Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 1 by Giustino Varrassi.
Sacroiliitis is the inflammation of the sacroiliac joint, the largest axial joint in the human body, contributing to 25% of lower back pain cases. It can be detected using various imaging techniques like radiography, Magnetic RIesonance Imaging (MRI), and CTomputed Tomography (CT) scans. Treatments range from conservative methods to invasive procedures. Recent advancements in artificial intelligence offer precise detection of this condition through imaging. Treatment options range from physical therapy and medications to invasive methods like joint injections and surgery.
- sacroiliitis
- MRI
- inflammation
- radiography
1. Introduction
Sacroiliitis is an inflammatory process that affects the sacroiliac joint (SIJ). It may appear acutely or along the course of chronic diseases [1]. The SIJs have an important role in transferring loads between the lumbar spine and the lower limbs and providing support for the upper body [2,3][2][3]. Inflammation and mechanical disfunctions are the two underlying mechanisms for any sacroiliac joint abnormality [3]. It has been reported that 25% of cases of lower back pain is related to the SIJ, of which this pain may stem from various causes such as sacroiliac joint dysfunction (SIJD), stress, pregnancy, trauma, lumbar fusion surgery, bone graft near the sacroiliac joint, and others [3]. The only way to detect structural changes accompanying sacroiliitis is the use of various imaging modalities. Often plain radiography is utilized, especially for its advantageous features. It is considered a safe option, given its low radiation exposure, and it is also cost effective and readily accessible [1]. Concerns have arisen due to its limitation of being a two-dimensional technique to evaluate three-dimensional structures. Therefore, other modalities have been considered such as Computed Tomography (CT) scans, Magnetic Resonance Imaging (MRI), and nuclear medicine scans (bone scans) [4,5,6,7][4][5][6][7].
2. Anatomy of the Sacroiliac Joint
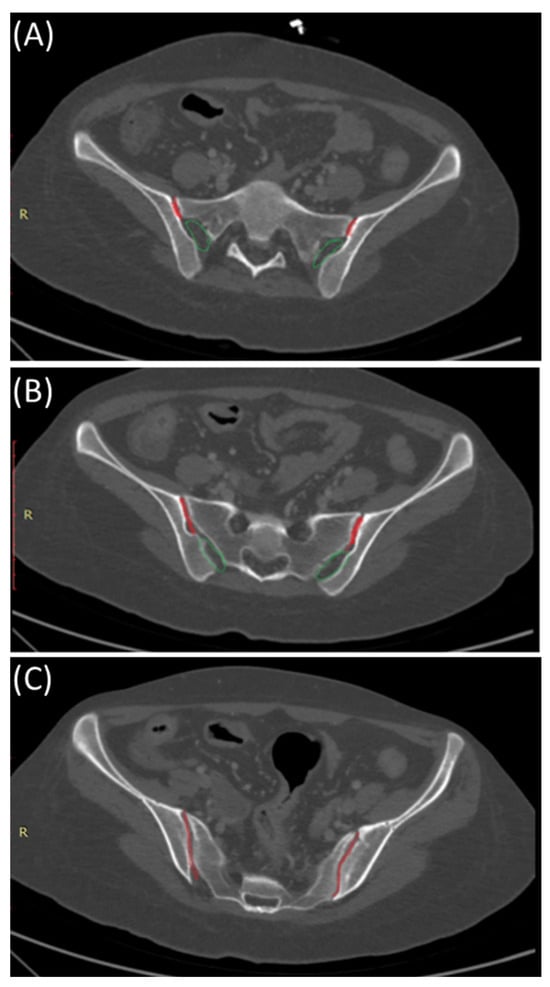
The SIJ is the largest axial joint in the body. It is often described as a C-shaped or an auricular-shaped structure [10,11][8][9]. As shown in Figure 21, the sacroiliac joint is divided into three parts craniocaudally. In the superior part, the posterior portion is syndesmotic up until the very superior section of the anterior part, where the interosseous sacroiliac ligament