The alteration of the physical association between the endoplasmic reticulum (ER) and mitochondria, also referred as mitochondria-associated membranes (MAMs), impacts various cellular housekeeping functions such as phospholipids-, glucose-, cholesterol-, and fatty-acid-metabolism, as well as calcium signaling, which are all altered in Alzheimer'’s disease (AD).
- endoplasmic reticulum (ER)
- mitochondria
- mitochondria-associated membranes (MAMs)
- Alzheimer’s disease (AD)
- calcium signaling
1. Introduction
Alzheimer’s disease (AD) is a neurodegenerative disease characterized by two major histological hallmarks: (1) the neurofibrillary tangles (NFTs) corresponding to intracellular aggregates of abnormally hyperphosphorylated Tau protein (pTau) and, (2) senile plaques that are mainly composed of extracellular aggregates of β amyloid peptide (Aβ) derived from the sequential cleavage of its precursor, the amyloid precursor protein (APP), by β-secretase and γ-secretase enzymes [1][2][1,2]. Late-onset AD (LOAD) cases are considered to be sporadic (SAD) accounting for the majority of AD cases. For a long time, apolipoprotein E (APOE) has been described as the sole and main genetic risk factor for LOAD forms [3]. Recently, a genome wide-association study (GWAS) identified several new AD genetic risk factors [4][5][6][4,5,6]. Dominantly inherited familial AD (FAD) accounts for less than 1% of the cases and can be caused by mutations in APP, presenilin 1 (PS1), or presenilin 2 (PS2) genes [7][8][7,8]. Overall, AD is now considered a complex pathology, the mechanistic defects of which remain unclear. The amyloid cascade is the most widely accepted hypothesis in AD and proposes Aβ accumulation as the etiological trigger of the pathology. This has been supported by genetic evidence demonstrating that FAD mutations in genes coding for APP or its processing enzymes (PS1 and PS2) constituting the catalytic components of the γ-secretase enzymatic complex [9] lead to increased production and secretion of Aβ peptides [9]. The latter accumulate in the form of neurotoxic Aβ oligomers (Aβo) and are thought to trigger several stress responses in neurons leading to the onset of neurofibrillary degeneration [9]. Several therapeutic approaches were developed with the aim to reduce the accumulation of Aβ through active and passive immunizations. However, the failure of these trials to rescue cognitive declines or even stabilize them [10] casts some doubts about the amyloid cascade hypothesis. Notably, the sole contribution of Aβ to AD pathogenesis is challenged, since APP processing yields several fragments besides Aβ [2]. In physiological conditions, 90% of mature APP is cleaved by α-secretase at the plasma membrane, producing the secreted soluble α-APP (sAPPα) and the membrane-anchored APP-C-terminal (APP-CTF)α fragment (C83). The latter is further cleaved by γ-secretase producing p3 and AICD (APP intracellular domain) peptides. On the other hand, 10% of mature APP is cleaved by β-secretase (BACE1) following its internalization towards the endosomal/lysosomal pathway, producing the soluble β-APP (sAPPβ) released in the extracellular environment, and the membrane-anchored APP-CTFβ fragment (C99), which is further cleaved by γ-secretase producing AICD and Aβ peptides [2]. C99 is also cleaved by α-secretase to produce C83 [11]. Furthermore, other APP-derived fragments produced by other enzymes (such as η- and δ- secretases) were recently described [12][13][14][12,13,14], likely contributing to AD pathophysiology [12][13][14][15][16][17][18][12,13,14,15,16,17,18].
