Quercetin (QRC) is a flavonoid belonging to a group of plant-derived nonsteroidal compounds called phytoestrogens. It is a polyphenol-based molecule and it is widely distributed in many vegetables, fruits, seed, grains, and also in tea and wine.
- Quercetin
- antibacterial effect
- nanocomposite
- tissue regeneration
- natural compound
- polyphenol
1. The Antibacterial Effect of Quercetin
Oral bacterial infections are strongly associated with the most common oral diseases, such as periodontitis and gingivitis. The kinds of bacteria involved are both Gram-positive, including Streptococcus and Actinomyces, and Gram-negative (Figure 2) [1]. On the one hand, the increase in bacterial number is related to a reduction of innate and adaptative immunity; on the other hand, the growth of drug-resistant bacterial strains makes the treatment of these diseases a challenge. In light of this, the usage of flavonoids, such as QRC, has been proposed as an alternative to common antibacterial treatments [2].
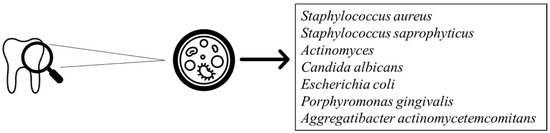
Figure 2. Bacterial strains involved in periodontal disease.
Some studies have investigated the role of flavonoids in the management of dental plaque bacterial infection. Notably, Gutierrez-Venegas et al. have demonstrated that QRC and other flavonoids possessed bacteriostatic activity on almost all microorganisms affecting the oral cavity, including Candida albicans. The latter is well known to cause candidiasis, which could manifest in different clinical forms and involves one or more mouth sites [3].
The properties of some microorganism to produce biofilm as well as the drug resistance are contemplated as global public health problems. In particular, biofilm promotes the growth of microorganisms, protecting them from the surrounding environment, acting as an important factor of virulence, and increasing bacterial resistance to antibiotics and the host’s immune system [4]. In a study proposed by Dias da Costa Júnior et al., the antibacterial and antibiofilm activity of QRC against Staphylococcus aureus and Staphylococcus saprophyticus, both vancomycin and methicillin resistant, was evaluated. QRC displayed the MIC values, ranging between 250 to 1000 µg/mL and 62.5 to 1000 µg/mL for Staphylococcus aureus and Staphylococcus saprophyticus, respectively. The best inhibitory effect of QRC was observed against the methicillin-sensitive Staphylococcus aureus (MSSA), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-intermediate Staphylococcus aureus (VISA) strains (MIC = 250, 500 and 125 µg/mL, respectively), while the lowest inhibitory effect was against the vancomycin-resistant Staphylococcus aureus (VRSA) strain (MIC = 1000 µg/mL). Regarding the antibiofilm activity, QRC was able to reduce 50% of the biofilm production, even when it was analysed in sub inhibitory concentrations [5].
An antibacterial mechanism of QRC has been proposed by Wang et al. Firstly, in this study they found that the MICs of QRC for Escherichia coli and Staphylococcus aureus were 0.0082 and 0.0068 µmol/mL, respectively. After that, both bacterial strains were treated with concentrations of QRC up to 500-fold higher than their respective MICs for 24 h and then analysed by transmission electron microscopy (TEM) and in term of alkaline phosphatase (ALP) extracellular activity, to investigate the morphology and the permeability of the bacteria. The TEM images displayed that the cell wall and membrane were already damaged using concentrations 50-fold higher than the MIC for Escherichia coli, and 10-fold higher for Staphylococcus aureus. At the same conditions, the researchers found that the ALP activity in Staphylococcus aureus was significantly higher than Escherichia coli, confirming the previous results. In conclusion, according to this study, the bacteriostatic effect of QRC is greater for Gram-positive than Gram-negative bacteria, probably related to the difference in peptidoglycan concentration in the cell wall [6].
Since Porphyromonas gingivalis (Pg) and Aggregatibacter actinomycetemcomitans (Aa) are both strongly associated with the onset of periodontitis, Geoghegan et al. have studied the effect of QRC against these bacteria. Both the in vitro cultures of these periodontal pathogens were treated with an aqueous QRC solution of 0.1, 0.05, and 0.025 g/mL, using chlorhexidine and sodium chloride as a positive and negative control, respectively. All the results were carried out after 1, 3, 6, and 24 h of incubation. They found that QRC was able to reduce significantly the growth of Pg at 1 h and no difference with the positive control after 6 h was detected, while the growth of Aa was inhibited in a time-dependent manner when compared with the negative control. Finally, in another study they showed that QRC possesses an antibacterial activity of 0.0125 g/mL and 0.1 g/mL MIC for Pg and Aa, respectively [7].