connects the sacrum and ilium and merges with the posterior sacroiliac ligament. In the middle part, the posterior section is syndesmotic, whereas the anterior part is synovial, and finally, the inferior part of the joint is identified as a true synovial joint [12,13,14][10][11][12]. These ligamentous connections alongside the muscles surrounding the SIJ limit the joint movement and provide stability [11,14][9][12]. There is a wide range of variability in the adult SIJ, including differences in shape and surface contour [14][12].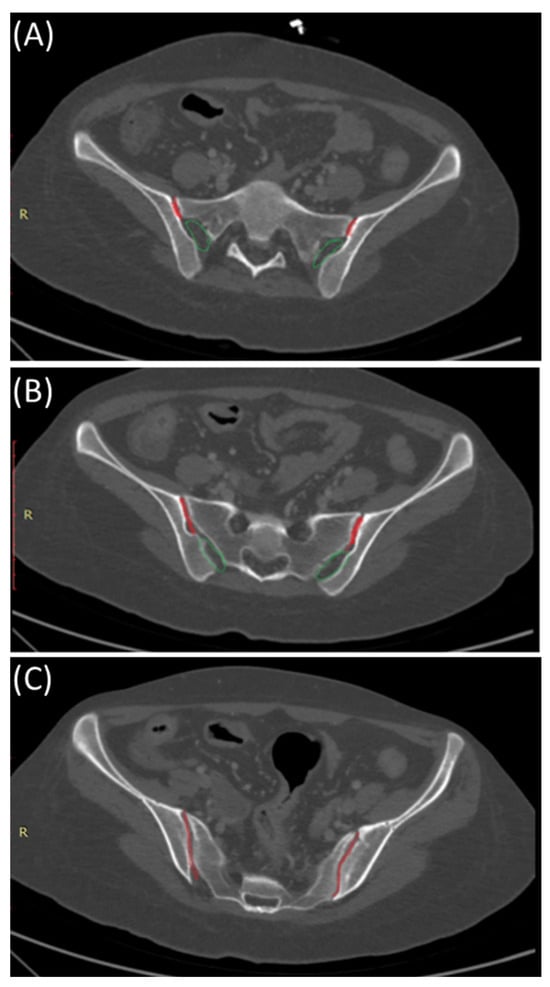
Figure 21. Sacroiliac joint anatomy: Synovial and syndesmotic parts. Axial bone window CT images indicating the position of the synovial (red) and ligamentous (green) components of the sacroiliac joint from cranial (A), mid- (B), and caudal (C) parts of the sacroiliac joints.
3. Clinical Presentation and Etiology of Sacroiliitis
The most common clinical manifestation of sacroiliitis is low back pain, which, generally, affects approximately 70% of individuals at some point in their lives [20][13]. Moreover, SIJ dysfunction is a major cause of chronic low back pain and may account for up to 20% of low back pain complaints in the general population [21][14]. This pain can be unilateral or bilateral, with unilateral pain occurring four times more frequently than bilateral pain [21][14]. The pain in the sacroiliac joint and surrounding structures can manifest itself in various patterns, such as lower back, pelvic, buttock, or sacral pain, as well as discomfort in the groin, posterolateral thigh, and abdomen Additionally, patients may experience acute abdominal pain localized in the lower quadrants and tenderness during rectal examination [22,23][15][16]. Despite the fact that sacroiliitis can manifest in various ways, its presentation is typically classified into acute and chronic [21][14]. Acute sacroiliitis often mimics other conditions and is frequently overlooked during its initial presentation. New-onset severe pain is a significant clinical symptom of acute sacroiliitis. This pain is typically intense and can be disabling for some patients. It intensifies during activities such as running, climbing stairs, or standing up from a seated position, which can hinder their ability to walk, sit, or even shift in bed [21,24,25,26][14][17][18][19]. In the context of acute sacroiliitis, it is widely recognized that pyogenic sacroiliitis is the most frequently reported cause in the medical literature [21][14]. It typically presents unilaterally and often includes symptoms like a high or low-grade fever and intense, persistent pain originating from the affected sacroiliac joint [22,23][15][16]. Proposed factors that may increase the risk of pyogenic sacroiliitis encompass intravenous drug use, infections, especially those originating from skin tissues and infective endocarditis, as well as pregnancy [22,28][15][20]. Another worth-noting entity is acute brucellar sacroiliitis, which is clinically similar to pyogenic sacroiliitis. Bilateral involvement of the sacroiliac joints may be observed in up to 25% of patients. Additionally, healthcare providers should not overlook concomitant clinical signs indicative of brucellosis, such as fever, sweating, malaise, and hepatosplenomegaly [21][14]. SIJ aspiration, guided by ultrasound or CT, is a diagnostic procedure that plays a crucial role in evaluating acute sacroiliitis, particularly when septic or crystal-induced causes are under consideration [13][11]. The procedure is indicated when there is suspicion of septic sacroiliitis, as it allows for the collection of synovial fluid from the joint for microbiological analysis [30][21]. This analysis is instrumental in identifying the causative infectious agent, guiding the selection of appropriate antibiotic therapy [30][21]. Both ultrasound and CT can be employed to guide the needle placement during SIJ aspiration [13][11]. Ultrasound provides real-time imaging, particularly advantageous for visualizing soft tissues [32][22], while CT offers detailed cross-sectional images, valuable in certain clinical contexts [33][23]. The patient is positioned lying down, and local anesthesia is administered to minimize discomfort. Under the guidance of ultrasound or CT, a thin needle is carefully advanced into the sacroiliac joint space and synovial fluid is aspirated [34][24]. Dual-energy-computed tomography (DECT) emerges as a pivotal diagnostic tool in the comprehensive evaluation of sacroiliitis [35][25]. Its dual-energy approach enhances sensitivity, enabling the detection of subtle inflammatory changes such as bone marrow edema and synovial enhancement [36][26]. The aspirated synovial fluid is then subjected to laboratory analysis [39][27]. In cases of septic sacroiliitis, microbiological cultures are performed to identify the infectious organism [39][27]. For crystal-induced sacroiliitis, the fluid is examined for the presence of crystals, such as monosodium urate or calcium pyrophosphate crystals [40][28]. Positive findings in the synovial fluid analysis confirm the diagnosis of septic or crystal-induced sacroiliitis, providing critical information for targeted and effective treatment [41][29].4. Radiological Findings and Imaging Modalities