Both the endoplasmic reticulum (ER) and mitochondria are vital organelles of the cell. Rough and smooth ER participate in protein synthesis, folding, and transport. The ER is also involved in other fundamental cellular functions such as lipids- and carbohydrates- metabolism and is the major calcium (Ca²+) storage pool [19]. On the other hand, mitochondria act as the powerhouse of the cell by generating energy through adenosine triphosphate (ATP) production [20]. Besides, mitochondria play a major role in buffering the Ca²+ flux from the ER, but also in lipid- and amino acid- metabolism, beneficial and harmful reactive oxygen species (ROS) production, and apoptosis [20]. It is now well established that ER and mitochondria functions are highly interconnected. They physically interact to form specific microdomains called mitochondria-associated ER membranes (MAMs), where the outer mitochondrial membrane (OMM) is close to the ER in the order of 10–100 nanometers [21][22][23][21,22,23]. The maintenance of stable contact sites between the ER and mitochondria provides a platform for bidirectional crosstalk. Not surprisingly, MAMs control intracellular elementary events such as Ca²+ homeostasis, metabolic flow, protein transport [24], mitochondrial lipids production, phospholipid biosynthesis, mitochondrial fusion and fission, and global events such as autophagy and apoptosis [25] (Figure 1). In addition, MAMs are a hot-spot for the transfer of stress signals from the ER to mitochondria, particularly under ER stress conditions activating the unfolded protein response (UPR) [26] (Figure 1). As a result, one can argue that the alteration of ER and mitochondria communication may influence and disrupt these functions, thus leading to the development of several pathologies and vice-versa.
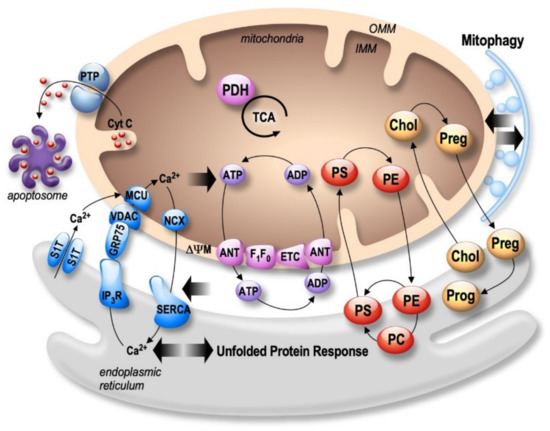
Figure 1.
2+
2+
2+
2+
2+
2+
2+
2+
+
2+
2+
3
ER stress and mitochondrial dysfunctions occur early in AD, likely contributing to disease progression and irreversible neuronal death [27][28][29][30][27,28,29,30]. Numerous papers reported that several pathogenic paradigms associated with AD are closely linked to MAMs structure and function alterations.
2. Structural and Functional Partners of MAMs Are Involved in AD
2.1. Mitofusins: MFNs
Mitofusins (MFN1 and MFN2) belongs to GTPases family and are located in the OMM. Both MFNs are involved in mitochondrial fusion process by forming homotypic and heterotypic interactions with the inner mitochondria membrane’s (IMM) OPA1 protein [31][32][31,32]. Besides, several studies proposed that MFN2 modulates mitochondrial membrane potential (ΔΨm) through the regulation of nuclear-encoded subunits of OXPHOS complexes I, II, III, and V [33]. MFN2 acts as a regulator of apoptosis in a cell type- and age-specific manner [34][35][34,35], and is linked to mitophagy [36]. The importance of MFN2 in organelles juxtaposition and the communication function of MAMs has been also proven through the regulation of mitochondria Ca2+ uptake [37]. MFN2 was also shown to be involved in dendritic outgrowth, spine formation in mice models, and to prevent neurodegeneration in the cerebellum through fusion mechanism [38].
Several studies reported that MFN2 is associated with AD [39] (Figure 2 and Table 1). MFN2 gene polymorphisms were reported in LOAD [40]. Moreover, the mitochondrial fusion and fission balance is altered in AD, correlating with enhanced or reduced MFNs expression [41]. A reduction of both MFN1 and MFN2 expression was reported in human AD brains [41][42][41,42]. Accordingly, a reduction of MFN2 expression was also reported in N2a cells expressing the APP familial Swedish mutation (APPswe) that overproduces Aβo [43]. On the contrary, an overexpression of MFN2 was observed in human cybrid cells in which mitochondria from mild cognitive impairment (MCI) subjects were incorporated into neuronal cells depleted of endogenous mitochondrial DNA [44]. These discrapencies may point out a complex regulation of MFN2 in AD pathogenesis. In fact, directly linked to APP processing in AD, MFN2 was shown to control γ-secretase activity and Aβ production by modulating ER and mitochondrial membrane contacts, without affecting BACE1 and neprilysin expression [45]. Moreover, PS2-linked FAD mutants promote ER-mitochondria coupling in a MFN2-dependent manner (Table 1) [46]. Altogether, these studies highlight a central role of MFN2 in AD pathogenesis through the regulation of MAMs tethering, mitochondrial structure and function, and cell death but also APP processing.
