As part of COVID-19 consequences, it has been estimated that 5% of patients affected by this dis-ease will require admission to the intensive care unit (ICU), and physical therapy techniques have been implemented in patients with other conditions admitted to ICU.
- coronavirus
- critical care rehabilitation
- intensive care units
- lung recruitment
- physiotherapy
- physical therapy modalities
- severe acute respiratory syndrome
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
1. Introduction
On 7 January 2020, the Chinese authorities identified a new virus, which was called SARS-CoV-2. It has been demonstrated that this virus can provoke various clinical symptoms, leading to a disease called COVID-19 [1]. At the date of 3 February 2021, according to the World Health Organization (WHO), there have been a total of 103,362,039 confirmed cases and 2,244,713 confirmed deaths attributed to COVID-19 [2]. Signs and symptoms of the disease can manifest as fever (98%), cough (76%), and myalgia or fatigue (44%) as the most typical; other symptoms described are sputum, headache, hemoptysis, vomiting, diarrhea, and dyspnea. In addition, many patients developed pneumonia, and one of the most typical complications was acute respiratory distress syndrome (ARDS) [3][4][5][3,4,5]. Due to its dramatic spread all over the world, many countries have been touched, leading to severe cases, deaths, and risk of healthcare and economic system collapse [6]. It is estimated that 80% of the patients will present mild symptoms (without hospital admission). The remaining 20% will need medical care, and 5% of them will require admission to the intensive care unit (ICU) [7][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42][43][44][45][46][47][48][49][4,7]; consequently, the disease can result in morbidity, disability, and mortality.
Although no criteria have been specifically developed to determine when a patient with COVID-19 must be admitted to ICU, criteria from the American Thoracic Society/Infectious Disease Society of America (ATS/IDSA) have been adopted [8][9][8,9]. As part of ICU management, some techniques and approaches are well known, such as pharmacology, hemodynamic support, or invasive mechanical ventilation, among others [10]. While there are currently no studies reporting the effect of physical therapy treatment in critically ill patients with COVID-19, it has been implemented with success in some ICUs, and effectiveness in this kind of patients has been found in some systematic reviews [11][12][11,12]. The aim of physical therapy treatment in these patients is to avoid or reduce what is known as ICU-acquired weakness [13], which has been demonstrated to be a possible risk factor of increased morbidity and mortality [14]. Thus, due to the high number of patients admitted to ICU due to COVID-19, this pandemic has created a challenge for physical therapists to apply their knowledge and skills in these patients. Therefore, it is important to summarize all the available information related to the implementation of physical therapy management in critically ill patients, so that it could be included as part of the treatment of patients admitted to the ICU suffering from COVID-19.
2. Discussion
The COVID-19 global pandemic has led to a high increase in patients admitted to ICUs. It is important to point out that physical therapists’ competences are different according to each country’s regulation, so functions will differ. In addition, health policies can also vary; thus, some of the procedures described in this review could be not recommended in some countries. Moreover, in-hospital requirements and saturation could make the implementation of these procedures difficult. During this pandemic, we have observed that acute care and ICUs have become overwhelmed in many countries. In that sense, according to a recent qualitative study performed in Spain, physical therapists have been obligated to help and develop other procedures not directly related to their profession [50], which indirectly hinders the application of these therapies [51]. Therefore, clinicians should consider deeply whether these procedures are indicated in the context of their clinical setting or could be delayed. Nonetheless, despite these objections, physical therapy treatment has been demonstrated to be effective as part of ICU management [52][11,12,52].
Thus, the aim of our review was to analyze and collect information available in the current scientific literature about physical therapy management in critically ill patients with COVID-19 or with similar respiratory conditions. The implementation of physical therapy in non-invasive mechanically ventilated patients was not considered. This is due to the high failure rate, the risk of aerosol generation, and the requirement of invasive mechanical ventilation in these patients [18]. The Italian guideline suggests a single attempt at non-invasive mechanical ventilation, with a duration of one hour [16], but this could be due to the shortage of material needed for this kind of interventions. Future publications should clarify this point.
