Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Catherine Yang and Version 4 by Stefano Bacci.
Photobiomodulation (PBM), formerly known as low-level laser light therapy (LLLT), is a safe phototherapy technique that uses wavelengths of the visible light spectrum which includes red light (RL, 620–700 nm) and near-infrared (NIR, 700–1440 nm). This treatment modality has been used in dermatology, both in clinical settings and at home. PBM involves the use of various light sources, including low-level lasers (LLL) and light-emitting diodes (LED), to deliver therapeutic light. Reviews on the matter have already been conducted.
- photobiomodulation
- dermatology
- laser
- photodynamic therapy
- LED
1. Introduction
Endre Mester, a Hungarian physician, first created the idea of photobiomodulation (PBM) in 1967 while researching the effects of laser light exposure on the growth of cancer cells in a mouse model. Mester discovered an unanticipated acceleration of hair regeneration during this investigation [1]. Naturally, since its inception, light therapy has undergone tremendous changes and has grown in scope. PBM has demonstrated efficacious outcomes in the management of non-healing wounds, scars, ulcers, musculoskeletal disorders, persistent pain, analgesia, and immunological regulation [2].
Increasingly, research indicates that particular electromagnetic radiation wavelengths, from visible to infrared, can produce photophysical and photochemical effects that can alter important biological processes in a variety of eukaryotic organs, including humans. Hence, non-ionizing light sources in the visible and infrared range, such as broadband lights, low-level lasers, and Light-Emitting Diodes (LEDs), are used in treatment to activate endogenous chromophores and stimulate biological functions in a non-thermal and, most importantly, non-cytotoxic manner [3][4].
The main characteristic of PBM is the direct interaction of continuous wave light at specific wavelengths directly with the tissue, i.e., with the endogenous chromophores.
However, due to a lack of understanding of the photo-physics and radiometric parameters that affect PBM’s accuracy and reliability, as well as a lack of knowledge about how PBM achieves its molecular effects, there is still disagreement about its practical application.
2. Blue LED Therapy
Blue LED technology was created in the early 1990s and has since found many uses in the biochemical and biological domains [5][6]. In fact, blue LED technology offers the possibility of a straightforward and affordable source for focusing on specific biological components, given that a number of biological molecules and chromophores exhibit a high absorption rate in the UV/blue area of the spectrum [7]. One use for it is the process of wound healing.
Blue light is absorbed mainly by the heme group, which can be found in the hemoglobin and in the cytochromes. These widely distributed biological elements have the capacity to trigger one or more intracellular signaling pathways following radiation exposure, which can alter the healing process [8]. Protoporphyrin IX is a chromophore that increases the sensitivity of cytochrome C and cytochrome C oxidase to blue light in the mitochondrial electron transport chain [8][9][10][11].
Cytochrome C and cytochrome C oxidase, once activated by blue light, strengthen the process of cellular respiration by interacting with the final two complexes of the chain and adjusting the ATP production [11][12]. For this reason, mitochondria represent a target organelle for blue light radiation. Mitochondria are involved in redox signaling and in maintaining the balance of reactive oxygen species (ROS), which is essential for several vital functions such as calcium homeostasis. In a preliminary study, Magni et al. [13] demonstrated that under blue light exposure, ROS are stimulated dose-dependently and that mitochondria are subject to morphological changes.
According to André-Lévigne et al. [14] and Dunnill et al. [15], flavins, which stimulate the synthesis of ROS and play a role in the signal transduction mechanism in numerous cellular pathways involved in tissue repair, can also be used to explain the therapeutic action of blue light. The shift from this phase to the proliferative one is facilitated by the modulation of ROS, which causes a controlled increase in inflammatory functions [16][17]. The macrophage phenotypic transition from M1 to M2 may also be responsible for this [2][3].
Compared to wounds that are not treated with blue light, wounds treated with it exhibit a quicker healing process as well as improved dermal collagen deposition and morphology [7][18][19][20][21][22]. Additionally, the modulation of the inflammatory response is better in wounds that have been treated. His process can be attributed to photochemical effects: nitric oxide release and fibroblast activation brought on by blue light promote re-epithelialization [8][23][24]. According to Fraccalvieri et al. [12] and Orlandi et al. [25], blue light helps injured tissue by regulating its energy supply, which is particularly important during the phases of proliferation and remodeling. It also establishes tissue repair, with a decrease in scar tissue and the likelihood of developing keloids, as well as the stimulation of angiogenesis [25][26].
In animal models of chronic ulcers, blue light treatment has also been shown to have a proangiogenic effect; this suggests that blue light therapy may be helpful throughout the whole tissue repair process [27]. In addition, blue light has been shown to have anti-inflammatory cytokine release, bacterial load reduction, and granulation stimulation [13][23][24][28]. The safety and efficacy of blue light in treating skin lesions, Inflammatory acne [29][30], burns [24], psoriasis [31][32][33][34], eczema [35], and diabetic ulcers are among the conditions that blue light is reported to be safe and effective for treating. Despite the evidence presented above, relatively few methodologically rigorous experiences have been conducted in daily clinical practice focused on chronic wounds [12].
In an in vitro research context, Rossi et al. [19] investigated the impact of blue LED light on the proliferation and metabolism of human fibroblasts derived from healthy skin cocultured with keratinocytes. As described in their article, the authors suggested using blue LED light to modulate the metabolism and growth of human fibroblasts.
Furthermore, human fibroblasts isolated from keloids and perilesional tissues were subjected to blue LED light irradiation, which was examined by Magni et al. [18]. The authors utilized various experimental techniques to demonstrate that blue LED light can modulate cell proliferation and metabolism in a dose-dependent manner and that these effects persist for at least 48 h after treatment.
Moreover, in keloid-derived fibroblasts and perilesional fibroblasts, the highest radiation doses decrease cell viability 24 and 48 h after treatment, respectively. In order to treat hypertrophic scars and keloids, the authors concluded that blue light irradiation was a novel and minimally invasive treatment option.
3. Photodynamic Therapy
Today, photodynamic therapy (PDT), which was first developed by Von Toppeiner and Jesionek in partnership [36], is extensively utilized to treat a wide range of illnesses [37]. The application of this therapy in dermatology spans the spectrum from treating bacterial, fungal, viral, immunological, or inflammatory illnesses to managing chronic wounds, including photorejuvenation in cosmetology [38].
The application of photosensitizers activated by a specific wavelength of light energy is used in this therapy: the topical use of 5 Aminolaevulinic Acid (ALA) has represented a breakthrough in PDT in the dermatological field because it is easily absorbed by the skin [39][40].