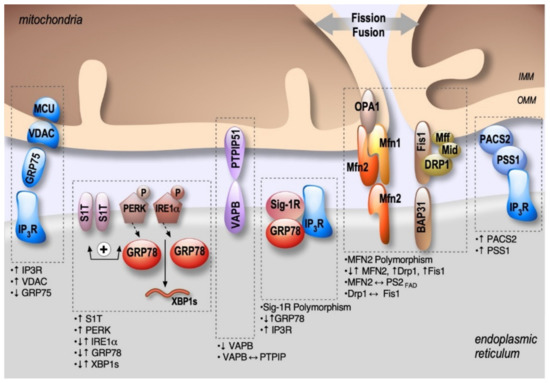
Figure 2. Schema showing the localization and alterations of MAMs molecular components in AD, including upregulation (↑) or down-regulation (↓) of MAMs proteins expression, MAMs proteins interactions (⟷), and genes polymorphism.
2.2. IP3R-Grp75-VDAC
The inositol 1,4,5-trisphosphate receptors (IP3Rs), releasing Ca2+ from the ER to the cytosol [47], are enriched in ER-mitochondria contact sites playing a key role in cellular differentiation, survival, and apoptosis [48][49][48,49]. Ca2+ uptake by mitochondria occurs through VDAC, an OMM protein which is a permeable Ca2+ channel, together with the mitochondrial Ca2+ uniporter (MCU) complex [50] located on the IMM (Figure 1). In MAMs, a functional complex between VDAC (isoform 1) and IP3R (isoform 3) is formed through a chaperone called glucose-regulated protein 75 (Grp75, a member of the heat shock protein 70 family) [51]. The IP3R-Grp75-VDAC complex regulates Ca²+ transfer from the ER to mitochondria, suggesting its involvement in Ca²+ homeostasis deregulation largely described in AD [51]. While there is only one study documenting a reduction of Grp75 expression in the temporal and parietal cortex of AD post-mortem brains [52], several studies demonstrated alterations of VDAC expression in AD (Figure 2 and Table 1). VDAC1 expression increases progressively according to AD stages in the cortex of post-mortem brains, in aged APP mice, and also in neuroblastoma cells treated with Aβo [53]. Accordingly, another study reported that Aβ treatment of primary hippocampal neurons increased VDAC1 and IP3R expression, resulting in enhanced contacts between ER and mitochondria [54]. VDAC1 also interacts with Aβ and pTau, likely contributing to mitochondrial dysfunction [55]. In turn, Aβ triggers VDAC dephosphorylation in lipid rafts in AD brains correlating with cell death [56]. Inversely, reduced expression of VDAC1 decreased the mRNA levels of APP, Tau, PS1 and PS2, and also BACE1 [57].
Altearations of IP3Rs expressions and activity have been largely explored in AD and were demonstrated to be linked to both Aβ and PS1 and PS2 FAD mutations. Fibroblasts from FAD patients exhibited an enhanced response to bombesin- and bradykinin-mediated IP3 generation in comparison to control cells [58]. These data were further confirmed in cortical and hippocampal neurons from 3xTgAD mice [59]. Aβo are also involved in IP3R overactivation by increasing IP3 production and triggering cytotoxicity [60]. Importantly, the reduction of IP3R1-mediated Ca2+ release in the cortical and hippocampal neurons of PS1M146V and 3xTgAD mice reduces ryanodine receptor (RyR)-mediated Ca2+ release, restores cAMP response element-binding (CREB)-dependent gene expression, rescues long-term potentiation (LTP) to normal levels, attenuates Aβ accumulation and pTau and reverses memory deficits [61]. Another study also showed a physical interaction of IP3R with PS1 (M146L) and PS2 (N141I) mutants stimulating IP3R gating activity [62] (Figure 2 and Table 1). Of note, our laboratory and others reported a major role of enhanced RyR expression and activity in AD [63][64][65][66][67][68][63,64,65,66,67,68]. Nevertheless, dedicated studies are still needed to demonstrate if the interaction between IP3R and FAD PSs mutants occurs preferentially in MAMs and to unravel the physiopathological contribution of RyRs in MAMs dysfunction related to AD.