4.1. Plain Radiographs
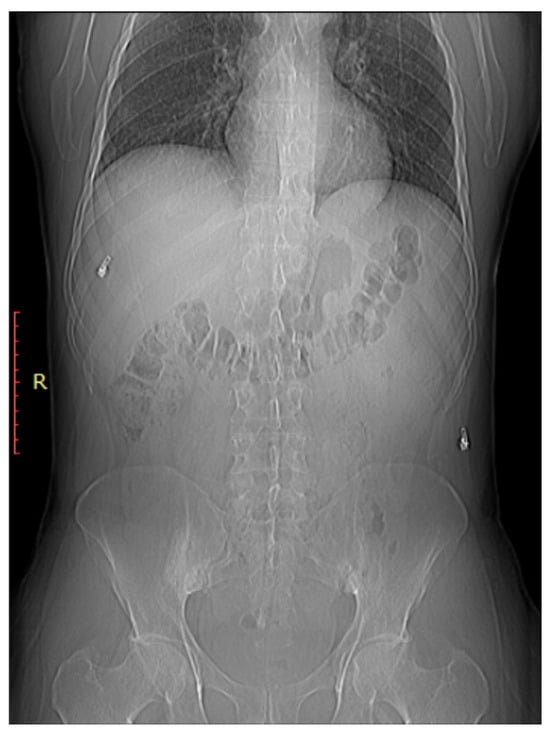
As shown in Figure 21, early sacroiliitis may show subtle erosions at the joint margins [44][30]. These erosions are typically irregular and may appear as small, well-defined areas of bone loss [44][30]. As the inflammation progresses, the joint may become more sclerotic, leading to increased bone density in the SI joint [45][31]. Progressive inflammation can lead to narrowing of the SIJ space, indicating joint damage and dysfunction As shown in Figure 32, early sacroiliitis may show subtle erosions at the joint margins [44][30]. These erosions are typically irregular and may appear as small, well-defined areas of bone loss [44][30]. As the inflammation progresses, the joint may become more sclerotic, leading to increased bone density in the SI joint [45][31]. Progressive inflammation can lead to narrowing of the SIJ space, indicating joint damage and dysfunction [1]. In addition, changes in the subchondral bone, including irregularities, sclerosis, and erosions, are common features of sacroiliitis [46][32].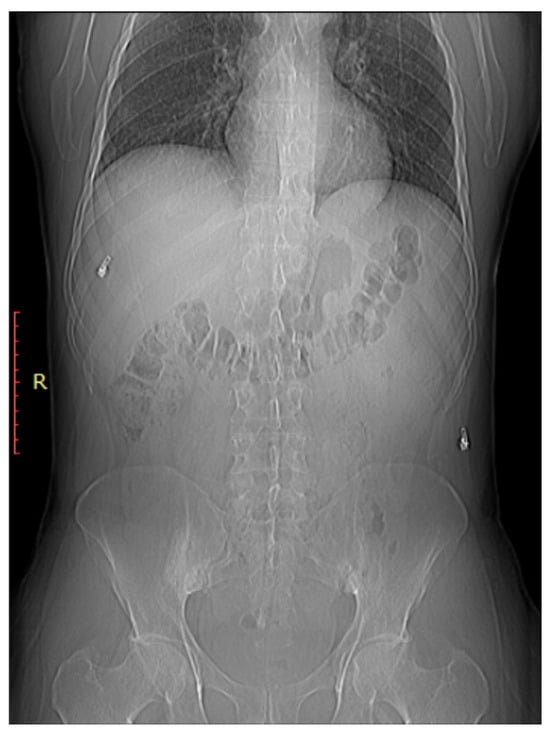
Figure 32. Bilateral sacroiliitis. X-ray for a 41-year-old male presenting with Rt sciatica showing irregularity and sclerosis of both sacroiliac joints is more evident on the right.
4.2. Computed Tomography
CT scans provide more detailed images of the sacroiliac joint and can reveal erosions, sclerosis, and joint space narrowing with greater clarity than X-rays [13][11]. Severe sacroiliitis, particularly in cases of ankylosing spondylitis, can lead to complete fusion or ankylosis of the sacroiliac joint [4]. CT scans can demonstrate the fusion as a solid, bony bridge between the sacrum and ilium [4]. CT scans can also assess soft tissues surrounding the SIJ, such as ligaments, tendons, and muscles, which may be inflamed in cases of sacroiliitis [44][30] as demonstrated in Figure 43 and Figure 54.
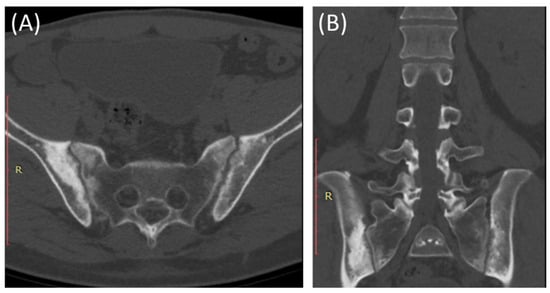
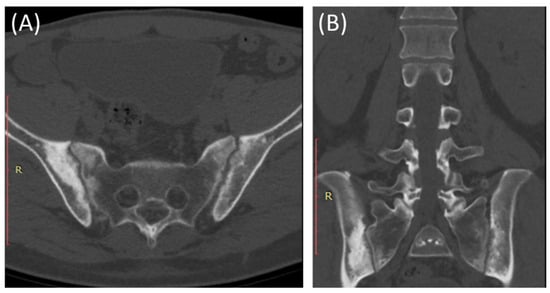
Figure 43. Axial bone window CT scan (A) and coronal bone window CT scan (B) for a 41-year-old male presenting with Rt sciatica suggestive of bilateral sacroiliitis (same Patient as in Figure 32).
