Severe mitral valve regurgitation (MR) carries a significant burden both in prognosis and quality of life of patients, as well as on healthcare systems, with high rates of hospitalization for heart failure. While mitral valve surgery constitutes the first-line treatment option for primary MR in suitable patients, surgical treatment for secondary severe MR remains controversial, with a substantial lack of evidence on a survival benefit. In recent decades, percutaneous mitral valve repair has emerged as an alternative treatment for patients deemed not suitable for surgery. Among several devices under development or evaluation, the MitraClip system is the most widespread and is supported by the strongest evidence. While the role of MitraClip in patients with chronic primary MR who are not deemed suitable for surgery is well established, with consistent data showing improvement in both prognosis and quality of life, MitraClip treatment in secondary MR is a rapidly evolving field. Two recent randomized clinical trials generated apparently controversial results but actually provided an interesting pathophysiologic frame that could help discerning patients who will benefit from the procedure versus patients who will not. In this review, we will discuss current treatment options for mitral regurgitation, focusing on percutaneous mitral valve repair with the MitraClip system.
- Mitral Valve Repair
- heart failure
- mitraclip
- mitral regurgitation
1. Mitral Valve Anatomy and Mitral Valve Regurgitation
The mitral valve apparatus comprises four main components: mitral valve leaflets (anterior and posterior), mitral annulus, chordae tendineae and papillary muscles. Normal mitral valve function allows unidirectional blood flow from the left atrium (LA) to the left ventricle (LV) during diastole, avoiding blood regurgitation in the opposite direction during systole. Mitral valve closing relies on a complex balance between the tethering forces of chordae tendineae and mitral annulus and the closing force generated by LV contraction that results in appropriate coaptation and symmetrical apposition of the leaflets. Any anatomical and/or functional abnormality of one or more of these structures can lead to mitral regurgitation[1].
Primary (degenerative) mitral regurgitation is related to anatomical abnormality of valve leaflets and/or chordae tendinae, while secondary (functional) mitral regurgitation occurs in the setting of LV dilation and systolic dysfunction, which compromises the tethering forces through annular dilation and retraction or displacement of papillary muscle/chordae tendinae, as well as the closing forces due to systolic dysfunction/dyssynchrony [1][2][3][4][5].
Table 1. Functional Carpentier classification [6] of mitral regurgitation and commonest underlying etiologies.
| Leaflet Motion | Lesion | Etiology |
| Type I: normal leaflet motion | Annular dilation/distortion Leaflet perforation |
Dilated cardiomyopathy, left atrial dilation, Endocarditis |
| Type II: excess leaflet motion (prolapse/flail) | Chordal elongation/rupture Papillary muscle rupture |
Degenerative valve disease Ischemic cardiomyopathy, trauma, endocarditis |
| Type IIIA: restricted systo-diastolic leaflet motion | Leaflet and/or chordae thickening/retraction, leaflet calcification/fusion, commissural fusion | Rheumatic heart disease, carcinoid heart disease, dilated cardiomyopathy, radiation |
| Type IIIB: restricted systolic leaflet motion | Papillary muscle displacement or chordal tethering | Ischemic or dilated cardiomyopathy |
2. Pathophysiology and Natural History
In chronic MR, there is an initial compensated stage in which eccentric remodeling of LV can preserve an appropriate forward cardiac output by the increase in LV diastolic volume and stroke volume. However, with progressive LV dilation, LV systolic dysfunction eventually occurs, and there is a progressive hemodynamic compromise with reduction of forward cardiac output and progressive increase in pulmonary venous pressure[7][8][9][10].
If not treated, severe MR is associated with poor prognosis irrespective of its etiology, and heart failure (HF) symptoms development, new-onset atrial fibrillation, LV systolic dysfunction and increase in systolic pulmonary artery pressure (sPAP) constitute the main factors associated with worse outcomes[11][12][13][14][15].