2.3. PACS2-PSS1
Phosphofurin acidic cluster sorting protein 2 (PACS2) is a multifunctional sorting protein that interacts with several cargo proteins and regulates their location in MAMs [69]. PACS2 controls apoptosis induction, through the translocation of Bim (Bcl-2-like protein 11) to lysosomes [70], or Bid (BH3 interacting domain) to mitochondria [71]. The precise localization of PACS2 in MAMs is still uncertain. However, it has been demonstrated that PACS2 controls ER-mitochondrial apposition through its tethering action and is also involved in Ca2+ transfer from ER to mitochondria through IP3R localization [71]. Accordingly, PACS2 deletion leads to decreased ER-mitochondria contacts and triggers mitochondria fragmentation [71] and apoptosis [72].
PSS1 (phosphatidylserine synthase-1) is synthesized and specifically located in MAMs, supporting the direct transfer of lipids between ER and mitochondria [73]. PACS2 and PSS1 are functionally linked, since the overexpression of PACS2 raises the levels of PSS1 in MAMs [71].
PACS2 and PSS1 regulations in AD were reported in a study by Hedskog et al. showing enhanced PACS2 and PSS1 protein levels in AD transgenic mice expressing Swe/LDN FAD mutations [54]. More precisely, PACS2 protein expression was enhanced in the hippocampus of 2 month-old aged mice before Aβ plaque formation, and in the cortex and the cerebellum at 6 months. Meanwhile, PSS1 protein expression was only enhanced in the cerebellum starting at 6 months. Importantly, the authors also revealed enhanced PSS1 and PACS2 protein levels in human SAD brains (Figure 2 and Table 1). Enhanced PSS1 and PACS2 protein expressions were not corroborated by an increase in PSS1 and PACS2 mRNAs levels, suggesting that the regulation of PSS1 and PACS2 expressions in AD occurs at the protein level only. The authors also reported unchanged phospholipid metabolism in both mice and AD brains, thus questioning the functional consequences related to enhanced PSS1 and PACS-2 protein expression. Nevertheless, ablation of PSS2 triggers degeneration of astrocytes and neuronal hippocampal primary cultures. In conclusion, this unique study unravels the potential contribution of an additional MAMs molecular component in AD [54].
2.4. BAP31-FIS1-DRP1
Another physical tether of MAMs has been described as the interaction between the resident integral ER protein B cell receptor–associated protein 31 (BAP31) and the OMM mitochondrial FIS1 protein involved in the initiation of mitochondrial fission process [74][75][74,75]. FIS1 interacts with dynamin-related protein1 (DRP1) after its recruitment at mitochondrial fission sites by the OMM receptors (Mff, Mid49 and Mid51) in the MAMs complex, including BAP31 [76]. Intriguingly, a recent study reported that the human FIS1 protein can cause mitochondrial fragmentation in the absence of DRP1 and Dyn2 GTPases through its ability to bind to MFN1, MFN2, and OPA1, also inhibiting the mitochondrial fusion [77]. Shen et al. also demonstrated that mutations in the FIS1 gene do not cause defects in mitochondrial fission in response to fission-inductor chemical treatments but trigger persisting large aggregates of autophagosomes [76]. Accordingly, FIS1 KO MEFs cells display a strongly impaired mitophagy [78]. Iwasawa et al. showed that FIS1 conveys an apoptosis signal from the mitochondria to the ER through its interaction with BAP31 at the ER and its cleavage into the pro-apoptotic p20 [74]. The latter triggers a Ca2+ transfer from the ER to the mitochondria leading to ΔΨm depolarization, hence priming cell death induction [74][75][74,75]. BAP31 is also essential for mitochondrial homeostasis as it stimulates the formation of the mitochondrial complex I [79].