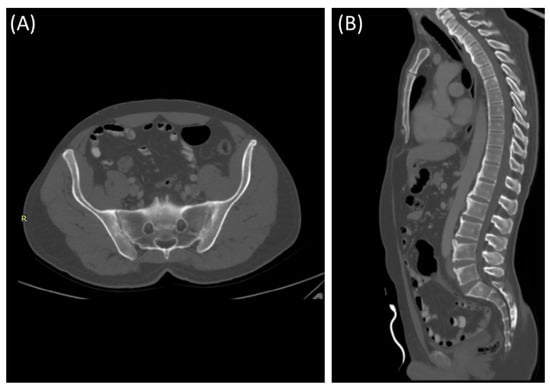
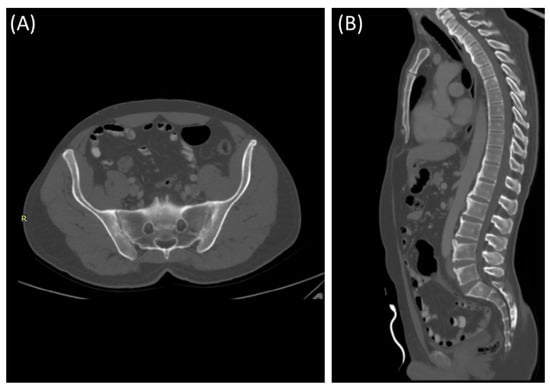
Figure 54. Axial bone window CT scan (A) showing Chronic sacroiliitis with ankyloses of the sacroiliac and a sagittal bone window CT scan (B) showing Syndesmophytes in the spine in a 55-year-old patient with Ankylosing spondylitis.
4.3. Magnetic Resonance Imaging
MRI is considered the gold standard for the diagnosis of sacroiliitis, especially in early and inflammatory stages [5]. It provides valuable information for diagnosing and monitoring the condition, assessing disease activity, and guiding treatment decisions [5].
As demonstrated in Figure 43, MRI is particularly sensitive in detecting active inflammation [44][30]. In sacroiliitis, MRI often reveals edema (swelling) and increased signal intensity on T2-weighted images within and around the SIJ [13][11]. This edema is indicative of active inflammation and is a hallmark feature [13][11].
MRI can reveal soft tissue changes, including inflammation of the ligaments and tendons around the SIJ [50][33]. Enthesitis, which is the inflammation of the insertion points of ligaments and tendons into bone, is a common finding in sacroiliitis and can be visualized [53][34]. Furthermore, a contrast agent (gadolinium) may be used to enhance areas of active inflammation, making them more visible [54][35]. In advanced cases, particularly in ankylosing spondylitis (Figure 65), MRI may show evidence of joint ankylosis, where the sacroiliac joint becomes fused [44][30].
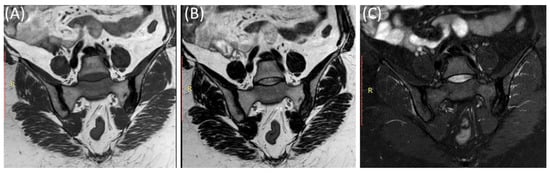
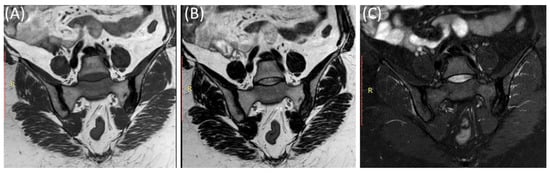
Figure 65. Coronal T1-WI image (A), coronal T2-WI image (B) and coronal T2-fat suppression image (C) showing sclerosis and mild irregularity in both sacroiliac joints, more on the left side with no evident bone marrow edema in a 52-year-old female with chronic low back and hip pain suggestive of bilateral chronic sacroiliitis.