3. Mitral Regurgitation Assessment and Grading
2
and a regurgitant volume (RVol) > 60 mL indicate severe primary mitral regurgitation, while in secondary MR, lower cutoffs are used (EROA > 20 mm2; RVol > 30 mL) due to evidence supporting a negative prognostic impact of secondary MR above those values [16][17][18][19]. The PISA method is based on the assumption of hemispheric symmetry of the velocity distribution proximal to the circular regurgitant lesion, which may not hold for eccentric jets, multiple jets, or complex or elliptical regurgitant orifices. Practically, the geometry of the PISA varies depending on the shape of the orifice and mitral valve leaflets surrounding the orifice. In functional MR, the PISA might look like an ellipsoidal shape, and two separate MR jets originating from the medial and lateral sides of the coaptation line can be observed on 2D echo. When the shape of the flow convergence zone is not a hemisphere, the PISA method may underestimate the degree of functional MR, and in every case the PISA method could not be applied, assessment of all the other parameters is needed. A list of the main echocardiographic parameters is shown in
; RVol > 30 mL) due to evidence supporting a negative prognostic impact of secondary MR above those values [16,17,18,19]. The PISA method is based on the assumption of hemispheric symmetry of the velocity distribution proximal to the circular regurgitant lesion, which may not hold for eccentric jets, multiple jets, or complex or elliptical regurgitant orifices. Practically, the geometry of the PISA varies depending on the shape of the orifice and mitral valve leaflets surrounding the orifice. In functional MR, the PISA might look like an ellipsoidal shape, and two separate MR jets originating from the medial and lateral sides of the coaptation line can be observed on 2D echo. When the shape of the flow convergence zone is not a hemisphere, the PISA method may underestimate the degree of functional MR, and in every case the PISA method could not be applied, assessment of all the other parameters is needed. A list of the main echocardiographic parameters is shown in [3,12,13,14,15].Table 2.
| Echocardiographic Parameters | Data/Values Suggestive of Severe MR | |||
| Parameters | Optimal Suitability | Suboptimal/Conditional Suitability | Qualitative |
|
| Pathology location | A2-P2 | A1-P1 or A3-P3 | · Morphologic assessment | Prolapse/flail, chordae or papillary muscle rupture |
| Calcification | Absent | Mild calcification, not in grasping zone, annular calcification | · Color flow MR Jet | Large central jet or eccentric jet reaching the posterior wall of LA |
| Leaflet mobility | Normal | Systolic restriction | · Flow convergence zone | |
| Mitral valve area | ≥4 cm2 | ≥3 cm2 | ||
| Coaptation depth † | <11 mm | ≥11 mm | ||
| Coaptation length † | ≥2 mm | <2 mm | ||
| Mobile length of PML | ≥10 mm | 7–10 mm | ||
| Flail width | ≤15 mm | >15 mm with large annulus size and with the possibility of multiple clip positioning | ||
| Flail gap | <10 mm |
Procedure contraindications are unfavorable anatomy, intolerance to procedural anticoagulation or post-procedural antiplatelet therapy, active endocarditis, rheumatic MV disease, mitral stenosis, femoral venous, superior vena cava (SVC) or inferior vena cava (IVC) thrombosis or intracardiac left-sided thrombosis or masses, life expectancy <1 year.
Complications: the main procedural and peri-procedural complications are pericardial effusion/tamponade, thrombus formation, access site bleeding, clip detachment from a single leaflet or device embolization, development of mitral stenosis, acute kidney injury and neurological events[36][37][38]. In the EVEREST II trial, major adverse events rate at 30 days was 15% [36]. In a subsequent meta-analysis also including EVEREST II, the weighted mean rate of major adverse effect at 30 days was 17%[37]. ACCESS-EU, a real-world post-approval study including a high risk, elderly population, mainly affected by secondary MR, demonstrated a 30 days major adverse events rate of 17% [39]. More recent trials on secondary MR, which will be later discussed in this review, demonstrated procedural complication rates of 8.5% and 14.6%[40][41].