Several studies reported that FIS1, BAP31, and DRP1 may contribute individually to AD physiopathology (Figure 2 and Table 1). It was first reported that the mRNA and protein levels of FIS1 and DRP1 are increased in the frontal cortex of patients with early, definite, and severe AD [42]. Joshi et al., reported later that Aβ42-treated neurons and fibroblasts from SAD or FAD patients feature an increased interaction between DRP1 and FIS1, which causes mitochondrial dysfunctions attested by increased mitochondrial fragmentation, oxidative stress, decreased ΔΨm and ATP levels, and increases in the activity of pro-apoptotic enzymes and Cyt c release [80]. Most importantly, inhibiting the DRP1-FIS1 interaction corrects these mitochondrial impairments, reduces in the 5xFAD mice AD model (that overexpress human APP and PS1 transgenes with a total of five AD-linked mutations) cognitive defects, Aβ40 and Aβ42 levels, and oxidative stress, and increases ATP levels [80]. In parallel, BAP31 knockdown in the hippocampus and the cerebral cortex of PS1 M146V mice results in an increased BACE1 protein level, exacerbating C99 accumulation and Aβ plaque formation [81]. Other studies showed that pTau and Aβ monomers and oligomers can also directly interact with Drp1 in AD late stages, likely contributing to abnormal mitochondrial dynamics [42][82][42,82]. Moreover, Aβ also triggers nitric oxide production, likely contributing to Drp1 S-nitrosylation-mediated mitochondrial fragmentation and neuronal damage [83] (Figure 2 and Table 1). Together, these studies support the involvement of the BAP31-FIS1-DRP1 complex in AD pathology.
2.5. VAPB-PTPIP51
The OMM protein, tyrosine phosphatase-interacting protein-51 (PTPIP51), was identified as a binding partner for the resident ER protein vesicle-associated membrane protein-associated protein-B (VAPB) [84]. As a physical tether of MAMs, VAPB has several functions, including vesicle trafficking and UPR [84]. It was then demonstrated that the loss of either VAPB or PTPIP51 perturbs the uptake of Ca2+ by mitochondria, decreasing ATP production [85] and stimulating the formation of autophagosomes [86]. Additionally, PTPIP51 can interact with the oxysterol-binding protein (OSBP)-related proteins ORP5 and ORP8 in MAMs [87], likely contributing to phosphatidylserine (PS) transport between ER and mitochondria.
VAPB P56S mutation is associated with dominantly inherited familial forms of type-8 amyotrophic lateral sclerosis (ALS) [88]. Moreover, TAR DNA binding protein 43 (TDP-43) and fused in sarcoma (FUS), two ALS/frontotemporal dementia (FTD)-associated proteins, were reported to activate the glycogen synthase kinase-3β (GSK-3β), which inhibits VAPB-PTPIP51 binding, ultimately resulting in disrupted Ca2+ homeostasis and reduced ATP production [85][89][85,89]. Strikingly, it has recently been observed that AD patients with granulovacuolar degeneration bodies (GVB) feature lower VAPB level [90] (Figure 2 and Table 1). Interestingly, AD is a pathology where TDP-43 and FUS accumulate in stress granules and GVB. Furthermore, GSK-3β is also overactivated in AD [91]. A recent study reports a reduction of VAPB and PTPIP51 interaction in the pyramidal cortex of patients with early/mid dementia, and a reduction of the expression of both VAPB and PTPIP51 in the cortex of AD patients at late-stages [92]. Together, these studies also suggest the involvement of VAPB-PTPIP51 physical/or functional alterations in AD pathophysiology.
2.6. Sig-1R-Grp78
Sigma non-opioid intracellular 1-receptor 1 (Sig-1R) is a chaperone protein present in ER lipid rafts that interacts and modulates different proteins in ER and plasma membrane [93]. Sig-1R is essential for MAMs stability [94], and is implicated in lipid synthesis and trafficking [95].
Grp78 (or BiP), a member of the heat shock protein 70 family, is a chaperone and an ER stress sensor [96]. Importantly, Grp78 is present in MAMs, where it folds the steroidogenic acute regulatory protein (StAR) transporting cholesterol for delivery to the OMM [97]. Under ER stress conditions, Grp78 dissociates from and activates three branches of the UPR: activating transcription factor 6 (ATF6), IRE1α, and PERK. The UPR generates an adaptive or a pro-apoptotic response according to the stress duration and/or intensity [98]. In aging, the pro-apoptotic response becomes more common than the adaptive pathway, probably due to a failure in chaperone systems [98]. Interestingly, the impairment in UPR, apoptosis, and accumulation of misfolded proteins are common features of AD and other neurodegenerative diseases [99]. Desipte this, there is still no consensus on the role of Grp78 in AD. While APP/PS1 mice and Aβ25-35 treated neurons presented increased Grp78 expression (reviewed in Reference [100]), another study in AD post-mortem brains with PS1 mutations showed a reduction in Grp78 mRNA levels [101]. Recently, a study demonstrated that the 5xFAD mice had no changes in Grp78 expression and other ER stress-related proteins [102]. These discrepancies could be linked to the pleiotropic functions regulated by and regulating Grp78 expression (Figure 2 and Table 1).