2. Effect of Quercetin on Bone Tissue Regeneration
Phytoestrogens are plant-derived dietary chemicals found in a lot of vegetables and fruits consisting of isoflavonoids, lignans, stilbenes, and the flavonoid QRC
[8]
. Some studies have displayed their role in prevention and treatment of cardiovascular diseases, osteoporosis, diabetes, obesity, and menopausal symptoms
. They are chemically characterized by structural similarity to 17-β-oestradiol (E2), which enables them to modulate the osteogenic mechanism by interaction with ERa and ERb, subtypes of the oestrogen receptors (ERs), both present on the surface of osteoblasts cells
[11]
. The effect of QRC on osteogenesis has been confirmed by several studies
and it is considered the most potent osteogenic chemical ever discovered, although the real mechanism involved is still unclear.
Pang et al. have investigated the effect of QRC in the proliferation and osteoblastic differentiation on the in vitro cultures of mice-derived bone marrow mesenchymal stem cells (BMSCs). The latter are multipotent stromal cells able to differentiate into various cell types, including the osteoblasts, and therefore play an important role in the induction of osteogenesis [14]. After treatment with increasing concentrations of QRC (0.1 μM–5 μM), they observed a significant rise in BMSC proliferation and ALP activity, which meant an enhanced osteoblast formation in a dose-dependent manner. They also displayed that QRC stimulated osteogenic differentiation, interacting with the oestrogen-signalling pathway, which led to the up-regulation of the osteogenic genes runt-related transcription factor 2 (RUNX2) and Osterix (OXS) [15].
The stimulatory effect of QRC on ALP activity was evaluated by Prouillet et al. In one study, they worked on human osteoblastic cell MG-63 incubated with QRC at 1, 10, and 50 μM for 24 and 48 h in Dulbecco’s modified eagle medium (DMEM), observing that QRC was able to rapidly increase the ALP activity in time and dose-dependent manners. They also found that the extracellular signal-regulated kinase (ERK) pathway was involved in the mechanism, highlighted by the reduction in QRC’s effect when the cells were treated with the MEK inhibitor PD 98059. They evidenced that ICI 182780, an antagonist of the oestrogen receptors (ERs), was also able to reduce the quercetin-mediated ALP activity, confirming the role of these receptors in the phenomenon [16].
Since is well known that the mitogen-activated protein kinase (MAPK) pathway was involved in the osteogenic differentiation of mesenchymal stem cells (MSCs), Li et al. have evaluated the role of QRC in this phenomenon. The MCSs obtained by mice were treated with QRC at 0.01, 0.1, 1, 10, and 100 μM for 72 h. After incubation, the authors found that QRC stimulated the ALP activity in a dose-dependent manner and increased the levels of osteocalcin (BGP) and type 1 collagen (COL I), two bone marker proteins. Moreover, the MAPK and ERK pathways were also stimulated by the treatment with QRC; these results were confirmed, incubating the cells simultaneously with QRC and antagonists of these pathways. The authors highlighted that all the above-mentioned markers were downregulated, confirming the role of QRC in the osteogenesis of MAPK [17].
QRC seems to influence also the osteoclastogenesis phenomenon. In a study carried out by Wattel et al., the in vitro role of QRC on osteoclastic differentiation was evaluated using two major models of osteoclastic-like cells, RAW 264.7 and PBMC, treated with various concentrations of this flavonoid up to 10 μM. They found that QRC showed a strong inhibitory effect in osteoclast differentiation at concentrations as low as 1 μM. Their investigations highlighted that QRC inhibits two transcription factors, the nuclear factor kappa-light-chain-enhancer of activated B cells (NFkB) and the activator protein 1 (AP-1), which are well known to modulate the differentiation and proliferation of osteoclasts [18].
A summary of QRC’s antibacterial activity and bone tissue regeneration properties is provided in Table 1.
