.; Ivanus, U.; Esserman, L.J.; Easton, D.F.; French, D.; Sroczynsk, G.; Hall, P.; Cuzick, J.; Evans, D.G.; et al. Personalized early detection and prevention of breast cancer: ENVISION consensus statement. Nat. Rev. Clin. Oncol. 2020, 17, 687–705.
- Harbeck, N.; Penault-Llorca, F.; Cortes, J.; Gnant, M.; Houssami, N.; Poortmans, P.; Ruddy, K.; Tsang, J.; Cardoso, F. Breast cancer (Primer). Nat. Rev. Dis. Primers 2019.
- Muley, H.; Fadó, R.; Rodríguez-Rodríguez, R.; Casals, N. Drug uptake-based chemoresistance in breast cancer treatment. Biochem. Pharmacol. 2020, 177, 113959.
- Amjad, E.; Asnaashari, S.; Sokouti, B.; Dastmalchi, S. Systems biology comprehensive analysis on breast cancer for identification of key gene modules and genes associated with TNM-based clinical stages. Sci. Rep. 2020, 10, 10816.
- Tran, P.; Lee, S.-E.; Kim, D.-H.; Pyo, Y.-C.; Park, J.-S. Recent advances of nanotechnology for the delivery of anticancer drugs for breast cancer treatment. J. Pharm. Investig. 2020, 50, 261–270.
- Mittal, P.; Singh, S.; Singh, A.; Singh, I.K. Current advances in drug delivery systems for treatment of Triple negative breast cancer (TNBC). Chem. Biol. Lett. 2020, 7, 1–12.
- Koh, J.; Kim, M.J. Introduction of a new staging system of breast cancer for radiologists: An emphasis on the prognostic stage. Korean J. Radiol. 2019, 20, 69–82.
- Cserni, G.; Chmielik, E.; Cserni, B.; Tot, T. The new TNM-based staging of breast cancer. Virchows Arch. 2018, 472, 697–703.
- Grobmyer, S.R.; Zhou, G.; Gutwein, L.G.; Iwakuma, N.; Sharma, P.; Hochwald, S.N. Nanoparticle delivery for metastatic breast cancer. Nanomed. Nanotechnol. Biol. Med. 2012, 8, S21–S30.
- Mutebi, M.; Anderson, B.O.; Duggan, C.; Adebamowo, C.; Agarwal, G.; Ali, Z.; Bird, P.; Bourque, J.M.; DeBoer, R.; Gebrim, L.H.; et al. Breast cancer treatment: A phased approach to implementation. Cancer 2020, 126, 2365–2378.
- Sridharan, S.; Howard, C.M.; Tilley, A.M.; Subramaniyan, B.; Tiwari, A.K.; Ruch, R.J.; Raman, D. Novel and Alternative Targets Against Breast Cancer Stemness to Combat Chemoresistance. Front. Oncol. 2019, 9, 1003.
- Davis, M.E.; Chen, Z.; Shin, D.M. Nanoparticle therapeutics: An emerging treatment modality for cancer. Nanosci. Technol. A Collect. Rev. Nat. J. World Sci. 2010, 239–250.
- Alqaraghuli, H.G.J.; Kashanian, S.; Rafipour, R. A Review on Targeting Nanoparticles for Breast Cancer. Curr. Pharm. Biotechnol. 2019, 20, 1087–1107.
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic: An update. Bioeng. Transl. Med. 2019, 4, e10143.
- Van der Meel, R.; Sulheim, E.; Shi, Y.; Kiessling, F.; Mulder, W.J.; Lammers, T. Smart cancer nanomedicine. Nat. Nanotechnol. 2019, 14, 1007–1017.
- Peer, D.; Karp, J.M.; Hong, S.; Farokhzad, O.C.; Margalit, R.; Langer, R. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2007, 2, 751–760.
- Kumari, P.; Ghosh, B.; Biswas, S. Nanocarriers for cancer-targeted drug delivery. J. Drug Target. 2016, 24, 179–191.
- Piddock, L.J. Multidrug-resistance efflux pumps? Not just for resistance. Nat. Rev. Microbiol. 2006, 4, 629–636.
- Prasad, R.; Jain, N.K.; Yadav, A.S.; Chauhan, D.S.; Devrukhkar, J.; Kumawat, M.K.; Shinde, S.; Gorain, M.; Thakor, A.S.; Kundu, G.C.; et al. Liposomal nanotheranostics for multimode targeted in vivo bioimaging and near-infrared light mediated cancer therapy. Commun. Biol. 2020, 3, 1–14.
- Nag, O.K.; Delehanty, J.B. Active cellular and subcellular targeting of nanoparticles for drug delivery. Pharmaceutics 2019, 11, 543.