Sig-1R forms a complex with Grp78 in MAMs under resting conditions [103]. During ER stress, Sig-1R also dissociates from Grp78 and forms a complex with IP3R through ankyrin B to increase Ca2+ signaling from ER to the mitochondria, thereby enhancing ATP synthesis [104]. Besides, Sig-1R stimulates phospholipase C (PLC) that increases IP3 levels, resulting also in Ca2+ release from the ER [105]. The activation of Sig-1R is considered neuroprotective since Sig-1R silencing in hippocampal neurons results in Cyt c release, caspase-3 activation, and a deficit in spine formation. Remarkably, this mechanism is reversed by superoxide dismutase activation, showing that the reduction of Sig-1R increases the levels of ROS [106].
Interestingly, Sig-1R has been associated with a variety of neurodegenerative diseases, including AD [107][108][107,108]. Reduced Sig-1R binding sites were reported in AD post-mortem brains [109]. It has also been proposed that a polymorphism in Sig-1R (TT-P) correlates with the risk of developing AD [110]. This finding has been challenged in another study demonstrating that another Sig-1R polymorphism (Q2P) may worsen clinical outcomes only in association with the gentic risk factor APOEε(epsilon)4 [111]. The protective effect of Sig-1R has also been observed in two AD mice models (3xTg-AD and MacGill-R-Thy1-APP), where the treatment with a Sig-1R agonist, named AF710B (a concomitant agonist of the muscarinic 1 receptor), have been shown to restore cognitive impairment, and to reduce amyloid pathology and neuroinflammation [112][113][112,113]. Accordingly, the silencing of Sig-1R or application of the Sig-1R antagonist (NE-100) aggravated the pathological status in Aβ25-35 treated mice (i.e., learning deficits, reduced BDNF levels, and enhanced expression of Bax) [114]. The treatment of Aβ25-35 injected mice with ANAVEX2-73, another agonist of Sig-1R, decreases pTau, Bax/Bcl-2 ratio, lipid peroxidation, C99 accumulation, and Cyt c release [115][116][115,116], while decreasing Sig-1R expression enhances Tau hyperphosphorylation and reduces dendritic spines formation [117].
Overall, these studies converge to demonstrate the neuroprotective effect of Sig-1R agonists, acting through a diversity of Sig-1R-mediated signaling functions that are generally pro-survival and anti-apoptotic.
2.7. Protein Kinase-Like Endoplasmic Reticulum Kinase: PERK
Several studies reported that the activation of the PERK pathway attenuates protein synthesis until the unfolded protein accumulation is removed [98]. Interestingly, PERK is enriched at MAMs [118], where it facilitates the tethering of the ER to mitochondria and sensitizes cells to apoptosis [118][119][118,119]. PERK KO cells show reduced MAMs and disturbed cytosolic Ca2+ signaling and also protect cells from ROS-induced mitochondrial dysfunction [118]. A recent study demonstrates that PERK localized in MAMs phosphorylates mitochondrial E3 ubiquitin ligases and decreases the formation of mitochondria-associated ER membranes under ER stress condition [120]. UPR occurs relatively early in AD, and PERK was shown to be activated in human AD-derived brains [121][122][121,122]. The dysregulated PERK pathway has been recapitulated in AD mice models that develop β-amyloidosis [123][124][125][123,124,125], Tau-mediated neurodegeneration [126][127][126,127], and in SAD genetic risk factor APOEε4 mice models [128] (Figure 2 and Table 1). Several studies have provided mechanistic insights into the direct relationship between PERK overactivation and several paradigms occurring in AD. The phosphorylation of eIF2α, occurring down-stream of PERK activation, has been shown to increase BACE1 expression, thereby enhancing the production of Aβ in neurons [129], and genetic reduction of PERK reduces BACE1 protein level and Aβ production in the 5xFAD mouse model [123]. Accordingly, the selective ablation of PERK improved the synaptic plasticity and spatial memory in mice harboring APP and PS1 mutations [124], consistent with the requirement for active protein translation in memory consolidation [130]. Another study demonstrated that a reduction in eIF2α phosphorylation enhances the late phase of LTP and memory in mice [131]. Furthermore, the local expression of ATF4 (a transcription factor activated downstream of PERK and eIF2α ER stress responsive pathway) in axons induces axonal damage through a cell-non-autonomous mechanism that propagates between neurons [132]. These data suggest that sustained PERK-eIF2α-ATF4 activation worsens AD pathogenesis, and that PERK localization in MAMs may act as a new pathogenic route contributing to AD development.