Table 1. Summary of in vitro QRC antibacterial activity and bone tissue regeneration properties.
| Antibacterial Activity | QRC Concentration | Cell Type | MIC | Markers | Findings | References |
|---|---|---|---|---|---|---|
| From 250 to 1000 µg/mL | Staphylococcus aureus; Staphylococcus saprophyticus | Staphylococcus aureus MIC = 62.5 µg/mL; Staphylococcus saprophyticus MIC = 1000 µg/mL; | 50% reduction of biofilm formation for each bacterium | Dias da Costa Júnior et al. 2018 [5] | ||
| Up to 500 times higher the MICs | Escherichia coli; Staphylococcus aureus | Escherichia coli MIC = 0.0082 µmol/mL; Staphylococcus aureus MIC = 0.0068 µmol/ml | Cell wall and membrane damaged at concentration of 50-fold and 10-fold higher than the E. coli and S. aureus MICs, respectively. | Wang et al. 2018 [6] | ||
| 0.1, 0.05, 0.025 g/mL | Porphyromonas gingivalis; Aggregatibacter actinomycetemcomitans | Porphyromonas gingivalis MIC = 0.0125 g/mL; Aggregatibacter actinomycetemcomitans MIC = 0.1 g/mL | Reduction of bacteria’s growth in time-dependant manner | Geoghegan et al. 2010 [7] | ||
| Osteoprotective Activity | ||||||
| From 0.1 μM to 5 μM | BMSCs | ALP; RUNX2; OXS | Increase of cells proliferation and up regulation of osteogenic genes. | Pang et al. 2018 [15] | ||
| 1, 10 and 50 μM | MG-63 | ALP; ERK Pathway; ERs | Increase of ALP activity, related to ERK and ERs pathways. | Prouillet et al. 2004 [16] | ||
| 0.01, 0.1, 1, 10 and 100 μM | MSCs | ALP, BGP, COL I; MAPK and ERK pathways | Increase of ALP activity and BGP and COL I levels. Increase of ERK and MAPK. | Li et al. 2015 [17] | ||
| Increasing up to 10 μM | RAW 264.7 and PBMC | NFkB; AP-1 | Strong inhibition of osteoclast proliferation and differentiation. | Wattel et al. 2004 [18] |
ALP: alkaline phosphatase; RUNX2: runt-related transcription factor 2; OXS: Osterix; ERK: extracellular signal-regulated ki
e phosphatase; RUNX2: runt-related transcription factor 2; OXS: Osterix; ERK: extracellular signal-regulated kinases; ER: oestrogen receptor; BGP: osteocalcin; COL I: collagen type 1; MAPK: mitogen-activated protein kinase; NFkB: nuclear factor kappa-light-chain-enhancer of activated B cells; AP-1: activator protein 1.
nases; ER: oestrogen receptor; BGP: osteocalcin; COL I: collagen type 1; MAPK: mitogen-activated protein kinase; NFkB: nuclear factor kappa-light-chain-enhancer of activated B cells; AP-1: activator protein 1.
3. Dentistry Application
In the last years, some studies have highlighted the effects of QRC in oral and dentistry applications. Researchers have
3. Dentistry Application
demonstrated that both the osteogenesis and anti-inflammatory properties of QRC could be used to manage the dental restoration and periodontitis.
In the last years, some studies have highlighted the effects of QRC in oral and dentistry applications. Researchers have demonstrated that both the osteogenesis and anti-inflammatory properties of QRC could be used to manage the dental restoration and periodontitis.
Since the stimulation of dentinogenic differentiation could accelerate pulp reparation after pulp-capping treatment, Kim et al. have investigated the role of QRC, genistein, and baicalin in this phenomenon in terms of ALP activity, dentin sialophosphoprotein (DSPP) mRNA expression, and mineral deposition. Increasing concentrations from 1 to 25 μM of QRC and other chemicals were tested on human dental pulp cells (HDP) culture that had been isolated from orthodontic patients’ incisors. Among all, QRC showed the highest ALP activity and DSPP mRNA expression. As the latter is an odontoblastic-specific protein, this result suggested a dentinogenic activity of QRC. Therefore, they also found that the cells treated with QRC displayed an increasing mineral deposition in a dose-dependent manner. Finally, the quercetin-related ERs and ERK signalling pathway have been hypothesized as having a role in dentinogenesis, but the results have not confirmed it yet [19].
