The disposition index, abbreviated DI, is an important concept in both theoretical and clinical diabetology. Serving as a biobiomarker for the function of the insulin-glucose feedback control system, i. It can be determined using various methods and provides an estimate of the loop gain of the homeostatic system. Generally, it is calculated as the product of pancreatic beta-cell function times insulin sensitivity.
- Disposition index
- hidradenitis suppurativa
- acne inversa
- prediabetes
- SPINA-GBeta
- SPINA-GR
- SPINA-DI
- Glucose clamp
- fsIGT
- fsOGT
1. Background
Background
Under physiological conditions, insulin sensitivity and beta cell function adapt to each other over a prolonged period[1]. This means that in cases of ‘healthy’ obesity, i.e. without diabetes mellitus, beta cell mass slowly increases as insulin sensitivity decreases (i.e. insulin resistance increases). Conversely, beta cell function decreases in conditions of high insulin sensitivity (e.g., in prolonged starvation). This long-term adaptation of glandular mass to demand is a general principle in endocrinology, which is referred to as dynamical compensation[2].
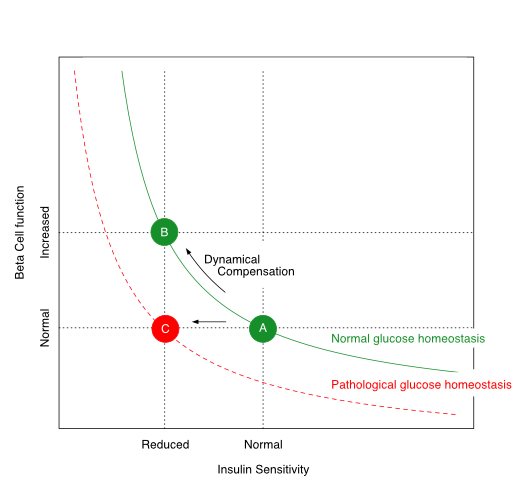
The relationship between insulin sensitivity and beta-cell function is hyperbolic in a ‘metabolically healthy’ organism. Via dynamic compensation, beta-cell mass increases with progressive insulin resistance, whereas the disposition index, which is the product of insulin sensitivity and beta-cell function (green line), remains constant (transition from A to B). If this does not happen or is insufficient (transition from A to C), the result is prediabetes or type 2 diabetes mellitus.
The disposition index, which is the product of insulin sensitivity and beta-cell function, remains constant in healthy organisms despite variations in body composition and insulin resistance. If, however, the pancreatic beta cells are no longer able to compensate for increasing insulin resistance by increased cell mass, the disposition index decreases and glucose homeostasis is impaired. This is the case in advanced metabolic syndrome. Depending on the extent of the reduction in the disposition index, prediabetes or type 2 diabetes mellitus may develop.
2. How to Determine the Disposition Index
How to Determine the Disposition Index
For determining the disposition index, data on insulin sensitivity and beta-cell function have to be obtained. This can be done in various ways:
- via a glucose clamp investigation
- via a frequently-sampled intravenous glucose tolerance test (fsIGT)
- an oral glucose tolerance test with a narrow temporal grid of measurement (‘frequently-sampled oral glucose tolerance test’, fsOGT) or
- based on fasting concentrations for glucose and insulin (SPINA Carb).
3. Calculation
3.1. GCalucose Clampculation
Glucose Clamp
If based on a glucose clamp investigation, the disposition index is calculated as the product of the insulin response curve (AUCΔInsulin) and the insulin sensitivity index (ISIClamp) with
[math]\displaystyle{DI_{Clamp}=AUC_{\Delta Insulin}\times ISI_{Clamp}}[/math]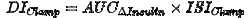 [32]
[32]
ISIClamp is the ratio of the mean glucose infusion rate and the mean insulin concentration during the clamp:
[math]\displaystyle{ISI_{Clamp}=\frac{\bar{GIR}}{[Insulin]}}[/math]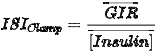
Intravenous Glucose Tolerance Test
3.2. Intravenous Glucose Tolerance Test
Using the frequently sampled intravenous glucose tolerance test (fsIGT)IGT, the time series of insulin and glucose concentration are to be fitted to the minimal model of glucose homeostasis by Bergman and Cobelli. Then the disposition index can be calculated with
[math]\displaystyle{DI_{fsIGT}=\varphi_1 \times S_1}[/math]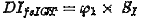
from the first phase of the insulin response (φ1) and the insulin sensitivity index (S1)[43].
3.3. Oral Glucose Tolerance Test
If the frequently sampled oral glucose tolerance test (fsOGT)OGT is used, it is to be coupled with the approach of Matsuda and DeFronzo. Then, the disposition index can be calculated with
[math]\displaystyle{DI_{fsOGT}=IGI \times ISI_{composite}}[/math]
from the insulinogenic index (IGI) and the insulin sensitivity index (ISIcomposite)[54].