- Blanco, E.; Shen, H.; Ferrari, M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015, 33, 941.
- Hamidi, M.; Azadi, A.; Rafiei, P.; Ashrafi, H. A pharmacokinetic overview of nanotechnology-based drug delivery systems: An ADME-oriented approach. Crit. Rev. Ther. Drug Carr. Syst. 2013, 30, 435–467.
- Yang, R.; Wei, T.; Goldberg, H.; Wang, W.; Cullion, K.; Kohane, D.S. Getting drugs across biological barriers. Adv. Mater. 2017, 29, 1606596.
- Anselmo, A.C.; Mitragotri, S. An overview of clinical and commercial impact of drug delivery systems. J. Control. Release 2014, 190, 15–28.
- Bender, A.; Scheiber, J.; Glick, M.; Davies, J.W.; Azzaoui, K.; Hamon, J.; Urban, L.; Whitebread, S.; Jenkins, J.L. Analysis of pharmacology data and the prediction of adverse drug reactions and off-target effects from chemical structure. ChemMedChem 2007, 2, 861–873.
- Torchilin, V.P. Recent advances with liposomes as pharmaceutical carriers. Nat. Rev. Drug Discov. 2005, 4, 145–160.
- Mo, R.; Jiang, T.; Gu, Z. Recent progress in multidrug delivery to cancer cells by liposomes. Nanomedicine 2014, 9, 1117–1120.
- Shih, H.; Lin, C.-C. Photoclick hydrogels prepared from functionalized cyclodextrin and poly (ethylene glycol) for drug delivery and in situ cell encapsulation. Biomacromolecules 2015, 16, 1915–1923.
- Palanikumar, L.; Al-Hosani, S.; Kalmouni, M.; Nguyen, V.P.; Ali, L.; Pasricha, R.; Barrera, F.N.; Magzoub, M. pH-responsive high stability polymeric nanoparticles for targeted delivery of anticancer therapeutics. Commun. Biol. 2020, 3, 1–17.
- Karim, M.; Shetty, J.; Islam, R.A.; Kaiser, A.; Bakhtiar, A.; Chowdhury, E.H. Strontium Sulfite: A New pH-Responsive Inorganic Nanocarrier to Deliver Therapeutic siRNAs to Cancer Cells. Pharmaceutics 2019, 11, 89.
- Jin, H.; Pi, J.; Yang, F.; Jiang, J.; Wang, X.; Bai, H.; Shao, M.; Huang, L.; Zhu, H.; Yang, P.; et al. Folate-chitosan nanoparticles loaded with ursolic acid confer anti-breast cancer activities in vitro and in vivo. Sci. Rep. 2016, 6, 30782.
- Khalid, M.; El-Sawy, H.S. Polymeric nanoparticles: Promising platform for drug delivery. Int. J. Pharm. 2017, 528, 675–691.
- Brannon-Peppas, L.; Blanchette, J. Nanoparticle and targeted systems for cancer therapy. Adv. Drug Deliv. 2012, 56, 1649–1659.
- Saraiva, C.; Praça, C.; Ferreira, R.; Santos, T.; Ferreira, L.; Bernardino, L. Nanoparticle-mediated brain drug delivery: Overcoming blood–brain barrier to treat neurodegenerative diseases. J. Control. Release 2016, 235, 34–47.
- Rosenblum, D.; Joshi, N.; Tao, W.; Karp, J.M.; Peer, D. Progress and challenges towards targeted delivery of cancer therapeutics. Nat. Commun. 2018, 9, 1–12.
- Koo, O.M.; Rubinstein, I.; Onyuksel, H. Role of nanotechnology in targeted drug delivery and imaging: A concise review. Nanomed. Nanotechnol. Biol. Med. 2005, 1, 193–212.
- Anselmo, A.; Mitragotri, S. Nanoparticles in the clinic. Bioeng Transl Med 2016, 1, 10–29.
- Shi, J.; Kantoff, P.W.; Wooster, R.; Farokhzad, O.C. Cancer nanomedicine: Progress, challenges and opportunities. Nat. Rev. Cancer 2017, 17, 20.
- Haque, S.T.; Karim, M.; Abidin, S.A.Z.; Othman, I.; Holl, M.M.B.; Chowdhury, E.H. Fe/Mg-Modified Carbonate Apatite with Uniform Particle Size and Unique Transport Protein-Related Protein Corona Efficiently Delivers Doxorubicin into Breast Cancer Cells. Nanomaterials 2020, 10, 834.
- Karim, E.; Rosli, R.; HChowdhury, E. Systemic delivery of nanoformulations of anti-cancer drugs with therapeutic potency in animal models of cancer. Curr. Cancer Ther. Rev. 2016, 12, 204–220.