The role of QRC as a remineralization agent on root caries treatment was evaluated by Epasinghe et al. For this purpose, demineralized root fragments obtained from human third molars were treated with a solution of 6.5% w/v QRC in phosphate buffer for 10 min. In the same way, a sodium fluoride solution and deionized water were used as the positive and negative control, respectively. All samples were treated cyclically six times per day with QRC solutions, an acidic buffer, and a neutral buffer for 8 days. Remineralization was assessed by transverse microradiography and confocal laser scanning microscopy. According to the results, QRC was able to inhibit the demineralization. Therefore, it promoted the remineralization of root caries lesions more than the negative control, although fluoride remained the most effective [20].
A reduction in the dentin-adhesive bond strength could lead to failure of the dental restoration due to the increasing metalloproteinases (MMPs) activity and acidogenic bacteria proliferation, such as Streptococcus mutans. A composite dental adhesive doped with QRC at various concentrations was developed by Yang et al. and evaluated in vitro and in situ. They found that the quercetin-based composite reduced both Streptococcus mutans biofilm growth and metabolic activity in a dose-dependent manner up to a QRC concentration of 1000 µg/mL. The composite was characterized in terms of microtensile bond strength, nano leakage expression, and MMPs activity by in situ analysis on caries-free human third molar specimens. The results highlighted that QRC exhibited no influence on the immediate bond strength at a range concentration of 100 to 500 µg/mL. Therefore, both nano leakage expression and MMPs activity decreased with the rising concentration of QRC. The overall results suggested that the adhesive loaded with QRC was more efficient than the empty one to preserve the degradation of the adhesive–dentin interface [21].
Napimoga et al. have evaluated the role of QRC on a mouse periodontitis model infected with Aggregatibacter actinomycetemcomitans. After three days of bacterial inoculation, to induce the periodontitis, the mice were treated with a QRC daily dose of 100 mg/kg, for 15 days, by subcutaneous injection. Then, on the sacrificed animals, the morphometric analysis highlighted that QRC reduced the alveolar bone resorption while it did not affect the viability of the bacteria colonies. An immunohistochemical assay conducted on gingival tissue has shown that QRC negatively modulated the production of pro-inflammatory cytokines, such as the interleukin-1β (IL-1β), tumour necrosis factor-α (TNF-α), and interleukin-17 (IL-17). Moreover, QRC downregulated the intercellular adhesion molecules I-CAM and osteoclastogenic receptor activator of nuclear factor kappa-Β ligand (RANKL) expression. These results suggested that QRC could be useful in the treatment of Aggregatibacter actinomycetemcomitans-related bone loss [22].
4. Quercetin Formulations for In Situ Osteogenesis
In the light of evidence about QRC’s strong effect in promoting osteogenesis, different strategies have been proposed to overcome its low bioavailability after oral administration; in particular, the development of targeted, sustained-release systems as scaffolds or drug delivery systems (DDSs) that are able to improve the QRC effects locally on bone tissue regeneration.
According to Wong et al., a collagen matrix mixed with QRC locally increases the bone formation when grafted into a skull defect. This study was assessed on 5-month-old New Zealand white rabbits with six defects in each parietal bone. They observed that the defects treated with QRC in the collagen matrix presented a total of 556% more new bone than those treated with the collagen matrix alone. These results confirmed the role of QRC in osteogenesis and bone healing [23].
Hydroxyapatite bioceramic microspheres with a nano-micro hybrid surface, loaded with QRC at a concentration of 200 μM (nHA/Quer) and without QRC (nHA), were prepared by Zhou et al. for the management of osteoporosis. QRC was released by the microspheres in a sustained manner for 28 days. Two groups of ovariectomized rats (OVX), both presenting inducted monocortical plug bone defects, were randomly treated with nHA or nHA/Quer particles, directly implanted into the injured sites. After eight weeks of implantation, the group treated with nHa/Quer, analysed by microfilm perfusion and micro-CT, showed a more massive formation of new bone mass and higher vessel area compared with the ones treated with nHA, demonstrating that QRC possesses osteoinductive activity and angiogenetic effect [24].