2.1. Respiratory Physiotherapy
An interesting fact is that the Italian guideline [16] does not recommend the implementation of breathing physical therapy. In this guideline, some maneuvers such as lung-recruitment maneuvers and airway-clearance techniques are mentioned as possible techniques to implement when considered strictly needed, but to their knowledge, they argue that they are, respectively, dangerous and not frequently required in COVID-19 patients [16]. Nonetheless, breathing physical therapy is recommended in the two other guidelines [17,18]. We think that it could be explained by the risk/benefit in relation to virus infection. Possibly, in the Italian guideline, the risk of contagion considered is higher than the benefits produced by breathing physical therapy, and that is the reason why they argued that it should not be implemented. However, in the two other guidelines, they argued that this decision should be taken by the multidisciplinary team because benefits can be significant [17,18]. In fact, the Australian guideline refers us to comply with international, national state, and/or hospital guidelines for infection control, following the example of WHO guidelines [53]; nonetheless, it is necessary to consider that resources such as personal protective equipment and requirements are not inexhaustible [54], so the decision to implement physical therapy must be deeply considered, as it has been argued that the COVID-19 outbreak will cause many limitations in the rehabilitation department and other hospital facilities [55][56][55,56]. On the other hand, the implementation of inspiratory musculature training (IMT) in extubated patients can court controversy. The deterioration of ventilation parameters after mechanical ventilation has been proved [28]; however, none of the consulted guidelines proposes the implementation of IMT after mechanical ventilation, independently of the stage of rehabilitation [16–18]. The implementation of IMT in ICU patients post-extubation could be considered a little risky due to the delicate condition of the patient and the possibility of inducing changes in vital values. Nonetheless, the benefits of the activation of inspiratory muscles are significant [28–30]. The IMT must be implemented in all patients under security criteria and the approval of the multidisciplinary team. This will modify the moment of therapy implementation; nevertheless, although it can be postponed in some patients at risk, at least it should be implemented in all patients in the subacute stage because of its impact on health and the future quality of life of patients [28–30]. Another key about breathing physiotherapy is assisted postural drainage with manual techniques (percussion and vibrations). In fact, it is mentioned and indicated in the Australian guideline [18]. However, nowadays there is controversy about its efficacy; there are very few and outdated studies, and a Cochrane review from 2016 in pediatric patients discourages its use due to its inefficiency and because of the associated side effects [57]. These techniques are obsolete in current clinical practice.
2.2. Positional Treatment
In relation to the patient’s position, while the patient does not require mechanical ventilation, it is recommended to alternate positions generating a dynamic positioning. It is important to reduce at minimum the efforts to maintain the posture and to monitor oxygen saturation and perceived dyspnea [16–18]. We found that the most controversial issue is observed in intubated patients. Prone positioning for 12–16 h per day is recommended in all guidelines consulted and supported by several publications [16–18,31–35]. How to perform this maneuver and how to avoid complications due to pressure or immobility in a prone position have also been published [16,35]. However, large periods of time in a prone position could lead to difficulty to implement mobilization therapy. Interdisciplinary team cooperation and training are required to prevent complications related to rest. In patients in whom prone positioning is contraindicated, although nothing has been published about this procedure, it could be possible to consider the implementation of other positions, such as semi-prone or lateral decubitus. Medical teams could consider these options after following clinical reasoning based on security. Since changes in position can both positively and negatively modify the V/P index, individualized control of the patient must be carried out.
2.3. Mobilization and Exercise Therapy
The three guidelines make reference to the necessity of implementing mobilization therapy in ICU patients. The Italian guideline makes a light reference to passive mobilization to reduce skin lesions and immobilization sequelae, and to the necessity of discussing with the multidisciplinary team to start an early active-mobilization program [16]; the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) guideline encourages to reduce possible complications in ICU patients by early passive and active mobilization [17]; finally, the Australian guideline proposed that any patient at significant risk of developing or with evidence of significant functional limitations could be referred to physiotherapy, taking precautions to avoid contagion [18]. It is also necessary to take into account that there are some barriers to early mobilization in these subjects: patient related, structural, cultural, and process related. Thus, it is important to identify practical strategies to overcome these barriers [58].
