Ocular chemical and thermal burns are frequent causes of hospitalization and require immediate interventions and care. Various surgical and pharmacological treatment strategies are employed according to damage severity. Controlling inflammation and neovascularization while promoting normal ocular surface anatomy and function restoration is the principal aim. In the most severe cases, when epithelial healing is severely affected, reconstruction of the ocular surface may be a valid option, which, however, requires expertise, adequate instruments, and qualified donors. Numerous endogenous and exogenous strategies have been considered for corneal repair. Among these, stem cells and their derivatives have offered numerous attractive possibilities in finding an effective way in stimulating corneal regeneration.
- cornea
- stem cells
- extracellular vesicles
- burn injury
- wound healing
- imaging
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
1. Introduction
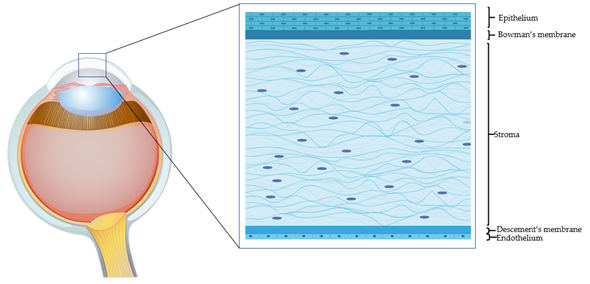
The human adult cornea, though only five layers thick, performs crucial sensory and protective functions (Figure 1). The transparent tissue allows the transmission of light and, as a refractive lens, transmits light onto the light-sensitive retina. The cornea also protects the inner ocular tissue by acting as a physical barrier to the external insults. Any minimal alteration to the properties of the cornea (including refractivity or transparency) can affect its optical functions. The prevalence of corneal pathologies worldwide is very high, and ocular burns represent the major (88%) indication for surgery [1]. Morbidity from corneal injuries ranges from mild to potentially life threatening, hence impinging negatively on the quality of life and heavily on health care systems. The corneal epithelial cells have very high turnover (every 4 to 7 days) and allow the corneal surface to regenerate continuously [2]. The limbus, where the adult (epithelial and mesenchymal) stem cells reside, is the main source of corneal epithelial cells. A series of events contribute to the successful corneal epithelium turnover [3]. However, upon severe injury, when the endogenous regenerative capacity of corneal surface is impaired due to limbal damage, there is need for alternatives. Corneal transplantation is a last-option (requires trained personnel and sophisticated instruments and is expensive) and definitive solution. The shortage of corneal tissue donors, however, does not allow fulfilling all the requests for transplantation. With the recent biotechnological advances, it has been possible to devise innovative strategies to address the problems related to corneal injuries. Current surgical and pharmacological strategies for rescuing corneal functions host several exogenous factors and drugs. Growth factor-rich hemoderivatives that elicit corneal repair exploiting endogenous mechanisms have shown considerable promises [4]. Biomechanical modulation therapy is a new treatment modality, aiming at restoration of the limbal stem cell niche that is being exploited for its capacity to regenerate the cornea after burns [5]. Stem cells such as mesenchymal stromal/stem cells (MSCs) of different origin have also been employed in attempts to regenerate the damaged cornea. Coupled to 3D technology, these systems have offered tremendous advances in the field of corneal repair. Moreover, recent knowledge gained on the cell-free approaches, such as on extracellular vesicles (EVs), have offered numerous attractive possibilities in dampening corneal damage and in stimulating healing.
In this review, we provide an update on the recent potential therapeutic avenues and clinical applications of stem cells and their products in corneal regeneration after burn injury, as well as current imaging strategies for monitoring extent of resolution.
Figure 1. The human cornea. An epithelial cell layer is found on the outer surface of the cornea, followed by a basement membrane above Bowman’s layer. The middle stromal layer contains sparse keratocytes surrounded by strands of connective tissue called collagen fibrils. The Descemet’s membrane separates the stroma from the underlying endothelium, which is the innermost layer of the cornea.