6. MitraClip in the Current Practice for Primary MR
The 2017 ESC guidelines suggest evaluation for percutaneous mitral valve repair in symptomatic patients with severe primary MR who are judged inoperable or at high surgical risk (COR IIb, LOE C)[3]. This indication mainly derives from data of the EVEREST II trial.
In the EVEREST II trial, 279 patients with moderate-to-severe MR (according to ACC/AHA criteria) were randomized in a 2:1 ratio to undergo either MitraClip procedure or mitral valve surgery. At 12 months follow up, while there was no statistical significance in mortality between the two groups (6% in both groups), and residual ≥3 MR (21% vs. 20%) repeat surgery was more frequent in MitraClip group (20% vs. 2%), driving the primary composite endpoint of freedom from death, repeat surgery and residual ≥3 MR in favor of surgery [36]. A survival benefit comparable to surgery has also been confirmed at 5 years follow up[42]. MitraClip demonstrated a durable benefit on quality of life and functional status as well as HF hospitalization reduction at 1 year in REALISM study that enrolled patients at prohibitive risk for surgery[43].
7. MitraClip for Secondary MR Treatment
The 2017 ESC guidelines suggest evaluation for percutaneous mitral valve repair in symptomatic patients with severe LV dysfunction, without indication for coronary revascularization and at high risk for surgery (COR IIb, LOE C)[3]. These recommendations derived from the lack of evidence on survival benefit of the MitraClip procedure, whose indication is intended only for symptom relief. However, these guidelines do not incorporate the results of two recent trials, namely the COAPT and the MITRA -FR that raised new interest and potential new indications for MitraClip procedure in secondary MR in HFrEF patients.
7.1. COAPT Trial (Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation)
7.2. MITRA–FR
n
n
8. Similarities and Differences between COAPT and MITRA–FR
Although the two trials had a similar design and target population, i.e., symptomatic patients with HFrEF despite medical therapy and moderate to severe mitral regurgitation, they showed substantially opposite results: the COAPT study demonstrated a significant benefit in the device group on HF hospitalization and all-cause mortality at 24 months, as well as in the QOL assessment (NYHA functional class and KCCQ score), while MITRA–FR failed to show any difference either on 12 months mortality and HF hospitalization or on NYHA functional class improvement[40][41][44].
8.1. Medical and Device Therapy at the Baseline
8.2. Echocardiographic Parameters at Baseline
2
Table 5.
| Baseline Parameters | COAPT | MITRA–FR |
| Etiology of LV dysfunction Ischemic Non-ischemic |
60.7% 39.3% |
59.6% 40.4% |
| 31 ± 10 mm | ||
| 2 | ||
| EROA > 30 mm | ||
| 2 |
| Outcome | COAPT | MITRA–FR |
| Post-procedural residual MR ≤2 | 95% | 91% |
| LVEDV | 101 ± 34 mL/m2 | 135 ± 35 mL/m2 |
| Large flow convergence | ||
| · CW signal of MR jet | Dense/triangular | |
| Semi-quantitative | ||
| · Vena contracta width | ≥ 7mm | |
| · Pulmonary vein flow | Systolic flow reversal | |
| Quantitative | ||
| · EROA | ≥ 40 mm2 (≥20 mm2 in secondary MR) | |
| · Regurgitant volume | ≥ 60 ml (≥30 ml in secondary MR) | |
| · Regurgitant fraction | ≥50% | |
| Additional evaluation | ||
| · LV and LA size | Chamber dilation (may not be present in acute MR; in secondary MR may be a consequence of underlying LV dysfunction) | |
| · Estimated sPAP | > 50 mmHg |
4. Surgical Treatment of Mitral Regurgitation
In chronic primary MR, medical therapy of hypertension and/or HFrEF is recommended, if indicated. However, valve surgery (repairing when feasible or replacement) [20][21][22] is the preferred treatment for chronic primary MR. Surgery is indicated in symptomatic patients with severe MR and left ventricle ejection fraction (LVEF) > 30% (Class of recommendation, COR I; Level of evidence, LOE B). In symptomatic patients with severe LV dysfunction (LVEF < 30%, LVESD > 55 mm) refractory to medical therapy, surgery could be considered if the surgical risk is low and there are no major comorbidities (mitral valve repair: COR IIa, LOE C; mitral valve replacement: COR IIb, LOE C) [3]. Surgical treatment in asymptomatic patients is indicated if there are signs of LV dilation and dysfunction (LV EF < 60% or LVESD > 45 mm) (COR I, LOE B) or in patients with preserved LV function (LVEF > 60%, LVESD < 45 mm) presenting new-onset atrial fibrillation (AF) or sPAP > 50 mmHg (COR IIa, LOE B) or in patients with preserved LV function (LVEF > 60%, LVESD 40–44 mm) presenting flail leaflet or significant LA dilation (LAVI > 60 mL/m
2 in sinus rhythm) when there is high likelihood or durable valve repair (COR IIa, LOE C) [3][23][24].