The molecular mechanism of action of PDT is complex. When triplet oxygen (3O2) is present, the photo-sensitizer can enter the tissue. The main purpose of PDT is to have a selective photokilling effect on a pathologic target while promoting healing in healthy tissue. In order to reach this goal, a photosensitizer is used and included in the target tissue. The photosensitizer has an absorption peak at a specific wavelength: when it is exposed to a light source (usually a laser) emitting at this wavelength, it generates Reactive Oxygen Species (ROS) that are very unstable. The generation of ROS can vary depending on the energy input and the characteristics of the photosensitizers [27]. While less noticeable levels of ROS may promote tissue proliferation and/or regeneration, high levels may cause a photokilling effect. This approach has been usually proposed in the treatment of cancerous cells or in the inactivation of multidrug-resistant pathogens [41].
PDT is used in medicine to treat a wide range of pathologies, both oncological and non-oncological [42][43]. As almost all the therapies are based on the use of light sources, its advantages include minimal invasiveness, ease of use in an outpatient setting, and a strong track record of short- and long-term safety.
Intravenous injection of photo-sensitizer can cause damage at the vascular level. Hypoxic damage can be beneficial in treating neoplasms, but it can also be detrimental in treating chronic non-neoplastic wounds because it exacerbates the hypoxic state, which is a major factor in noxa.
Without a single, perfect photo-sensitizer, the selection process should focus on molecules that have a proven track record of improving skin ulcer healing and can be applied topically. Two reviews [41][44] have recently examined this vast topic. Photo-sensitizers for chronic ulcers have been tested using various chemical categories, primarily in preclinical settings and a few pilot studies. These chemical categories include phenothiazines (methylene blue and toluidine blue), xanthenic dyes (rose bengal), and tetrapyrrolic macrocycles and analogs (porphyrins, chlorines, and phthalocyanines).
The selection of the light source is also very important. In clinical practice, PDT is performed using laser or LED (Light Emitting Diodes) sources. Lasers are strictly monochromatic, thus enabling an excellent matching with the photosensitizer absorption curve, high fluences and a spatially narrow beam. On the other hand, LED sources usually present a large emission spectrum but are more affordable, and their wide angular emission can cover larger tissue areas. The wavelength controls how well light can pass through tissue. Specifically, lengths between 600 and 800 nm are thought to have sufficient skin penetration to be utilized in clinical settings. Fundamentally, red is the color that penetrates the skin the most, followed by green and blue [45].
Given that the technique relies on a tissue’s interaction with light energy, it is clear that the effectiveness is directly correlated with the total amount of energy applied per treated area’s volume. A number of parameters, including power, irradiance, energy density, irradiation time, and release of light mode (simple or fractional), can be used to express this [46]. Energy density, which is expressed as J/cm and is derived from the measurement of time (in seconds) and irradiance (in W/cm2), is the most widely used format for reporting a PDT treatment schedule [47].
According to research on wound healing, particularly chronic wounds, PDT can cause an acute inflammatory response that is primarily related to immune system activation [48].
This is supported by the description of how PDT not only causes new fibroblasts (effector cells) to diversify but also fosters close relationships between these cell types and mast cells, which are positive for TNF-α and Fibroblast Growth Factor (FGF) in their granules. This was reported by Corsi et al. [49].
Thus, these results support the hypothesis that mast cells could transmit signals for the same fibroblast recruitment and differentiation following therapy [49]. When it comes to mast cells, they proliferate and degranulate during the course of treatment. Their increase could have resulted from nearby cells migrating, precursors already present in the tissue differentiating, or precursors entering the tissue and differentiating into mast cells.
As a result, these cell types would be both attracted and stimulated to release their granules into the dermis in reaction to the therapy. During therapy, the venules, or the vessels of the sub-papillary plexus, appear to be a preferred location for cell infiltration and clustering [49].
The presence of TNF-alpha, GM-CSF, and TGF-β in mast cells after PDT treatment provides additional evidence of immune system activation. TNF-alpha plays a crucial role in differentiating dendritic cells, including plasmacytoid cells, which interact with regulatory T-type lymphocytes. GM-CSF is also involved in this process. TGF-beta is essential for the differentiation of macrophages.
According to Grandi et al. [40], there is no doubt that the induction of TGF-beta is connected to the subsequent decrease in wound volume. In fact, TGF-beta seems to affect the epithelial-mesenchymal transition—which permits keratinocyte migration from the margins toward the wound bed—at different phases of ulcer healing. Additionally, this cytokine can stimulate myofibroblast differentiation as a component of the processes observed in scar reshaping [50].
Additional research has demonstrated that PDT significantly affects neutrophil activation, which may account for the rise in pro-inflammatory cytokines following treatment. Lipid mediators are produced in tandem with the acute phase of inflammation resolution and the restoration of tissue homeostasis). These mediators have been linked to anti-inflammatory and immunomodulatory properties, such as the inhibition of leukocyte chemotaxis, the blockade of TNF-alpha and IL-6 production, and the induction of increased IL-10 expression [51][52][53][54]. As a result, the researchers can draw the conclusion that PDT significantly affects the immune system, having both immunostimulatory and immunosuppressive effects. It also likely influences the type of cell death that is induced.
According to Steinmann [55], the nervous system has the ability to control the immune system’s activity; ulcer healing is another example of this close relationship. Actually, results from experiments indicate that neurogenic stimuli significantly impact wound healing following injury and that delayed wound healing following skin nerve resection is seen in animal models [56][57].
Studies have demonstrated that following PDT treatment, there is an increase in neuronal populations belonging to the autonomous nervous system, which is found in the dermis. These neuronal populations contain the typical nerve mediators involved in ulcer healing (CGRP, NGF, NKA, NPY, SP, PGP 9.5, and VIP). Additionally, after a single irradiation, the proportion of mast cells that contain and secrete VIP and NGF rises. Given that mast cell degranulation is stimulated by both VIP and NGF, these results appear to be consistent with the previously documented rise in mast cell degranulation index following PDT treatment, indicating that neurogenic stimuli may play a role in this phenomenon.
In light of this, the researchers can presume that an increase in NGF and VIP release following therapy results in mast cell activity and that these mediators can activate dermal neurons and nerve fibers [54][58][59]. Corsi et al. [49] suggest that increased TGF-beta, cellular infiltrate response, and increased ECM secretion by fibroblasts may all be related to the activation of nerve fibers.
Due to its gaseous nature and relatively short half-life, NO is the smallest known signaling molecule that can cross membranes freely. It has recently been added to the list of mediators involved in wound healing [60]. In fact, the presence of bacterial antigens, apoptotic bodies, or inflammatory cytokines increases the expression of the enzyme, which suggests this molecule is derived from the NOS enzyme complex, where the inducible isoform is overregulated during stressful situations.
