Interferons (IFNs) are a heterogenous group of proteins that can be classified into three families (Type I, II, and III) based on distinct functions and characteristics. The family of human type I IFN is composed of 5 subgroups: IFN-α, -β, -κ, -ε, and -ω, whereas the type II IFN group only contains IFN-γ. Type III IFNs are composed of four IFN-λ proteins.
- Interferons
- innate immunity
- immune regulation
- type I interferon
1. Introduction
Type I IFNs all bind to a common heterodimeric receptor consisting of the IFN-α/β R1 (IFNAR1) and IFN-α/β R2 (IFNAR2) subunits [1][2][3][7,8,9], which are expressed on most cell types. Binding of type I IFNs to their receptor causes receptor subunit dimerization [4][10], rapid activation of the R2 subunit associated Janus kinase 1 (JAK1) [5][6][11,12], and subsequently induction of the JAK-STAT pathway [7][13]. This tyrosine kinase auto-phosphorylates and additionally phosphorylates specific residues within the interaction sites of the intracellular domain of the receptor, revealing signal transducer and activator of transcription (STAT) binding pockets [8][14]. After binding of the STAT proteins via their Src-homology 2 (SH2) domains, STATs get phosphorylated by activated JAK1, leading to their dissociation from the receptor. IFN-α induces the formation of STAT1/STAT2 heterodimers [9][15], which can further associate with interferon regulatory factor 9 (IRF9), and subsequently form the IFN-stimulated gene factor 3 (ISGF3) [10][16]. The ISGF3 translocates into the nucleus to bind interferon stimulated response elements (ISREs), inducing antiviral response genes [9][11][12][15,17,18]. Furthermore, STAT1 can form homodimers or heterodimers with STAT3. STAT1, STAT3, STAT4, STAT5, and STAT6 form homodimers. Dimerization precedes translocation into the nucleus and activation of genes regulated by a gamma interferon activation site (GAS) [13][14][15][19,20,21], causing a pro-inflammatory response (Figure 1).
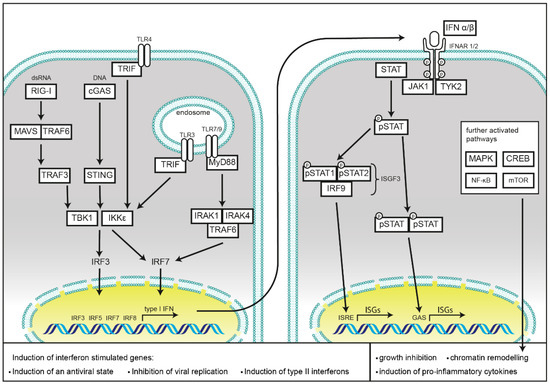
Figure 1.
Binding of IFN-α to its receptor also leads to rapid phosphorylation of receptor subunit R1 associated tyrosine kinase Tyk2 [16][17][18][19][22,23,24,25], which mediates signaling to non-IFN pathways. This results in initiation of the MAP kinase pathway, activation of p38 and subsequent growth inhibition [20][26], as well as chromatin remodeling upon translocation of the Cre binding element (CREB) [21][27]. Furthermore, Tyk2 activates phosphoinositide-3-kinase (PI3-K), resulting in the activation of the mammalian target of rapamycin (mTOR) pathway and initiation of mRNA translation, as well as activation of the pro-inflammatory nuclear factor ‘kappa-light-chain-enhancer’ of activated B-cells (NF-κB) pathway [22][28].
2. Immune Response to Infection and Tissue Tolerance are Influenced by the Type I Interferon Response
Viruses interact with a broad range of proteins in mammalian cells, and their evolution has been driven by antiviral constraints and adaptation of their host cells. It is hence not surprising that their co-evolution has resulted in highly sophisticated regulatory mechanisms of the timing and amplitude of immune responses to viral challenges. Type I IFNs have a central role in controlling viral infections and are also involved in the defense of other pathogens. In 1957, IFNs were discovered by Alick Isaacs and Jean Lindenmann, as a soluble factor in the supernatant of chorio-allantoic membrane, challenged with heat inactivated influenza virus, that interferes with the viral infection in cells, hence the name “interferon” [23][29]. Type I IFNs act both in an autocrine and paracrine manner, and prime bystander cells for upcoming viral infection by the latter. Their ability to restrict viral replication is mainly driven by a multitude of interferon-stimulated genes (ISGs). Furthermore, type I IFNs play an important role in the activation of cells that are involved in the development of the adaptive immune response. Here type I IFNs take part in the control of cell expansion and differentiation and determining cytokine and chemokine responses of cells of the lymphoid lineage [24][30].