In chronic secondary MR, medical and device (CRT if indicated) treatment of HFrEF is recommended[25][26][27], as well as treatment of underlying coronary artery disease, if present. Mitral valve surgery (either repair or replacement) failed to demonstrate a survival benefit in this setting [28][29][30] and only improves symptoms, so current guidelines suggest surgical treatment of secondary MR in patients with LVEF > 30% undergoing coronary artery bypass surgery (CABG) (COR I, LOE C) or symptomatic patients with LVEF < 30% with evidence of myocardial viability and an option for revascularization (COR IIa, LOE C). Mitral valve surgery in symptomatic patients without options for revascularization could be evaluated in patients with LVEF > 30% and low surgical risk (COR IIb, LOE C) [3]. As already mentioned before, mitral valve surgery in secondary MR lacks robust evidence derived from randomized clinical trial, since current guidelines’ indications refer to single-center retrospective studies. The newer interest in the field generated by the development of percutaneous mitral valve repair (PMVR) contributed to filling this gap in knowledge. The ongoing MATTERHORN trial will be the first randomized clinical trial directly comparing MV surgery VS MitraClip in the setting of severe secondary MR in surgical high-risk patients. Acute mitral regurgitation treatment is not the subject of this review and will not be discussed.
Table 3.
| Clinical Setting | Indication for Intervention | Intervention |
| Symptomatic chronic primary mitral regurgitation | · LVEF > 30% | Surgery (COR I, LOE B) |
| · LVEF < 30%, LVESD > 55 mm low surgical risk, no major comorbidities |
Repair (COR IIa, LOE C) or Replacement (COR IIb, LOE C) | |
| · LVEF < 30%, LVESD > 55 mm high surgical risk and/or major contraindication for surgery |
Edge to edge TMVR if feasible (COR IIb, LOE C) | |
| Asymptomatic chronic primary mitral regurgitation | · LVEF < 60% and/or LVESD > 45 mm | Surgery (COR I, LOE B) |
| · LVEF > 60% and new onset AF or sPAP > 50 mmHg | Surgery (COR IIa, LOE B) | |
| · LVEF >60% + LVESD 40–44 mm and flail leaflet or severe LA dilation; low surgical risk | Repair if high likelihood of durable repair (COR IIa, LOE C) | |
| Symptomatic chronic secondary mitral regurgitation | · LVEF > 30% undergoing CABG | Surgery (COR I, LOE B) |
| · LVEF > 30%, low surgical risk | Surgery (COR IIb, LOE C) | |
| · LVEF < 30% with myocardial viability and option for revascularization | Surgery (COR IIa, LOE C) | |
| · LVEF < 30%, high surgical risk | Edge to edge TMVR if feasible (COR IIb, LOE C); ventricular assist device or transplantation program (COR IIb, LOE C) |
5. Percutaneous Treatment of Mitral Regurgitation
MitraClip is a percutaneous mitral valve repair system that imitates the surgical Alfieri technique, which connects the middle segments of the mitral leaflets through surgical stitches in order to create a double valve orifice and reduce mitral regurgitation[31].