3.4. SPINA Carb
This method delivers a static disposition index that requires fasting concentrations of insulin and glucose only. It is calculated with
[math]\displaystyle{SPINA\text{-}DI=SPINA\text{-}G_{Beta} \times SPINA\text{-}G_R}[/math]
as the product of the secretory capacities of pancreatic beta cells (SPINA-GBeta) and the reconstructed insulin receptor gain (SPINA-GR)[65][76].
Interpretation
4. Interpretation
The approaches presented provide similar but slightly different information. Even though the results of the four methods correlate significantly with each other[7], several biological factors may cause certain deviations. These are rooted, for example, in the different mechanisms that determine static and dynamic insulin secretion patterns. In a comparative study, the discriminatory power of the static disposition index for the diagnosis of diabetes mellitus was higher than that of the oGTT-based disposition index according to Matsuda and DeFronzo[7].
5. Clinical Significance
Prognostic aspects
ThA reduced disposition index is reduced in diabetes mellitus and prepredicts the evolution of type 2 diabetes[7][8]. It is also reduced in certain chronic and inflammatory conditions, including cystic fibrosis[98], reduced PCSK9 expression[109], obstructive sleep apnea[11] anand hidradenitis suppurativa (aka acne inversa)[1210].
6. Prognostic aspects
A reduced disposition index predicts the evolution of type 2 diabetes[13]. In a prospective evaluation of the NHANES study, a reduced static disposition index (SPINA-DI) predicted all-cause mortality over 10 years[14].
7. Therapeutic interventions
Therapeutic measures leading to an improved disposition index include physical activity and nutritional interventions[15]. In carriers of the risk allele of the gene for the transcription factor TCF7L2 increased dietary fibre intake led to a rising disposition index[1611].
References
- Richard N. Bergman; Marilyn Ader; Katrin Huecking; Gregg Van Citters; Accurate Assessment of β-Cell Function. Bergman RN, Ader M, Huecking K, Van Citters G. Accurate assessment of beta-cell function: the hyperbolic correction. Diabetes. 2002, 51, S212-S220. Suppl 1, S212-20.
- Omer Karin; Avital Swisa; Benjamin Glaser; Yuval Dor; Uri Alon; Dynamical compensation in physiological circuits. Shah SS, Ramirez CE, Powers AC, Yu C, Shibao CA, Luther JM. Hyperglycemic clamp-derived disposition index is negatively associated with metabolic syndrome severity in obese subjects. Metabol. Syst. Biol.. ism. 2016, 12, 886., 65(6), 835-42.
- Sapna S. Shah; Claudia E. Ramirez; Alvin C. Powers; Chang Yu; Cyndya A. Shibao; James M. Luther; Hyperglycemic clamp-derived disposition index is negatively associated with metabolic syndrome severity in obese subjects. MeBergman RN. Origins and History of the Minimal Model of Glucose Regulation. Front Endocrinol (Lab.. usanne). 20216, 65, 835-842., 11, 583016.
- Richard N. Bergman; Origins and History of the Minimal Model of Glucose Regulation. FronMatsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabet.es Endocrinol.. 202Care. 1, 11, 583016.999, 22, 1462-70.
- M Matsuda; R A DeFronzo; Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp.. DDietrich JW, Dasgupta R, Anoop S, Jebasingh F, Kurian ME, Inbakumari M, Boehm BO, Thomas N. SPINA Carb: a simple mathematical model supporting fast in-vivo estimation of insulin sensitivity and beta cell function. Sciabetes CarRe. 1999, p. 2022, 122, 1462-1470., 17659.
- Johannes W. Dietrich; Riddhi Dasgupta; Shajith Anoop; Felix Jebasingh; Mathews E. Kurian; Mercy Inbakumari; Bernhard O. Boehm; Nihal Thomas; SPINA Carb: a simple mathematical model supporting fast in-vivo estimation of insulin sensitivity and beta cell function. ScDietrich JW, Abood A, Dasgupta R, Anoop S, Jebasingh FK, Spurgeon R, Thomas N, Boehm BO. A novel simple disposition index (SPINA-DI) from fasting insulin and glucose concentration as a robust measure of carbohydrate homeostasis. J Di. Rabetep.. s. 2022, 4, 12, 1-13.6, e13525.
- Johannes W. Dietrich; Assjana Abood; Riddhi Dasgupta; Shajith Anoop; Felix K. Jebasingh; R. Spurgeon; Nihal Thomas; Bernhard O. Boehm; A novel simple disposition index (SPINA‐DI) from fasting insulin and glucose concentration as a robust measure of carbohydrate homeostasis. J. Lorenzo C, Wagenknecht LE, Rewers MJ, Karter AJ, Bergman RN, Hanley AJ, Haffner SM. Disposition index, glucose effectiveness, and conversion to type 2 diabetes: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes. Care. 201024, 16, e13525., 33, 2098-103.