Type I IFNs are associated with the rapid induction of a cellular antiviral state, and most cells can produce them in response to an appropriate pattern-recognition receptor (PRR) stimulation. They prime the infected cells, as well as the surrounding cells towards a state of either defense or tolerance [25][31]. Their importance as protective factors during viral infections was proven by showing the high susceptibility of mice deficient in the IFNAR1 receptor (Ifnar1−/− mice) to vesicular stomatitis virus (VSV), Semliki Forest virus, vaccinia virus (VACV), and lymphocytic choriomeningitis virus (LCMV) [26][32]. Furthermore, mice with STAT1 deficiency were shown to be highly susceptible to influenza viruses [27][33], further cementing the importance for type I IFNs in antiviral responses. In humans, several forms of inherited STAT1 deficiencies are associated with a high susceptibility to intracellular bacteria and viruses [28][34], while some gain-of-function STAT1 mutations are responsible for the development of chronic mucocutaneous candidiasis [29][35].
In bacterial infections, the functions of type I IFNs are more complex, as they can influence host defense either positively or negatively [24] [30]. Type I IFN treatment of macrophages results in better restriction of bacterial replication during infection with intracellular Legionella pneumophilia or Bacillus anthracis [30][31][32][33][36,37,38,39]. Furthermore, type I IFN appears to protect cells from invasion by Salmonella enterica subsp. enterica ser. Typhimurium (S. Thphimurium) and Shigella flexneri, as mice treated with recombinant type I IFN showed reduced numbers of invasive bacteria in epithelial cells and improved survival [34][35][40,41]. Type I IFNs contribute to the activation of macrophages, regarding production of nitric oxide (NO) and TNFα [36][42]. However, IFN-α and -β have also been identified as negative regulators of many of the cytokines and chemokines, orchestrating immune responses to bacterial infections, in particular for Listeria monocytogenes [37][38] [43,44] and S. Thphimurium [38][39] [44,45] (reviewed in [40][46]).
Besides bacteria, recognition of fungi, most importantly by the C-type lectin receptor Dectin-1, but also of fungal nucleic acids by Toll-like receptor 7 (TLR7) and TLR9 induces robust type I interferon responses [41][42][47,48]. However, as with bacterial infections, type I interferons can also be supportive for pathogen survival [43][49].
Type I IFNs are of equal importance in orchestrating adaptive immune responses to infection by transcriptional regulation of a broad range of target genes. Notably, type I IFNs induce and support the production of type II IFNs, mainly IFN-γ in NK cells directly [44][45][50,51], and support production of IL-12 in dendritic cells (DCs) [46][52]. They can further enhance responses of myeloid cells, B cells, and T cells upon viral infection, leading to improved clearance of viruses and to establishment of a robust adaptive T and B cell memory repertoire. In antigen presentation, IFN-γ induces the transcription of MHC class I and class II by inducing the expression of two NLR family members, caspase activation and recruitment domain (CARD) containing 5 (NLRC5) and MHC class II transcriptional activator (CIITA), respectively [47][48][53,54]. Meanwhile it was found that the expression of many other NLRs is regulated by both type I and type II IFNs. In the following section, we describe in detail how NLRs are regulated by type I IFNs and how they modulate the outcome of type I IFN responses. We discuss how deregulation of NLRs can result in susceptibility to either infection or auto-inflammatory disease as a consequence of pathogen dissemination or a lowered tissue tolerance to stress damage.
3. Induction of Type I Interferon Response by Nucleic Acid Sensing
Recognition of pathogen-associated molecular patterns (PAMPs) by evolutionary conserved PRRs is the initial step for mounting of a rapid innate immune response. After sensing potentially noxious non-self molecules, PRRs activate a defined set of signaling cascades, culminating in induction of a state of tolerance or defense in the host cell. This allows the production and release of cytokines, which signal to neighboring cells for recruiting immune cells for the initiation of a specific adaptive immune response.
PRRs are localized in different subcellular compartments. Toll-like receptors (TLRs), C-type lectins, and scavenger receptors cover the cell surface, as well as, in the case of TLRs, membranes of the endosomal compartment. NOD-like receptors (NLRs), RIG-I like receptors (RLRs), and cyclic GMP-AMP synthase (cGAS) monitor the cytoplasm for cell damage or the presence of invasive pathogens. Activation of these receptors results in the induction or repression of type I IFNs secretion, which will be discussed in the following chapters and is summarized in Figure 1.