- Karim, M.; Tha, K.K.; Othman, I.; Borhan Uddin, M.; Chowdhury, E.H. Therapeutic potency of nanoformulations of siRNAs and shRNAs in animal models of cancers. Pharmaceutics 2018, 10, 65.
- Mura, S.; Nicolas, J.; Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 2013, 12, 991–1003.
- Foy, S.P.; Manthe, R.L.; Foy, S.T.; Dimitrijevic, S.; Krishnamurthy, N.; Labhasetwar, V. Optical imaging and magnetic field targeting of magnetic nanoparticles in tumors. ACS Nano 2010, 4, 5217–5224.
- Cole, A.J.; David, A.E.; Wang, J.; Galbán, C.J.; Hill, H.L.; Yang, V.C. Polyethylene glycol modified, cross-linked starch-coated iron oxide nanoparticles for enhanced magnetic tumor targeting. Biomaterials 2011, 32, 2183–2193.
- Tang, L.; Fan, T.M.; Borst, L.B.; Cheng, J. Synthesis and biological response of size-specific, monodisperse drug–silica nanoconjugates. ACS Nano 2012, 6, 3954–3966.
- Toy, R.; Peiris, P.M.; Ghaghada, K.B.; Karathanasis, E. Shaping cancer nanomedicine: The effect of particle shape on the in vivo journey of nanoparticles. Nanomedicine 2014, 9, 121–134.
- Anselmo, A.C.; Zhang, M.; Kumar, S.; Vogus, D.R.; Menegatti, S.; Helgeson, M.E.; Mitragotri, S. Elasticity of nanoparticles influences their blood circulation, phagocytosis, endocytosis, and targeting. ACS Nano 2015, 9, 3169–3177.
- Rosenblum, D.; Peer, D. Omics-based nanomedicine: The future of personalized oncology. Cancer Lett. 2014, 352, 126–136.
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: Mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46 Pt 1, 6387–6392.
- Soussan, E.; Cassel, S.; Blanzat, M.; Rico-Lattes, I. Drug delivery by soft matter: Matrix and vesicular carriers. Angew. Chem. Int. Ed. 2009, 48, 274–288.
- Hobbs, S.K.; Monsky, W.L.; Yuan, F.; Roberts, W.G.; Griffith, L.; Torchilin, V.P.; Jain, R.K. Regulation of transport pathways in tumor vessels: Role of tumor type and microenvironment. Proc. Natl. Acad. Sci. USA 1998, 95, 4607–4612.
- Li, S.-D.; Huang, L. Pharmacokinetics and biodistribution of nanoparticles. Mol. Pharm. 2008, 5, 496–504.
- Yu, B.; Tai, H.C.; Xue, W.; Lee, L.J.; Lee, R.J. Receptor-targeted nanocarriers for therapeutic delivery to cancer. Mol. Membr. Biol. 2010, 27, 286–298.
- Wisse, E.; Braet, F.; Luo, D.; De Zanger, R.; Jans, D.; Crabbe, E.; Vermoesen, A. Structure and function of sinusoidal lining cells in the liver. Toxicol. Pathol. 1996, 24, 100–111.
- Sadauskas, E.; Wallin, H.; Stoltenberg, M.; Vogel, U.; Doering, P.; Larsen, A.; Danscher, G. Kupffer cells are central in the removal of nanoparticles from the organism. Part. Fibre Toxicol. 2007, 4, 1–7.
- Wilhelm, S.; Tavares, A.J.; Dai, Q.; Ohta, S.; Audet, J.; Dvorak, H.F.; Chan, W.C.W. Analysis of nanoparticle delivery to tumours. Nat. Rev. Mater. 2016, 1, 1–12.
- Byrne, J.D.; Betancourt, T.; Brannon-Peppas, L. Active targeting schemes for nanoparticle systems in cancer therapeutics. Advanced Drug Deliv. Rev. 2008, 60, 1615–1626.
- Kurmi, B.D.; Patel, P.; Paliwal, R.; Paliwal, S.R. Molecular approaches for targeted drug delivery towards cancer: A concise review with respect to nanotechnology. J. Drug Deliv. Sci. Technol. 2020, 57, 101682.
- Das, M.; Mohanty, C.; Sahoo, S.K. Ligand-based targeted therapy for cancer tissue. Expert Opin. Drug Deliv. 2009, 6, 285–304.
- Pérez-Herrero, E.; Fernández-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79.
- Yoo, J.; Park, C.; Yi, G.; Lee, D.; Koo, H. Active targeting strategies using biological ligands for nanoparticle drug delivery systems. Cancers 2019, 11, 640.
- Vhora, I.; Patil, S.; Bhatt, P.; Gandhi, R.; Baradia, D.; Misra, A. Receptor-targeted drug delivery: Current perspective and challenges. Ther. Deliv. 2014, 5, 1007–1024.