The inflammatory phase of wound repair, which is characterized by the promotion of vasodilation and antibacterial activity, has been theorized to be facilitated by iNOS [54][61][62]. Experimental preliminary results show increased expression of iNOS in chronic wounds treated with photodynamic therapy. In contrast to granulocytes to M2-type macrophages, vessels, and neurons where iNOS expression increases, mast cells have a higher degranulation index and contain iNOS; however, the proportion of these cells containing this mediator decreases following treatment [63].
However, research is currently being done in the lab to determine how different cell types respond to PDT in terms of iNOS secretion and subsequent wound healing.
4. LED vs. Low-Level Laser Light Therapy Comparison
The treatment known as PBM has been labeled by various terms. The term “photobiomodulation” is more widely accepted among authors as it refers to the general mechanism, whereas using the term LLLT may confuse the reader into thinking that PBM can only be done with lasers [64].
PBM is used to refer to the interaction of light sources with a target modulatory action on specific biological reactions or pathways. The term LLLT arises from the discovery of the photobiomodulatory effects of lasers on the periphery of treated lesions. Despite the fact that this term has been widely used, PBM effects on the skin can be obtained not only by applying a laser at low energies with that intention. LED lights or non-coherent sources, without seeking selective photothermolysis, can also be used for PBM [65] (Figure 1).
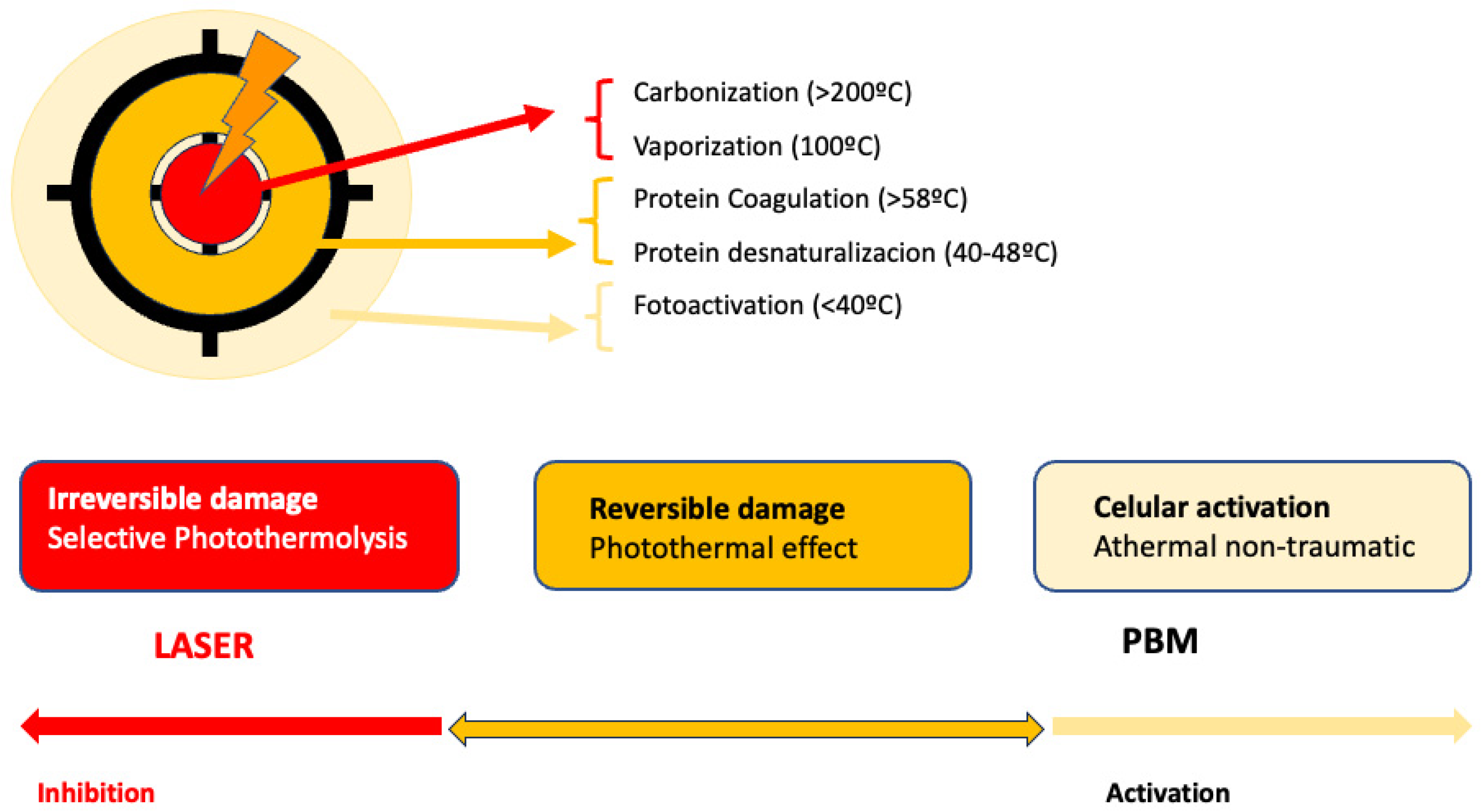
Figure 1. Represents the action of lasers in dermatology: In the center, selective photothermolysis occurs with the selective destruction of the chromophore and necrosis of the target tissue. In the surrounding tissue, PMB effects occur, corresponding to the dissipation of laser energy or lower doses.
Consequently, there are two main ways to apply PBM in dermatology. One method involves using LED lights, while the other utilizes low-dose lasers below the selected target threshold. Both light sources differ in some key aspects. Laser light is coherent and exact, whereas LED light is non-coherent in a bandwidth of 1–2 nm [64]. The application methods also vary. Despite using low doses [66], lasers deliver high energy in a short time, resulting in short sessions administered by an expert dermatologist [67]. Laser devices are more expensive. LEDs, on the other hand, are simple, more affordable devices that do not require specialized handling. LEDs apply energy over a longer duration compared to lasers [65]. For PBM applications, both devices require repeated sessions, with protocols not clearly established, typically ranging from once per week to multiple times per week [68]. Most of the published works on PBM utilize lasers as light sources, representing up to 90 percent of the more than 3000 published works [64]. This could lead to the wrong assumption that PBM is only achieved with lasers. However, numerous studies currently support the idea that LEDs are another valid option for applying PBM. Table 1 shows the differences between laser and LED devices when used as light sources in PBM.