Detection of cytosolic DNA is mainly mediated by the ubiquitously expressed cGAS and the absent in melanoma 2 (AIM2) protein. This not only includes foreign DNA derived from pathogens, but also cytosolic chromatin resulting from genotoxic stress. While cGAS activation induces type I IFNs, detection of cytosolic DNA by AIM2 results in pyroptotic cell death as a consequence of the activation of caspase-1 and the subsequent processing and release of mature IL-1β and IL-18 [49][55]. Binding to cytosolic DNA renders cGAS in an active state, leading to the synthesis of the second messenger cyclic GMP-AMP (cGAMP) with a mixed-linkage backbone (c[G(2′,5′)pA(3′,5′)p]), which in turn is sensed by the protein referred as stimulator of interferon genes (STING) [50][51][52][53][56,57,58,59], located at the membrane of the endoplasmic reticulum [54][60]. Activation of STING leads to its translocation into the Golgi network and activates the TRAF family member associated NF-κB activator-binding kinase 1 (TBK1). After auto-phosphorylation, TBK1 subsequently activates IRF3 through direct binding [55][61]. This enables its dimerization, translocation into the nucleus, and initiation of transcription of type I IFNs. IRF3 activation results in an initial wave of transcription with IFN-β and IFN-α4 as central transcription targets. Transcription of IRF7 is also induced for allowing a positive feedback loop leading to a second wave of type I IFNs secretion [56][62]. STING is the essential mediator of this response as its deficiency abolishes cGAS-induced IRF3 activation and IFN-β induction [57][63]. cGAS deficiency in mouse bone marrow-derived macrophages (BMDMs) has been shown to be detrimental to induction of antiviral type I IFN responses towards DNA viruses such as herpes simplex virus (HSV) 1, VACV, and murine gammaherpesvirus 68, but does not influence the response towards the RNA virus Sendai virus (SeV) [58][59][64,65]. Besides activation of IRF3, STING also functions as an activator of NF-κB. For an extensive review on the functions of cGAS-STING activation, the reader is referred to [60][66].
Studies in cells from cGAS−/− mice have proven that cGAS is the main DNA sensor in antigen presenting cells, such as plasmacytoid dendritic cells (pDCs) and conventional dendritic cells (cDCs). Depletion of cGAS in those cells rendered them unresponsive towards DNA transfection and infection with DNA viruses [61][67]. The type I IFN response towards these nucleic acids is also essential as a priming signal for the function of the DNA-induced AIM2 inflammasome assembly [49][55].
Besides nucleic acids from several DNA viruses like cytomegalovirus [62][63][68,69], HSV 1 [61][67], VACV [61][67], and retroviruses [64][70], cGAS is also the sensor for microbial DNA from invasive bacteria and protozoans such as L. monocytogenes [65][66][67][71,72,73], Chlamydia trachomatis [68][74], Mycobacterium tuberculosis [69][70][71][75,76,77], Toxoplasma gondii [72][78], and Leishmania major [73][79].
The most important family of cytosolic RNA-sensors is the RIG-I-like receptor family (RLRs), consisting of the retinoic acid-inducible gene I protein (RIG-I), melanoma differentiation-associated protein 5 (MDA5), and laboratory of genetics and physiology 2 (LGP2). These proteins are able to sense the 5-prime di- and tri-phosphates of short, blunt end double stranded (ds)RNA by RIG-I, or long dsRNA by MDA5 [74][80]. All three proteins contain DExD/H box domains with ATPase function, which are crucial for RNA binding. RIG-I and MDA5 further contain two CARD. These N-terminal domains are responsible for further downstream signaling by binding to the CARD domain of the mitochondrial antiviral signaling protein (MAVS). The C-terminal domain of RIG-I serves as an inhibitory domain, keeping the protein in an inactive state until it binds RNA and conformational changes are induced [75][81].
After the binding of different cytosolic RNA species, both MDA5 and RIG-I are subject to K63-linked ubiquitination, both by covalent, and non-covalent attachment [76][82]. Either RIG-I, tripartite motif-containing protein 25 (TRIM25) [76][82], or Riplet [77][78] [83,84] can function as E3 ubiquitin ligases. This process enables RIG-I to homotetramerize [79] [85] and localize to MAVS at the outer mitochondrial membrane initiating its oligomerization [80][86]. This multimerization of MAVS results in its activation and enables recruitment of additional downstream adaptor proteins TRAF2, TRAF6, and TRADD [81][82][87,88]. Subsequently TRAF3 [83] [89] and TANK [84][90] are recruited to facilitate the activation of TBK1 and IKKε, which then phosphorylate the transcription factors IRF3 and IRF7. Activation of those two factors enables their homodimerization and translocation into the nucleus where they initiate transcription of type I and type III IFNs [85][86][87][88][91,92,93,94]. LGP2 does not contain a CARD domain, and hence was proposed not to function in signaling, but rather as a regulator of RIG-I or MDA5 function [89][95].
4. Induction of Type I Interferon Responses by Membrane Bound TLRs
While most of the members of the TLR family of TLRs may activate NF-κB signaling cascade by MyD88, type I IFNs are induced by TLRs via activation of TRIF [90][96]. Among those TLRs, TLR4 has proven to be the most important inducer of type I IFNs. Recognition of LPS, or several viral proteins, leads to the activation of TRIF. TRIF can then directly associate with TBK1, inducing IRF3 activation and translocation into the nucleus as described above [91][92][97,98]. Further, TLR3, which also signals via TRIF, and TLR7 and TLR9 are inducers of IFN responses [92][98]. TLR7 and TLR9, are mainly expressed in pDCs where they induce type I IFN expression in a MyD88-dependent manner. pDCs constitutively express IRF7, and it has been shown that MyD88 can form a complex with IRF7 to trigger its activation and transcriptional activity [93][94][99,100]. For a more comprehensive review on TLR induced immune signaling, see [95][96][101,102].