2. Corneal Burn Injury
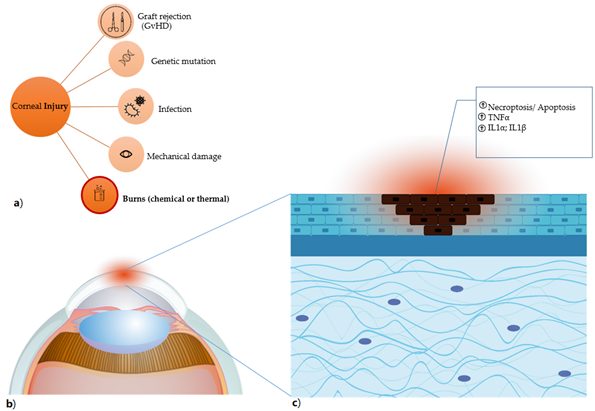
Due to the close contact with the surrounding environment, the cornea is constantly at risk of being injured. Corneal injuries can be classified according to the type of trauma and the depth of the injury [6]. Corneal injuries comprise burns of various nature including chemical, thermal, radiation, and laceration (Figure 2). The resulting ocular trauma can be limited to the more anterior structures, such as the epithelium and stroma, or can penetrate deeper into the posterior structures such as the endothelium and anterior chamber up to the crystalline. Damage can be associated with hypoxia with consequent bacterial proliferation, hence necessitating ad-hoc treatments. Other causes of corneal degeneration are genetic and autoimmune such as type I diabetes.
Burns account for up to 18% of all reported ocular traumas [7] [7]. Chemical corneal burns are very common in the workplace and are mainly caused by acidic and/or alkaline substances. Lipophilic alkalis have a much faster and deeper penetration capacity, and cause greater damage, with respect to acids [8][9][8,9]. Ensuing limbal stem pool deficiency may impair epithelialization, resulting in corneal neovascularization, lymph-angiogenesis, scar tissue formation, and immune response in the previously immune-privileged cornea. Secondary glaucoma may ensue, thus making it difficult to recover the corneal anatomical structure and physiological function, that is, sight [10][6,10].
The severity and depth of the damage, and the structures involved determine the outcome of corneal burns (Table 1). In fact, the deeper the damage is at the anatomical level and the more is the risk of infiltration by inflammatory cellular components. The latter induce, through release of cytokines and chemokines, remodeling of the stromal matrix, corneal neovascularization and lymph angiogenesis. Subsequently, scar-forming fibrotic processes entail, and blindness occurs.
Figure 2. Corneal injury (a) the different types of corneal damages are listed, in particular burns, which comprise both chemical (for instance, induced by alkali exposure) and thermal burns. (b) Anatomical detail of the damaged corneal area, highlighted in red. (c) the damage caused by alkali burn induces necroptosis and apoptosis (shown as dark cells) with result in the release of factors that trigger the inflammatory process and have TNFα, IL1α and IL1β as primum movens.
Table 1. Severity and depth of corneal damage and grading.
|
Degree of Chemical Injury |
Aim |
Clinical Treatment |
Follow-up |
|
Grades I and II |
Reduce the exposure of the chemical agent by decreasing its concentration and restoring the pH of the tear film and the surface involved |
-Sterile saline buffered with HCO3- -Lactated ringer’s solution -Balanced sterile saline solution -Glucose solution (lesion given by lime) |
This damage has a good prognosis and must be treated with antibiotics and artificial tears. |
|
Grades III and IV |
The debridement of the necrotic tissue reduces inflammation, promoting re-epithelialization. In general, it is important to intervene in the first week after the injury to have a quick recovery and to avoid blindness. |
-Debridement of the necrotic epithelium -Limbal stem cell transplant -Cultured oral mucosal epithelium transplant (COMET) -Amniotic Membrane transplant (AMT) |
If proper follow-up is not done, dry eye and secondary glaucoma can occur |