Table 1. Summary of published clinical trials on PMB and photorejuvenation and wrinkles treatment.
| Author/Year | Type of LED | Patients | Design of the Study | Protocol of Treatment | Results |
|---|---|---|---|---|---|
| Weis 2005 [69] | RL 590 nm | N = 90 | 8 treatments in 4 weeks 6 months follow-up |
0.1 J/cm2 pulsing | 90% of patients reduced photoaging signs. Histological response: - 90% improve Collagen I - 4% decrease MMPI |
| Russell 2005 [70] | RL 630 nm + NIR 830 nm |
N = 31 | 9 light treatments Flow up weeks 9 and 12 |
RL 126 J/cm2 NIR 66 J/cm2 |
52% of patients reduced photoaging signs 81% of patients reported improvement in periocular wrinkles |
| Goldberg 2007 [71] | RL 630 nm + NIR 830 nm |
N = 36 | 9 treatments in 12 weeks | RL 126 J/cm2 NIR 66 J/cm2 |
Significant improvement in softness, smoothness, and firmness |
| Yoon-Lee 2007 [72] | RL 630 nm + NIR 830 nm |
N = 112 | 4 Groups: NIR, RL, NIR + RL and placebo 8 sessions, 4 weeks, and 3 months follow-up |
RL 126 J/cm2 NIR 66 J/cm2 |
Both RL and NIR had effective and significant wrinkle reduction Skin elasticity better NIR and NIR + RL Melanin decrease RL |
| Baez 2007 [73] | RL 630 nm + NIR 830 nm |
N = 30 | 9 sessions, 12 weeks | RL 126 J/cm2 NIR 66 J/cm2 |
91% color improvement 82% smoothness improvement 25–50% investigator assessment improvement |
| Wunsch 2014 [74] | RLT 611–650 nm ELT 570–850 nm |
N = 136 | 2 sessions per week 30 treatments 3 Groups: RLT, ELT, and placebo |
No difference between wavelengths Both treatments have significant differences in wrinkles |
|
| Hee-Nam 2017 [75] | RL 660 nm LED 411–777 nm |
N = 52 | 1 session/day 12 weeks 2 Groups: RL, LED |
5.17 J/cm2 | Both treatments significantly improve wrinkles |
| Rocha-Mota 2023 [76] | RL 660 nm AL 590 nm |
N = 137 Split-face |
10 sessions periocular 4 weeks |
3.8 J/cm2 | Significant periocular wrinkles, with RL 31.6% and 29.9% with AL. |
The use of light in a no-thermal effect is supported by the photon’s absorption of the cells’ receptors. The three main chromophores in the skin are melanin in the epidermis, hemoglobin in the dermis, and water in all the skin, with longer wavelengths achieving deeper penetration (Figure 2) (1). Red light (RL) targets melanin and hemoglobin, whereas NIR light targets water in the deeper layers of the epidermis [77] (Figure 3). Blue light (BL 400–500 nm) has been included in some devices, but it is considered very close to ultraviolet light with deleterious effects on the skin and without modulatory effects [78].
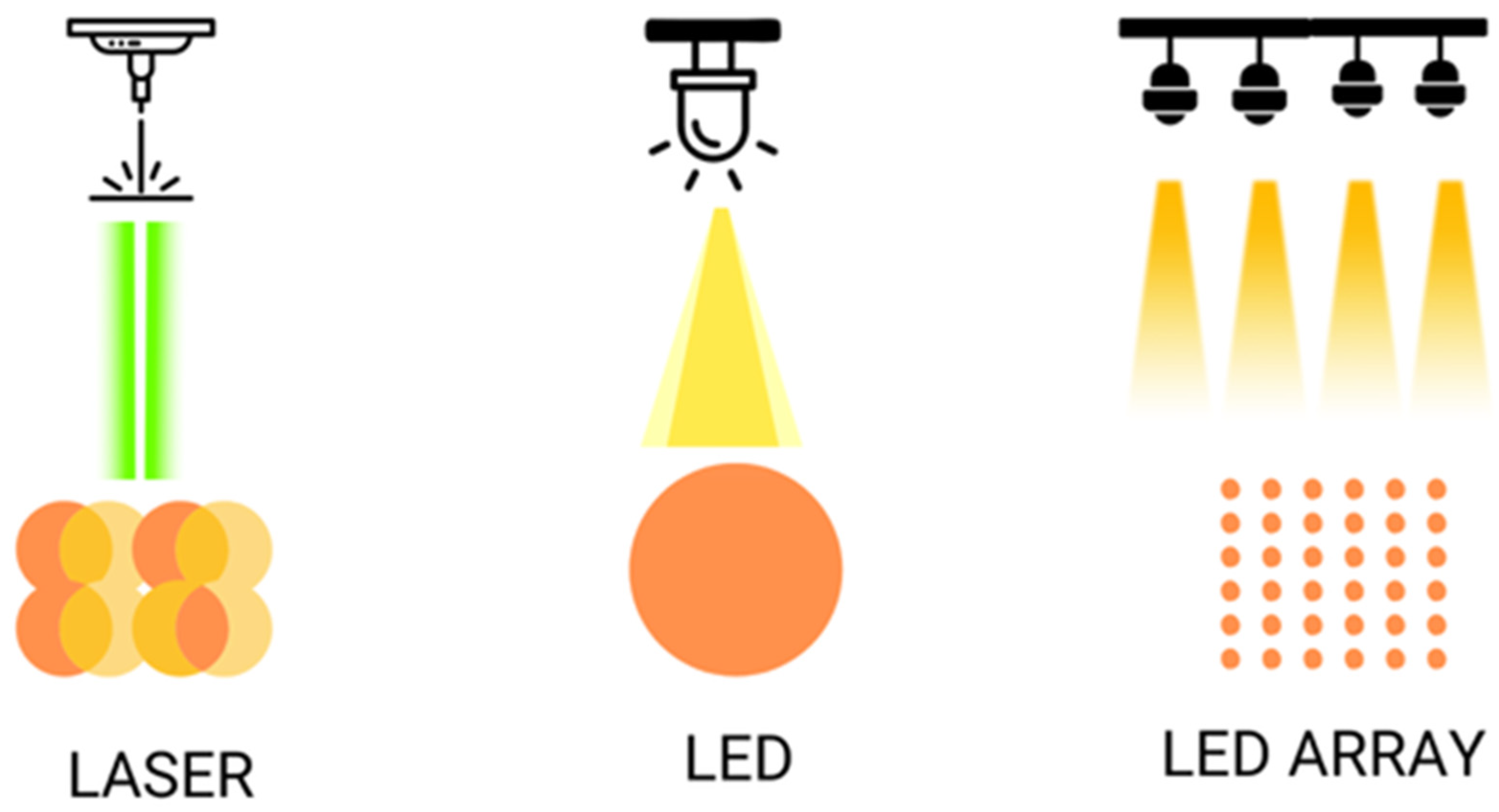
Figure 2. Shows the different ways of illumination with laser and LED, simple or on arrays.