Figure 1). The patient is under general anesthesia and systemic anticoagulation with an activated clotting time (ACT) target > 250 s administered. The MitraClip itself is a cobalt chromium clip covered with a polypropylene fabric whose function is to grasp and approximate two opposite segments of the anterior and posterior leaflet. The clip is delivered percutaneously through a venous femoral access. Transseptal puncture is performed in order to introduce the clip delivery system into the left atrium and then into the left ventricle. Once in the left ventricle, the delivery system is steered and aligned over the origin of the regurgitant jet, and leaflet grasping is performed. In its most recent version, the MitraClip system allows for independent leaflets grasping. Once adequate grasping is obtained, desired position of the clip is confirmed and functional assessment of the mitral valve is done, the clip can be released from the delivery system or reopened and repositioned. Residual MR can be targeted by positioning additional clips[32]. Procedural success is defined as proper placement of the device without procedural mortality and with reduction in post-procedural MR by ≥1 grade from baseline and to an absolute level of ≤moderate MR.
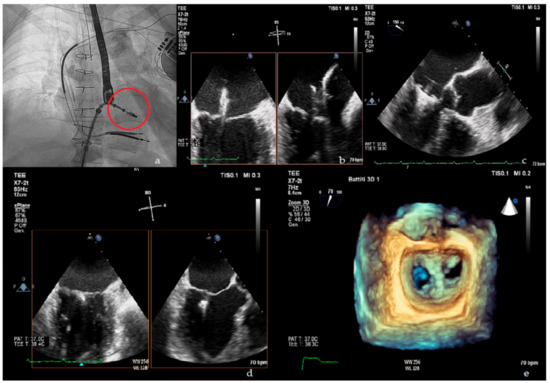
Figure 1.
Upper panel
a
b
c
Lower panel
d
e
Table 4 resumes the optimal suitability criteria as defined in the EVEREST trial[33], as well as suboptimal valve morphology criteria in which MitraClip procedure can still be performed, however with lower success rates [34][35].
resumes the optimal suitability criteria as defined in the EVEREST trial [33], as well as suboptimal valve morphology criteria in which MitraClip procedure can still be performed, however with lower success rates [34,35].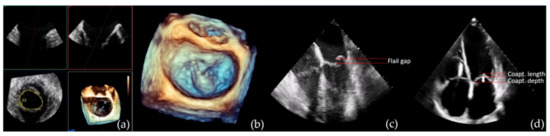
Figure 2.
a
b
c
d) transthoracic echocardiogram (TTE) four chamber view screening of coaptation depth and length in secondary MR.
Table 4.
| LVEF inclusion criteria | ||
| 86% | ||
| 1 year follow up residual ≥3 MR | 5% | |
| >20%, <50% | >15%, <40% | |
| Mean LVEF | 31% ± 9% | 33 ± 7% |
| EROA cutoff | >30 mm2 | >20 mm2 |
| Mean EROA | 41 ± 15 mm2 | 48% |
| Additional criteria | LVESD < 70 mm sPAP < 70 mmHg RV dysfunction < moderate |
8.3. Procedural Outcomes
| 17% | ||
| % of patients treated with >1 clip | 64% | 54% |
9. A New Concept in the Evaluation of MR Severity: Proportionate vs. Disproportionate MR
A new conceptual framework for comprehensive evaluation of secondary MR was proposed by Grayburn and colleagues[45].
In the proposed model, severe secondary MR is not defined with a fixed cut-off of EROA and regurgitant volume, but these parameters must be indexed to the degree of LV dilation and systolic dysfunction. As a consequence, in order to produce a severe MR, defined as a regurgitant fraction >50%, expected EROA and Regurgitant volume are different on each patient[46]. Using a different cutoff of EROA could further classify the patients into three groups:
- , is unlikely to be severe given the greater degree of LV dilation (moderate MR).
-
Patients whose MR severity is proportionate to the degree of LV dilation and dysfunction (proportionate MR).
-
Patients whose MR severity is unexpectedly more compared to their LV dilation and dysfunction (disproportionate MR).
-
Patients whose MR, despite an EROA > 20 mm2, is unlikely to be severe given the greater degree of LV dilation (moderate MR).