Table 1. MAMs molecular component alterations in AD. These alterations include reduced (↓), increased (↑), unchanged expressions (=), or interaction (⟷) between proteins observed in AD study models and human-derived samples (SAD brains and SAD/ FAD fibroblasts); KO: knock-out; KI: knock-in; “OE”: overexpressing; MCI: mild cognitive impairment; GVB: granulovacuolar degeneration bodies; Aβo: Aβ oligomers.
Proteins | Alterations | Study Models | References | |||||||||||||
MFNs | Polymorphism | AD patients |
[40] |
|||||||||||||
| ↓MFN2 & MFN1 (proteins and mRNA) | AD brains (hippocampus & frontal cortex) & N2a “OE” APPswe |
[41–43] |
|||||||||||||
| ↑MFN2 | MCI cytoplasmic hybrid (cybrid) cells |
[44] |
|||||||||||||
| ↑MFN2⟷PS2 (FAD), ↑MAMs | MFN2 KO MEFs | FAD PS2 (N141I) Mice |
[46] |
||||||||||||
IP3R-Grp75-VDAC | ↑VDAC | Aβ⟷VDAC | pTau⟷VDAC | Tg2576 and J20 mice | APP, APP/PS1, 3xTgAD mice & AD brains (cortical tissues) |
[53] [55] |
||||||||||
| ↑VDAC, ↑IP3R activity, ↑MAMs | Ab-treated hippocampal neurons |
[54] |
|||||||||||||
| VDAC dephosphorylation | AD brains |
[56] |
|||||||||||||
| ↓Grp75 | AD brains (temporal and parietal cortex) |
[52] |
|||||||||||||
| FAD PS1/2⟷IP3R | Sf9 cells |
[62] |
|||||||||||||
PACS2-PSS1 | ↑PACS2, | ↑PSS1 | APPswe/LDN mice | AD brains cortex |
[54] |
|||||||||||
BAP31-FIS1-DRP1 | ↑Fis1, ↑Drp1 | AD brains (frontal cortex) |
[42] |
|||||||||||||
| ↑Drp1⟷Fis | Aβ42-treated neurons, SAD/FAD fibroblasts, N2a “OE” APPswe, & 5xTgAD mice |
[80] |
|||||||||||||
| pTau⟷Drp1 | ↓Drp1 mito localization | AD brains, APP, APP/PS1 & 3xTgAD mice | Drosophila “OE” Tau R406W |
[55] [133] |
|||||||||||
| Ab⟷Drp1 | AD brains (frontal cortex) |
[42] |
|||||||||||||
VAPB-PTPIP51 | ↓VAPB, ↓PTPIP51 | ↓VAPB⟷PTPIP51 | AD brains (subicular with GVB neurons) | AD brains (cortex) |
[90] [92] |
|||||||||||
Sig-1R-Grp78 | ↓Sig-1R | Sig-1R polymorphism | AD brains | AD patients |
[109] |
[109] [110,111] |
||||||||||
| ↑Grp78 | Streptozotocin model, APP/PS1 mice & Aβ25-35-treated rats |
[134–136] |
| ||||||||||||
| ↓Grp78 mRNA | AD brains (FAD PS1) |
[101] |
|||||||||||||
| =Grp78 expression | 5xFAD mice |
[102] |
|||||||||||||
PERK | ↑PERK pathway | AD brains | 5xFAD mice | APP/PS1, APP(SL)/PS1 KI & rTg4510 mice | APOE4 mice |
[121][122][123][124][125][126] [123] |
[121–126] [123] [124–127] [128,129] |
|||||||||
IRE1a | ↑↓IRE1a pathway, ↑↓XBP1s | AD brains & 5xFAD mice | Aβ 42o-treated SH-SY5Y & CHO “OE” APPLDN |
[137] [138] |
||||||||||||
S1T | ↑S1T |
| AD brains, SHSY-5Y “OE”APPswe or treated with Aβo |
[139] |
|
2.8. Active Inositol-Requiring Transmembrane Kinase and Endonuclease Alpha: IRE1α
The UPR IRE1α branch increases protein folding trough the induction of chaperones and enhances the removal of misfolded proteins [98]. Active IRE1α processes the mRNA encoding X-box-binding protein 1 spliced isoform (XBP1s), a transcription factor that upregulates genes encoding mediators of protein folding, ERAD (ER-associated degradation), organelle biogenesis, and protein quality control [98]. A fraction of IRE1α is located at MAMs through Sig-1R stabilization responding to mitochondrial ROS [103][140][103,140]. A recent study demonstrated that the mitochondrial ubiquitin ligase (MITOL/MARCH5) inhibits ER stress-induced apoptosis through ubiquitylation and degradation of IRE1α at MAMs [141]. IRE1α at MAMs can also induce cell death via mitochondrial Ca2+ overload [142]. Another study linked IRE1α to mitochondrial dysfunction and apoptosis through the phosphorylation of ASK1 and JNK [143][144][143,144].