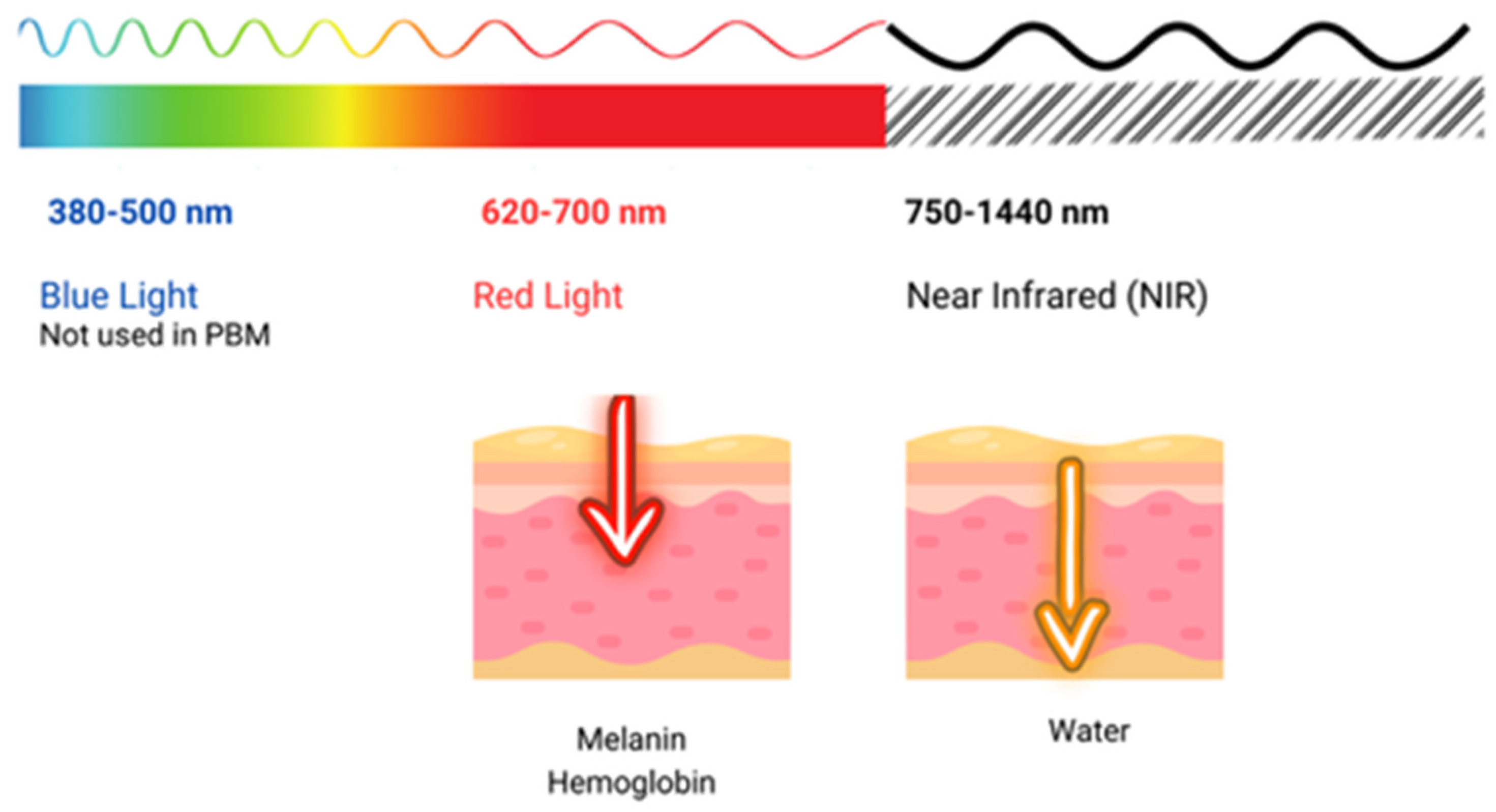
Figure 3. Shows the penetration of light at different wavelengths throughout the visible and near-infrared (NIR) spectrum.
References
- Mester, E.; Szende, B.; Gärtner, P. The effect of laser beams on the growth of hair in mice. Radiobiol. Radiother. 1968, 9, 621–626.
- Tripodi, N.; Corcoran, D.; Antonello, P.; Balic, N.; Caddy, D.; Knight, A.; Meehan, C.; Sidiroglou, F.; Fraser, S.; Kiatos, D.; et al. The Effects of Photobiomodulation on Human Dermal Fibroblasts in Vitro: A Systematic Review. J. Photochem. Photobiol. B Biol. 2021, 214, 112100.
- Kuffler, D.P. Photobiomodulation in Promoting Wound Healing: A Review. Regen. Med. 2016, 11, 107–122.
- Shaikh-Kader, A.; Houreld, N.N. Photobiomodulation, Cells of Connective Tissue and Repair Processes: A Look at In Vivo and In Vitro Studies on Bone, Cartilage and Tendon Cells. Photonics 2022, 9, 618.
- Yeh, G.; Wu, C.-H.; Cheng, T.-C. Light-Emitting Diodes—Their Potential in Biomedical Applications. Renew. Sustain. Energy Rev. 2010, 14, 2161–2166.
- Wang, H.-C.; Chen, Y.-T. Optimal Lighting of RGB LEDs for Oral Cavity Detection. Opt. Express 2012, 20, 10186–10199.
- Cicchi, R.; Rossi, F.; Alfieri, D.; Bacci, S.; Tatini, F.; De Siena, G.; Paroli, G.; Pini, R.; Pavone, F.S. Observation of an Improved Healing Process in Superficial Skin Wounds after Irradiation with a blue-LED Haemostatic Device. J. Biophotonics 2016, 9, 645–655.
- Passarella, S.; Karu, T. Absorption of Monochromatic and Narrow Band Radiation in the Visible and near IR by Both Mitochondrial and Non-Mitochondrial Photoacceptors Results in Photobiomodulation. J. Photochem. Photobiol. B 2014, 140, 344–358.
- Mason, M.G.; Nicholls, P.; Cooper, C.E. Re-Evaluation of the near Infrared Spectra of Mitochondrial Cytochrome c Oxidase: Implications for Non Invasive in Vivo Monitoring of Tissues. Biochim. Biophys. Acta (BBA)-Bioenerg. 2014, 1837, 1882–1891.