10. Conclusions
11. Open Questions
-
Whether proportionate and disproportionate secondary MR represent different stages of the same disease or different clinical entities is unclear.
-
A better understanding of pathophysiology of secondary MR could help identify early markers for disproportionate MR and thus prompt treatment.
-
Potential diagnostic performance improvement with cardiac MRI needs to be evaluated. Cardiac MRI could overcome the already mentioned limitations and potential underestimation of the PISA method in MR severity assessment, but current guidelines on valvular disease, as well as the trials on MR treatment presented in this review, does not include it in the diagnostic/therapeutic workup; thus it is still not known if a performance improvement in severity assessment could translate into better patients selection and/or better outcomes; moreover, recent studies have shown possible prognostic implications of left ventricular scar extension detected with cardiac magnetic resonance imaging in patients with secondary mitral regurgitation[51].
-
Potential diagnostic performance improvement with cardiac MRI needs to be evaluated. Cardiac MRI could overcome the already mentioned limitations and potential underestimation of the PISA method in MR severity assessment, but current guidelines on valvular disease, as well as the trials on MR treatment presented in this review, does not include it in the diagnostic/therapeutic workup; thus it is still not known if a performance improvement in severity assessment could translate into better patients selection and/or better outcomes; moreover, recent studies have shown possible prognostic implications of left ventricular scar extension detected with cardiac magnetic resonance imaging in patients with secondary mitral regurgitation [51].
- Patients whose MR severity is proportionate to the degree of LV dilation and dysfunction (proportionate MR).
-
Patients whose MR severity is unexpectedly more compared to their LV dilation and dysfunction (disproportionate MR).
-
Patients whose MR, despite an EROA > 20 mm2
Controversies of the “Disproportionate MR” Framework
All these results are limited from the small sample size, the post-hoc setting of the analyses, and the same limitations and differences of the main trials already mentioned before (medical therapy and exclusions criteria, in particular exclusion of patients with severe RV dysfunction, severe pulmonary hypertension and/or severe tricuspid regurgitation in COAPT but not in MITRA–FR). Taken together, we can conclude that the disproportionate MR framework is an interesting theoretic model that is, however, not readily applicable in clinical practice to make therapeutic choices in the individual patient[50]. Together with anatomic, echocardiographic and clinical selection criteria applied in the different trials, a special emphasis should be dedicated to the optimization of medical treatment before eventual percutaneous mitral valve repair.
Beyond MitraClip: In addition to the MitraClip system, several PMVR systems are currently under investigation. One of these is the Edwards PASCAL system, an edge-to-edge mitral valve repair system that has been shown promising results both in safety and efficacy in the 30 days data of the CLASP study
[
52], as well as a potential to extend MR treatment to patients who do not fulfill eligibility criteria for MitraClip. Moreover, a further therapeutic approach in the treatment of severe mitral regurgitation is represented by a transcatheter mitral valve replacement (TMVR) treatment; this procedure has emerged as a potential therapy for inoperable or high–surgical risk patients with symptomatic mitral regurgitation. The early feasibility of TMVR has been demonstrated in several prior studies[53], with the Tendyne system (Abbott Structural, Santa Clara, CA, USA) representing the largest experience.
Beyond MitraClip: In addition to the MitraClip system, several PMVR systems are currently under investigation. One of these is the Edwards PASCAL system, an edge-to-edge mitral valve repair system that has been shown promising results both in safety and efficacy in the 30 days data of the CLASP study [52], as well as a potential to extend MR treatment to patients who do not fulfill eligibility criteria for MitraClip. Moreover, a further therapeutic approach in the treatment of severe mitral regurgitation is represented by a transcatheter mitral valve replacement (TMVR) treatment; this procedure has emerged as a potential therapy for inoperable or high–surgical risk patients with symptomatic mitral regurgitation. The early feasibility of TMVR has been demonstrated in several prior studies [53], with the Tendyne system (Abbott Structural, Santa Clara, CA, USA) representing the largest experience.