The activation of the IRE1α branch is implicated in AD pathogenesis, mainly through the activation of XBP1s [121][122][121,122] (Figure 2 and Table 1). Enhanced or reduced XBP1 mRNA splicing was reported in AD human brains [145]. XBP1s activation occurs upon Aβo treatment lowering BACE1 protein level [138] and activating Kalirin-7 (Kal7), a protein that controls synaptic plasticity [146]. This suggest that XBP1s acts as a protective mechanism in AD. Accordingly, the overexpression of XBP1s protects against Aβ toxicity [147] and pathological Tau [148]. In addition, a genomic screen identified a cluster of AD genes as possible direct targets of XBP1s, including APP, and components of the α-secretase, and proteins involved in APP trafficking and maturation [149]. Finally, in both Drosophila and mammalian cell culture models of AD, XBP1 overexpression also down-regulates RyR3 expression, which in turn prevents cytosolic Ca2+ overload [147]. These last data corroborate studies demonstrating that pharmacological and genetic approaches reducing RyR-mediated exacerbated ER Ca2+ leak provide protective effects and rescue several AD pathogenic paradigms in cellular and mice AD models [64][65][66][64,65,66].
2.9. The Truncated Variant of the Sarco-Endoplasmic Reticulum Ca2+-ATPase 1: S1T
S1T is among molecular partners at the ER-mitochondria interface regulating inter-organelle Ca2+ signaling and cell death [150][151][152][150,151,152]. We reported the induction of S1T expression under pathological ER stress conditions occurring through the PERK-eIF2α-ATF4-CHOP (C/EBP homologous protein) pathway. On the one hand, S1T induction amplifies ER stress response, and on the other hand, it enhances ER Ca2+ leak, increases the number of ER-mitochondria contact sites, and inhibits mitochondrial movements. This leads to increased Ca2+ transfer to mitochondria, thus activating the mitochondrial apoptotic pathway [152]. Interestingly, we recently reported a molecular interplay between S1T-dependent ER Ca2+ leak, UPR, and APP processing, likely contributing to AD pathogenesis [139] (Figure 2 and Table 1). We demonstrated that S1T expression is increased in SAD brains and correlates with Aβ and ER stress chaperone protein levels (Grp78 and Calreticulin). Increased S1T expression is induced in an Aβ-dependent manner and enhances in return the production of APP-CTFs and Aβ through specific increases of BACE1 expression and activity. Interestingly, the induction of S1T expression is also linked to neuroinflammation [139]. Other studies are ongoing to unravel the contribution of S1T-mediated ER Ca2+ leak to MAMs dysfunctions, synaptic plasticity alterations, and cognitive deficits in AD.