- K.M. Venkat Narayan; Dimple Kondal; Howard H. Chang; Deepa Mohan; Unjali P. Gujral; Ranjit Mohan Anjana; Lisa R. Staimez; Shivani A. Patel; Mohammed K. Ali; Dorairaj Prabhakaran; Nikhil Tandon; Viswanathan Mohan; Natural History of Type 2 Diabetes in Indians: Time to Progression. Nielsen BU, Mathiesen IHM, Krogh-Madsen R, Katzenstein TL, Pressler T, Shaw JAM, Rickels MR, Almdal TP, Faurholt-Jepsen D, Stefanovski D. Insulin sensitivity, disposition index and insulin clearance in cystic fibrosis: a cross-sectional study.. Diabetes Cologiare. . 2024, 4, 67, 858-863., 2188-2198.
- Bibi U. Nielsen; Inger H. M. Mathiesen; Rikke Krogh-Madsen; Terese L. Katzenstein; Tacjana Pressler; James A. M. Shaw; Michael R. Rickels; Thomas P. Almdal; Daniel Faurholt-Jepsen; Darko Stefanovski; Insulin sensitivity, disposition index and insulin clearance in cystic fibrosis: a cross-sectional study. DCyr Y, Lamantia V, Bissonnette S, Burnette M, Besse-Patin A, Demers A, Wabitsch M, Chrétien M, Mayer G, Estall JL, Saleh M, Faraj M. Lower plasma PCSK9 in normocholesterolemic subjects is associated with upregulated adipose tissue surface-expression of LDLR and CD36 and NLRP3 inflammasome. Physiabetol.. Rep. 2024, 67, 2188-2198.1, 9, e14721.
- Yannick Cyr; Valérie Lamantia; Simon Bissonnette; Melanie Burnette; Aurèle Besse‐Patin; Annie Demers; Martin Wabitsch; Michel Chrétien; Gaétan Mayer; Jennifer L. Estall; Maya Saleh; May Faraj; Lower plasma PCSK9 in normocholesterolemic subjects is associated with upregulated adipose tissue surface‐expression of LDLR and CD36 and NLRP3 inflammasome. PhysAbu Rached N, Dietrich JW, Ocker L, Stockfleth E, Haven Y, Myszkowski D, Bechara FG. Endotyping Insulin-Glucose Homeostasis in Hidradenitis Suppurativa: The Impact of Diabetes Mellitus and Inflammation. J Cliol.n Rep.. Med. 2021, 9, e14721.5, 14, 2145.
- Abu Youssef HA, Elshazly MI, Rashed LA, Sabry IM, Ibrahim EK. Insulin resistance in obstructive sleep apnea. EgyptDietrich JW. P4-Endokrinologie – Kybernetische Perspektiven eines neuen Ansatzes. Leiabn Journal of Chest Diseases and Tubiz Onlinerculosis. . 20124, 63, 133-9., 54, 20.
- Nessr Abu Rached; Johannes W. Dietrich; Lennart Ocker; Eggert Stockfleth; Yannik Haven; Daniel Myszkowski; Falk G. Bechara; Endotyping Insulin–Glucose Homeostasis in Hidradenitis Suppurativa: The Impact of Diabetes Mellitus and Inflammation. J. Clin. Med.. 2025, 14, 2145.
- Carlos Lorenzo; Lynne E. Wagenknecht; Marian J. Rewers; Andrew J. Karter; Richard N. Bergman; Anthony J.G. Hanley; Steven M. Haffner; Disposition Index, Glucose Effectiveness, and Conversion to Type 2 Diabetes. Diabetes Care. 2010, 33, 2098-2103.
- Dietrich JW. P4-Endokrinologie – Kybernetische Perspektiven eines neuen Ansatzes. Leibniz Online. 2024, 54, 20.
- Thomas P. J. Solomon; Steven K. Malin; Kristian Karstoft; Sangeeta R. Kashyap; Jacob M. Haus; John P. Kirwan; Pancreatic β-cell Function Is a Stronger Predictor of Changes in Glycemic Control After an Aerobic Exercise Intervention Than Insulin Sensitivity. J. Clin. Endocrinol. Metab.. 2013, 98, 4176-4186.
- Ulla K. Tolonen; Maria A. Lankinen; Markku Laakso; Ursula S. Schwab; Association of dietary fibre with type 2 diabetes risk is modified by transcription factor 7 like 2 genotype in men with impaired fasting glucose: The T2D-GENE study. Clin. Nutr.. 2025, 53, 262-269.