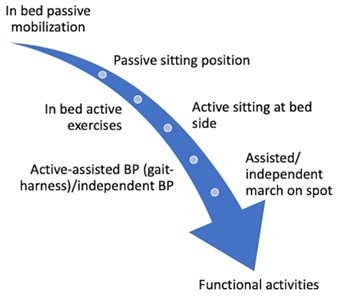
On the one hand, it has been shown that just passive mobilization can produce positive changes in the immune system [40]; on the other hand, it has been observed that active mobilization/exercise therapy can produce changes both in the short and long term [59][60][59,60]. However, we find that mobilization and exercise therapy have received less consideration than in other studies [38–49], although reported adverse events are minimum and potential benefits are high [36]. This might be due to several reasons: the saturation of ICUs, the absence of evidence of these procedures in COVID-19 patients, and/or because the risk of virus contagious is very high. Nonetheless, when protective personal equipment and other security requirements are available, we find that it would be very interesting to give more importance to these procedures, given the effectiveness that has been demonstrated [50], which could offer the possibility to reduce the length of stay in ICU survivors [61]. In addition, physical therapy management should be continued after patients are discharged from ICU to reduce ICU-acquired weakness. For this purpose, management of patients with post-intensive care symptoms should continue rehabilitation in the hospital, but intensive care follow-up programs in post-ICU clinics or at home should also be considered [62][63][62,63], as has already been done [64]; in that sense, telerehabilitation appears as a feasible option [65][66] [65,66]. That is why we developed a summary of mobilization progression based on different proposals [37,39,41,46] that can be checked in Figure 1. Nevertheless, we consider that it is very important to follow the guidelines’ recommendations about security.
Figure 1. Active exercise progression model.
This review aimed to show all the information available in relation to physical therapy management in ICU patients with COVID-19, with the intention of proportioning the most possible comprehensive review, detailing different aspects of this management. In that sense, we think this review could be used by clinicians around the world to improve their healthcare provision to critically ill patients, which could lead to reducing the length of stay and fewer complications related to intensive care.
2.4. Study Limitations
We present a theoretical guideline that is based on current scientific literature. First of all, we find important to point out that we included in our review different kinds of articles, such as clinical guidelines, that could not be assessed in terms of quality. We are conscious that it could become a limitation; nonetheless, our aim is not to assess the effectiveness, or ineffectiveness, of physical therapy procedures in critically ill patients admitted to ICU with COVID-19, and we found that clinical guidelines could offer us information not yet available in scientific sources and of interest for clinicians. Secondly, procedural details can differ from those carried out in hospitals because of system requirements and saturation. Due to the fact that not all patients are going to get benefits from these procedures, monitoring and joint decision-making by multidisciplinary teams and individualized care are required. Finally, although COVID-19 shares similarities with other respiratory conditions, we still do not know the nature of this disease, and different presentations can be found; therefore, these procedures should be implemented with caution and following a clinical reasoning process.
3. Conclusions
The implementation of physiotherapy in patients affected with COVID-19 admitted to the ICU is a necessary strategy, since it prevents complications and contributes to the stabilization of patients in critical periods, facilitating their recovery. Our review found that treatment in the ICU could be based on three main treatment modalities. At first, respiratory physiotherapy has been found to favor pulmonary ventilation, the mobilization and excretion of secretions, and the stimulation of respiratory muscles. Secondly, positional treatment has been proposed to increase the V/P index. Finally, exercise therapy could improve immune function and reduce complications, favoring functional recuperation in patients affected by COVID-19 admitted to ICU. A clinical reasoning process must be followed before implementing these procedures, and physical therapy treatment should be adapted to the context of the clinical setting.