- Hamblin, M.R. Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation. Photochem. Photobiol. 2018, 94, 199–212.
- Magni, G.; Banchelli, M.; Cherchi, F.; Coppi, E.; Fraccalvieri, M.; Pugliese, A.M.; Pedata, F.; Mangia, A.; Gasperini, S.; Pavone, F.S.; et al. Human Keloid Cultured Fibroblasts Irradiated with Blue LED Light: Evidence from an in Vitro Study. In Proceedings of the Medical Laser Applications and Laser-Tissue Interactions IX, Munich, Germany, 23–25 June 2019; Optica Publishing Group: Washington, DC, USA, 2019; p. 11079_31.
- Fraccalvieri, M.; Amadeo, G.; Bortolotti, P.; Ciliberti, M.; Garrubba, A.; Mosti, G.; Bianco, S.; Mangia, A.; Massa, M.; Hartwig, V.; et al. Effectiveness of Blue Light Photobiomodulation Therapy in the Treatment of Chronic Wounds. Results of the Blue Light for Ulcer Reduction (B.L.U.R.) Study. Ital. J. Dermatol. Venerol. 2022, 157, 187–194.
- Magni, G.; Tatini, F.; Bacci, S.; Rossi, F. Blue LED Light Affects Mitochondria and Modulates Reactive Oxygen Species: Preliminary in Vitro Results. In Proceedings of the Translational Biophotonics: Diagnostics and Therapeutics III, Munich, Germany, 25–30 June 2023; Lilge, L.D., Huang, Z., Eds.; SPIE: Munich, Germany, 2023; p. 37.
- André-Lévigne, D.; Modarressi, A.; Pepper, M.S.; Pittet-Cuénod, B. Reactive Oxygen Species and NOX Enzymes Are Emerging as Key Players in Cutaneous Wound Repair. Int. J. Mol. Sci. 2017, 18, 2149.
- Dunnill, C.; Patton, T.; Brennan, J.; Barrett, J.; Dryden, M.; Cooke, J.; Leaper, D.; Georgopoulos, N.T. Reactive Oxygen Species (ROS) and Wound Healing: The Functional Role of ROS and Emerging ROS-Modulating Technologies for Augmentation of the Healing Process. Int. Wound J. 2017, 14, 89–96.
- Naik, E.; Dixit, V.M. Mitochondrial Reactive Oxygen Species Drive Proinflammatory Cytokine Production. J. Exp. Med. 2011, 208, 417–420.
- Landén, N.X.; Li, D.; Ståhle, M. Transition from Inflammation to Proliferation: A Critical Step during Wound Healing. Cell. Mol. Life Sci. 2016, 73, 3861–3885.
- Magni, G.; Banchelli, M.; Cherchi, F.; Coppi, E.; Fraccalvieri, M.; Rossi, M.; Tatini, F.; Pugliese, A.M.; Rossi Degl’Innocenti, D.; Alfieri, D.; et al. Experimental Study on Blue Light Interaction with Human Keloid-Derived Fibroblasts. Biomedicines 2020, 8, 573.
- Rossi, F.; Magni, G.; Tatini, F.; Banchelli, M.; Cherchi, F.; Rossi, M.; Coppi, E.; Pugliese, A.M.; Rossi degl’Innocenti, D.; Alfieri, D.; et al. Photobiomodulation of Human Fibroblasts and Keratinocytes with Blue Light: Implications in Wound Healing. Biomedicines 2021, 9, 41.
- Magni, G.; Tatini, F.; Bacci, S.; Paroli, G.; De Siena, G.; Cicchi, R.; Pavone, F.S.; Pini, R.; Rossi, F. Blue LED Light Modulates Inflammatory Infiltrate and Improves the Healing of Superficial Wounds. Photodermatol. Photoimmunol. Photomed. 2020, 36, 166–168.
- Magni, G.; Tatini, F.; Siena, G.D.; Pavone, F.S.; Alfieri, D.; Cicchi, R.; Rossi, M.; Murciano, N.; Paroli, G.; Vannucci, C.; et al. Blue-LED-Light Photobiomodulation of Inflammatory Responses and New Tissue Formation in Mouse-Skin Wounds. Life 2022, 12, 1564.
- Rossi, F.; Tatini, F.; Pini, R.; Bacci, S.; Siena, G.D.; Cicchi, R.; Pavone, F.; Alfieri, D. Improved Wound Healing in Blue LED Treated Superficial Abrasions. In Proceedings of the Medical Laser Applications and Laser-Tissue Interactions VI, Munich, Germany, 12–16 May 2013; SPIE: Munich, Germany, 2013; Volume 8803, pp. 160–164.
- Ablon, G. Phototherapy with Light Emitting Diodes: Treating a Broad Range of Medical and Aesthetic Conditions in Dermatology. J. Clin. Aesthet. Dermatol. 2018, 11, 21–27.
- de Alencar Fernandes Neto, J.; Nonaka, C.F.W.; de Vasconcelos Catão, M.H.C. Effect of Blue LED on the Healing Process of Third-Degree Skin Burns: Clinical and Histological Evaluation. Lasers Med. Sci. 2019, 34, 721–728.
- Orlandi, C.; Purpura, V.; Melandri, D. Blue Led Light in Burns: A New Treatment’s Modality. J. Clin. Investig. Dermatol. 2021, 9, 5.
- Ankri, R.; Friedman, H.; Savion, N.; Kotev-Emeth, S.; Breitbart, H.; Lubart, R. Visible Light Induces Nitric Oxide (NO) Formation in Sperm and Endothelial Cells. Lasers Surg. Med. 2010, 42, 348–352.
- Yang, B.; Chen, Y.; Shi, J. Reactive Oxygen Species (ROS)-Based Nanomedicine. Chem. Rev. 2019, 119, 4881–4985.
- Khoo, V.B.; Soon, S.; Yap, C.J.; Chng, S.P.; Tang, T.Y. Use of Blue Light in the Management of Chronic Venous Ulcer in Asian Patients: A Case Series. Cureus 2021, 13, e17703.
- Gold, M.H.; Sensing, W.; Biron, J.A. Clinical Efficacy of Home-Use Blue-Light Therapy for Mild-to Moderate Acne. J. Cosmet. Laser Ther. 2011, 13, 308–314.
- Dai, T.; Gupta, A.; Murray, C.K.; Vrahas, M.S.; Tegos, G.P.; Hamblin, M.R. Blue Light for Infectious Diseases: Propionibacterium Acnes, Helicobacter Pylori, and Beyond? Drug Resist. Updates 2012, 15, 223–236.