3D printing and thermally induced phase separation technology have been used by Zhu et al. to develop an innovative composite scaffold constituted of porous poly (L-lactide)/chitosan functionalized with polydopamine and QRC at a 200 μM concentration. The scaffold was analysed in vitro both on MC3T3-E1 and RAW 264.7 cells cultured for 7/14 days and 24/48 h, respectively. The results showed that the scaffold displayed an optimal osteogenic activity in terms of calcium deposition, ALP activity, and osteogenic related-genes Runx-2, COL-I, and OCN expression. Moreover, it is able to counteract the inflammatory response by a reduction in TNF-α and interleukin-6 (IL-6) expression [25].
An innovative in vitro triculture model involving osteoblast (OB), osteoclast (OC), and endothelial cells (ED) was used by Forte et al. to investigate the osteogenesis effects of a hydroxyapatite scaffold functionalized with increasing amounts of QRC up to 3.1 wt% for 7 and 14 days. They found that QRC in a time- and dose-dependent manner positively influenced the bone microenvironment. Monitoring ALP, COLL1, and the osteoprotegerin (OPG)/RANKL ratio, the authors confirmed that QRC enables osteogenesis by stimulating the osteoblast activity and proliferation, downregulating the osteoclast differentiation and promoting the angiogenetic process necessary for new bone formation [26].
References
- Alwaeli, A.Z.J. Anaerobic Bacteria Associated with Periodontitis. In Oral Microbiology in Periodontitis; InTech: Rijeka, Croatia, 2018; Charpter 3; ISBN 978-1-78923-475-6. [Google Scholar]
- Xie, Y.; Yang, W.; Tang, F.; Chen, X.; Ren, L. Antibacterial Activities of Flavonoids: Structure-Activity Relationship and Mechanism. Curr. Med. Chem. 2014. [Google Scholar] [CrossRef]
- Gutiérrez-Venegas, G.; Gómez-Mora, J.A.; Meraz-Rodríguez, M.A.; Flores-Sánchez, M.A.; Ortiz-Miranda, L.F. Effect of flavonoids on antimicrobial activity of microorganisms present in dental plaque. Heliyon 2019, 5, e03013. [Google Scholar] [CrossRef]
- Gabrilska, R.A.; Rumbaugh, K.P. Biofilm models of polymicrobial infection. Future Microbiol. 2015, 10, 1997–2015. [Google Scholar] [CrossRef]
- da Costa Júnior, S.D.; de Oliveira Santos, J.V.; de Almeida Campos, L.A.; Pereira, M.A.; Magalhães, N.S.S.; Cavalcanti, I.M.F. Antibacterial and antibiofilm activities of quercetin against clinical isolates of Staphyloccocus aureus and Staphylococcus saprophyticus with resistance profile. Int. J. Environ. Agric. Biotechnol. 2018, 3, 1948–1958. [Google Scholar] [CrossRef]
- Wang, S.; Yao, J.; Zhou, B.; Yang, J.; Chaudry, M.T.; Wang, M.; Xiao, F.; Li, Y.; Yin, W. Bacteriostatic effect of quercetin as an antibiotic alternative in vivo and its antibacterial mechanism in vitro. J. Food Prot. 2018. [Google Scholar] [CrossRef]
- Geoghegan, F.; Wong, R.W.K.; Rabie, A.B.M. Inhibitory effect of quercetin on periodontal pathogens in vitro. Phytother. Res. 2010, 24, 817–820. [Google Scholar] [CrossRef]
- Moutsatsou, P. The spectrum of phytoestrogens in nature: Our knowledge is expanding. Hormones (Athens.) 2007, 6, 173–193. [Google Scholar] [PubMed]
- Weaver, C.M.; Alekel, D.L.; Ward, W.E.; Ronis, M.J. Flavonoid Intake and Bone Health. J. Nutr. Gerontol. Geriatr. 2012, 31, 239–253. [Google Scholar] [CrossRef] [PubMed]
- Welch, A.A.; Hardcastle, A.C. The Effects of Flavonoids on Bone. Curr. Osteoporos. Rep. 2014, 12, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Coxam, V. Phyto-oestrogens and bone health. Proc. Nutr. Soc. 2008, 67, 184–195. [Google Scholar] [CrossRef]
- Zhou, C.; Lin, Y. Osteogenic differentiation of adipose-derived stem cells promoted by quercetin. Cell Prolif. 2014. [Google Scholar] [CrossRef]
- Kim, Y.J.; Bae, Y.C.; Suh, K.T.; Jung, J.S. Quercetin, a flavonoid, inhibits proliferation and increases osteogenic differentiation in human adipose stromal cells. Biochem. Pharmacol. 2006. [Google Scholar] [CrossRef]
- Futrega, K.; Mosaad, E.; Chambers, K.; Lott, W.B.; Clements, J.; Doran, M.R. Bone marrow-derived stem/stromal cells (BMSC) 3D microtissues cultured in BMP-2 supplemented osteogenic induction medium are prone to adipogenesis. Cell Tissue Res. 2018, 374, 541–553. [Google Scholar] [CrossRef]
- Pang, X.-G.; Cong, Y.; Bao, N.-R.; Li, Y.-G.; Zhao, J.-N. Quercetin Stimulates Bone Marrow Mesenchymal Stem Cell Differentiation through an Estrogen Receptor-Mediated Pathway. Biomed Res. Int. 2018, 2018, 4178021. [Google Scholar] [CrossRef]
- Prouillet, C.; Mazière, J.-C.; Mazière, C.; Wattel, A.; Brazier, M.; Kamel, S. Stimulatory effect of naturally occurring flavonols quercetin and kaempferol on alkaline phosphatase activity in MG-63 human osteoblasts through ERK and estrogen receptor pathway. Biochem. Pharmacol. 2004, 67, 1307–1313. [Google Scholar] [CrossRef]
- Li, Y.; Wang, J.; Chen, G.; Feng, S.; Wang, P.; Zhu, X.; Zhang, R. Quercetin promotes the osteogenic differentiation of rat mesenchymal stem cells via mitogen-activated protein kinase signaling. Exp. Ther. Med. 2015, 9, 2072–2080. [Google Scholar] [CrossRef]
- Wattel, A.; Kamel, S.; Prouillet, C.; Petit, J.-P.; Lorget, F.; Offord, E.; Brazier, M. Flavonoid quercetin decreases osteoclastic differentiation induced by RANKL via a mechanism involving NF kappa B and AP-1. J. Cell. Biochem. 2004, 92, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-G.; Son, K.M.; Park, H.C.; Zhu, T.; Kwon, J.H.; Yang, H.-C. Stimulating effects of quercetin and phenamil on differentiation of human dental pulp cells. Eur. J. Oral Sci. 2013, 121, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Epasinghe, D.; Yiu, C.; Burrow, M. Effect of flavonoids on remineralization of artificial root caries. Aust. Dent. J. 2016, 61, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Li, K.; Yan, H.; Liu, S.; Wang, Y.; Huang, C. High-performance therapeutic quercetin-doped adhesive for adhesive–dentin interfaces. Sci. Rep. 2017, 7, 8189. [Google Scholar] [CrossRef]
- Napimoga, M.H.; Clemente-Napimoga, J.T.; Macedo, C.G.; Freitas, F.F.; Stipp, R.N.; Pinho-Ribeiro, F.A.; Casagrande, R.; Verri, W.A. Quercetin Inhibits Inflammatory Bone Resorption in a Mouse Periodontitis Model. J. Nat. Prod. 2013, 76, 2316–2321. [Google Scholar] [CrossRef]
- Wong, R.W.K.; Rabie, A.B.M. Effect of quercetin on bone formation. J. Orthop. Res. 2008, 26, 1061–1066. [Google Scholar] [CrossRef]
- Zhou, Y.; Wu, Y.; Ma, W.; Jiang, X.; Takemra, A.; Uemura, M.; Xia, L.; Lin, K.; Xu, Y. The effect of quercetin delivery system on osteogenesis and angiogenesis under osteoporotic conditions. J. Mater. Chem. B 2017, 5, 612–625. [Google Scholar] [CrossRef]
- Zhu, L.; Chen, S.; Liu, K.; Wen, W.; Lu, L.; Ding, S.; Zhou, C.; Luo, B. 3D poly (L-lactide)/chitosan micro/nano fibrous scaffolds functionalized with quercetin-polydopamine for enhanced osteogenic and anti-inflammatory activities. Chem. Eng. J. 2019, 123524. [Google Scholar] [CrossRef]
- Forte, L.; Torricelli, P.; Boanini, E.; Gazzano, M.; Rubini, K.; Fini, M.; Bigi, A. Antioxidant and bone repair properties of quercetin-functionalized hydroxyapatite: An in vitro osteoblast–osteoclast–endothelial cell co-culture study. Acta Biomater. 2016, 32, 298–308.