- Weinstabl, A.; Hoff-Lesch, S.; Merk, H.F.; Von Felbert, V. Prospective Randomized Study on the Efficacy of Blue Light in the Treatment of Psoriasis Vulgaris. Dermatology 2011, 223, 251–259.
- Glitzner, E.; Korosec, A.; Brunner, P.M.; Drobits, B.; Amberg, N.; Schonthaler, H.B.; Kopp, T.; Wagner, E.F.; Stingl, G.; Holcmann, M.; et al. Specific Roles for Dendritic Cell Subsets during Initiation and Progression of Psoriasis. EMBO Mol. Med. 2014, 6, 1312–1327.
- Pfaff, S.; Liebmann, J.; Born, M.; Merk, H.F.; von Felbert, V. Prospective Randomized Long-Term Study on the Efficacy and Safety of UV-Free Blue Light for Treating Mild Psoriasis Vulgaris. Dermatology 2015, 231, 24–34.
- Félix Garza, Z.C.; Liebmann, J.; Born, M.; Hilbers, P.A.J.; van Riel, N.A.W. A Dynamic Model for Prediction of Psoriasis Management by Blue Light Irradiation. Front. Physiol. 2017, 8, 28.
- Keemss, K.; Pfaff, S.C.; Born, M.; Liebmann, J.; Merk, H.F.; von Felbert, V. Prospective, Randomized Study on the Efficacy and Safety of Local UV-Free Blue Light Treatment of Eczema. Dermatology 2016, 232, 496–502.
- Szeimies, R.-M.; Dräger, J.; Abels, C.; Landthaler, M. Chapter 1 History of Photodynamic Therapy in Dermatology. In Comprehensive Series in Photosciences; Calzavara-Pinton, P., Szeimies, R.-M., Ortel, B., Eds.; Photodynamic Therapy and Fluorescence Diagnosis in Dermatology; Elsevier: Amsterdam, The Netherlands, 2001; Volume 2, pp. 3–15.
- Kang, K.; Bacci, S. Photodynamic Therapy. Biomedicines 2022, 10, 2701.
- Niculescu, A.-G.; Grumezescu, A.M. Photodynamic Therapy—An Up-to-Date Review. Appl. Sci. 2021, 11, 3626.
- Cappugi, P.; Campolmi, P.; Mavilia, L.; Prignano, F.; Rossi, R. Topical 5-Aminolevulinic Acid and Photodynamic Therapy in Dermatology: A Minireview. J. Chemother. 2001, 13, 494–502.
- Grandi, V.; Bacci, S.; Corsi, A.; Sessa, M.; Puliti, E.; Murciano, N.; Scavone, F.; Cappugi, P.; Pimpinelli, N. ALA-PDT Exerts Beneficial Effects on Chronic Venous Ulcers by Inducing Changes in Inflammatory Microenvironment, Especially through Increased TGF-Beta Release: A Pilot Clinical and Translational Study. Photodiagnosis Photodyn. Ther. 2018, 21, 252–256.
- Vallejo, M.C.S.; Moura, N.M.M.; Ferreira Faustino, M.A.; Almeida, A.; Gonçalves, I.; Serra, V.V.; Neves, M.G.P.M.S. An Insight into the Role of Non-Porphyrinoid Photosensitizers for Skin Wound Healing. Int. J. Mol. Sci. 2020, 22, 234.
- Morton, C.A.; Szeimies, R.-M.; Basset-Seguin, N.; Calzavara-Pinton, P.; Gilaberte, Y.; Haedersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum Guidelines on Topical Photodynamic Therapy 2019 Part 1: Treatment Delivery and Established Indications—Actinic Keratoses, Bowen’s Disease and Basal Cell Carcinomas. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2225–2238.
- Morton, C.A.; Szeimies, R.-M.; Basset-Séguin, N.; Calzavara-Pinton, P.G.; Gilaberte, Y.; Haedersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum Guidelines on Topical Photodynamic Therapy 2019 Part 2: Emerging Indications—Field Cancerization, Photorejuvenation and Inflammatory/Infective Dermatoses. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 17–29.
- Vallejo, M.C.S.; Moura, N.M.M.; Gomes, A.T.P.C.; Joaquinito, A.S.M.; Faustino, M.A.F.; Almeida, A.; Gonçalves, I.; Serra, V.V.; Neves, M.G.P.M.S. The Role of Porphyrinoid Photosensitizers for Skin Wound Healing. Int. J. Mol. Sci. 2021, 22, 4121.
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D.; et al. Photodynamic Therapy of Cancer: An Update. CA Cancer J. Clin. 2011, 61, 250–281.
- Henderson, B.W.; Busch, T.M.; Snyder, J.W. Fluence Rate as a Modulator of PDT Mechanisms. Lasers Surg. Med. 2006, 38, 489–493.
- Peplow, P.V.; Chung, T.-Y.; Baxter, G.D. Photodynamic Modulation of Wound Healing: A Review of Human and Animal Studies. Photomed. Laser Surg. 2012, 30, 118–148.
- Reginato, E.; Wolf, P.; Hamblin, M.R. Immune Response after Photodynamic Therapy Increases Anti-Cancer and Anti-Bacterial Effects. World J. Immunol. 2014, 4, 1–11.
- Corsi, A.; Lecci, P.P.; Bacci, S.; Cappugi, P.; Pimpinelli, N. Early Activation of Fibroblasts during PDT Treatment in Leg Ulcers. G. Ital. Dermatol. Venereol. 2016, 151, 223–229.
- Haensel, D.; Dai, X. Epithelial-to-Mesenchymal Transition in Cutaneous Wound Healing: Where We Are and Where We Are Heading. Dev. Dyn. 2018, 247, 473–480.
- Nesi-Reis, V.; Lera-Nonose, D.S.S.L.; Oyama, J.; Silva-Lalucci, M.P.P.; Demarchi, I.G.; Aristides, S.M.A.; Teixeira, J.J.V.; Silveira, T.G.V.; Lonardoni, M.V.C. Contribution of Photodynamic Therapy in Wound Healing: A Systematic Review. Photodiagnosis Photodyn. Ther. 2018, 21, 294–305.
- Oyama, J.; Fernandes Herculano Ramos-Milaré, Á.C.; Lopes Lera-Nonose, D.S.S.; Nesi-Reis, V.; Galhardo Demarchi, I.; Alessi Aristides, S.M.; Juarez Vieira Teixeira, J.; Gomes Verzignassi Silveira, T.; Campana Lonardoni, M.V. Photodynamic Therapy in Wound Healing in Vivo: A Systematic Review. Photodiagnosis Photodyn. Ther. 2020, 30, 101682.
- Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735.
- Grandi, V.; Corsi, A.; Pimpinelli, N.; Bacci, S. Cellular Mechanisms in Acute and Chronic Wounds after PDT Therapy: An Update. Biomedicines 2022, 10, 1624.
- Steinman, L. Elaborate Interactions between the Immune and Nervous Systems. Nat. Immunol. 2004, 5, 575–581.
- Laverdet, B.; Danigo, A.; Girard, D.; Magy, L.; Demiot, C.; Desmoulière, A. Skin Innervation: Important Roles during Normal and Pathological Cutaneous Repair. Histol. Histopathol. 2015, 30, 875–892.
- Ashrafi, M.; Baguneid, M.; Bayat, A. The Role of Neuromediators and Innervation in Cutaneous Wound Healing. Acta Derm. Venereol. 2016, 96, 587–594.
- Siiskonen, H.; Harvima, I. Mast Cells and Sensory Nerves Contribute to Neurogenic Inflammation and Pruritus in Chronic Skin Inflammation. Front. Cell Neurosci. 2019, 13, 422.
- Grandi, V.; Paroli, G.; Puliti, E.; Bacci, S.; Pimpinelli, N. Single ALA-PDT Irradiation Induces Increase in Mast Cells Degranulation and Neuropeptide Acute Response in Chronic Venous Ulcers: A Pilot Study. Photodiagnosis Photodyn. Ther. 2021, 34, 102222.
- Lee, M.; Rey, K.; Besler, K.; Wang, C.; Choy, J. Immunobiology of Nitric Oxide and Regulation of Inducible Nitric Oxide Synthase. Results Probl. Cell Differ. 2017, 62, 181–207.
- Shi, H.P.; Most, D.; Efron, D.T.; Tantry, U.; Fischel, M.H.; Barbul, A. The Role of iNOS in Wound Healing. Surgery 2001, 130, 225–229.
- Luo, J.; Chen, A.F. Nitric Oxide: A Newly Discovered Function on Wound Healing. Acta Pharmacol. Sin. 2005, 26, 259–264.
- Notari, L.; Nardini, P.; Grandi, V.; Corsi, A.; Pimpinelli, N.; Bacci, S. Neuroimmunomodulation in Chronic Wound Healing after Treatment with Photodynamic Therapy: The Role of iNOs. Med. Sci. Forum 2023, 21, 44.
- Heiskanen, V.; Hamblin, M.R. Correction: Photobiomodulation: Lasers vs. Light Emitting Diodes? Photochem. Photobiol. Sci. 2019, 18, 259.
- Hamblin, M.R. Photobiomodulation or Low-level Laser Therapy. J. Biophotonics 2016, 9, 1122–1124.
- Zhao, F.; Li, Y.; Meng, Z. Successful Treatment of Hyperpigmentation from Fixed Drug Eruption with a Low-dose and Large-spot Q-switched 1064 Nm Nd: YAG Laser. J. Cosmet. Dermatol. 2023, 22, 2128–2130.
- Doppegieter, M.; Van Der Beek, N.; Bakker, E.N.T.P.; Neumann, M.H.A.; Van Bavel, E. Effects of Pulsed Dye Laser Treatment in Psoriasis: A Nerve-wrecking Process? Exp. Dermatol. 2023, 32, 1165–1173.
- Glass, G.E. Photobiomodulation: The Clinical Applications of Low-Level Light Therapy. Aesthetic Surg. J. 2021, 41, 723–738.
- Weiss, R.A.; McDaniel, D.H.; Geronemus, R.G.; Weiss, M.A. Clinical Trial of a Novel Non-thermal LED Array for Reversal of Photoaging: Clinical, Histologic, and Surface Profilometric Results. Lasers Surg. Med. 2005, 36, 85–91.
- Russell, B.A.; Kellett, N.; Reilly, L.R. A Study to Determine the Efficacy of Combination LED Light Therapy (633 Nm and 830 Nm) in Facial Skin Rejuvenation. J. Cosmet. Laser Ther. 2005, 7, 196–200.
- Goldberg, D.J.; Amin, S.; Russell, B.A.; Phelps, R.; Kellett, N.; Reilly, L.A. Combined 633-Nm and 830-Nm Led Treatment of Photoaging Skin. J. Drugs Dermatol. 2006, 5, 748–753.
- Lee, S.Y.; Park, K.-H.; Choi, J.-W.; Kwon, J.-K.; Lee, D.R.; Shin, M.S.; Lee, J.S.; You, C.E.; Park, M.Y. A Prospective, Randomized, Placebo-Controlled, Double-Blinded, and Split-Face Clinical Study on LED Phototherapy for Skin Rejuvenation: Clinical, Profilometric, Histologic, Ultrastructural, and Biochemical Evaluations and Comparison of Three Different Treatment Settings. J. Photochem. Photobiol. B Biol. 2007, 88, 51–67.
- Baez, F.; Reilly, L.R. The Use of Light-emitting Diode Therapy in the Treatment of Photoaged Skin. J. Cosmet. Dermatol. 2007, 6, 189–194.
- Wunsch, A.; Matuschka, K. A Controlled Trial to Determine the Efficacy of Red and Near-Infrared Light Treatment in Patient Satisfaction, Reduction of Fine Lines, Wrinkles, Skin Roughness, and Intradermal Collagen Density Increase. Photomed. Laser Surg. 2014, 32, 93–100.
- Nam, C.H.; Park, B.C.; Kim, M.H.; Choi, E.H.; Hong, S.P. The Efficacy and Safety of 660 Nm and 411 to 777 Nm Light-Emitting Devices for Treating Wrinkles. Dermatol. Surg. 2017, 43, 371–380.
- Mota, L.R.; Duarte, I.D.S.; Galache, T.R.; Pretti, K.M.D.S.; Neto, O.C.; Motta, L.J.; Horliana, A.C.R.T.; Silva, D.D.F.T.D.; Pavani, C. Photobiomodulation Reduces Periocular Wrinkle Volume by 30%: A Randomized Controlled Trial. Photobiomodulation Photomed. Laser Surg. 2023, 41, 48–56.
- Mosca, R.C.; Ong, A.A.; Albasha, O.; Bass, K.; Arany, P. Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach. Adv. Ski. Wound Care 2019, 32, 157–167.
- Chamayou-Robert, C.; DiGiorgio, C.; Brack, O.; Doucet, O. Blue Light Induces DNA Damage in Normal Human Skin Keratinocytes. Photodermatol. Photoimmunol. Photomed. 2022, 38, 69–75.
More