4.4. Nuclear Medicine—Bone Scans
Nuclear medicine scans (bone scans) can also play a role in the evaluation of sacroiliitis, particularly in detecting active inflammation and assessing disease activity and inflammatory changes earlier than conventional X-rays [6,7][6][7].
As provided in Figure 86, one of the most commonly used nuclear medicine scans for sacroiliitis is the Technetium-99m bone scan [6]. This tracer is taken up by bone tissue in areas of increased metabolic activity [6]. In sacroiliitis, areas of active inflammation and increased bone turnover will absorb more of the radioactive tracer, leading to “hot spots” on the scan [63][36]. A bone scan can provide information about the extent and distribution of inflammation in the sacroiliac joints and other areas of the body, if applicable [64][37]. It is particularly useful for detecting active inflammation and assessing the overall disease activity in sacroiliitis [6].
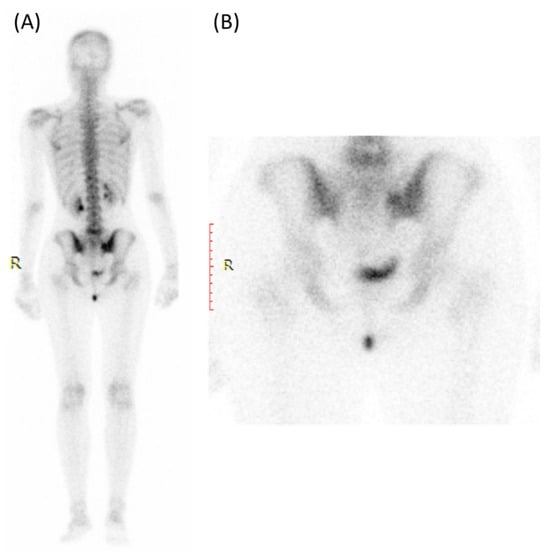
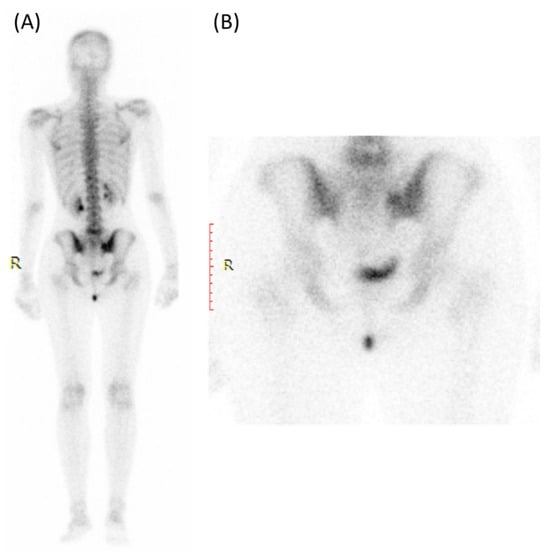
Figure 86. Bone scan (using Tc99m HDP) for a 30-year-old female presented with Lt hip pain showing focal increased tracer uptake in the Lt sacroiliac joint in the blood pool (A) and delayed images (B).
5. Radiological Criteria and Scoring Systems
Sacroiliitis is graded using plain films based on the Modified New York Criteria in which the sacroiliac joint is observed and graded as one of five different grades. Grade 0 is given to a normal sacroiliac joint; Grade 1 is given if there is observed suspicion (blurriness surrounding the margins of the joint); Grade 2 if there are small abnormalities, including restricted sclerosis or erosions; Grade 3 if there are explicit and extensive anomalies including changes in the width of the joint, and a significant number of erosions; finally, Grade 4 would be given if complete ankylosis is observed. It is worth mentioning that the diagnosis of sacroiliitis depends on its laterality.
The Spondyloarthritis Research Consortium Canada (SPARCC) MR-based scoring system relied on T2-weighted images, as inflammation-induced edema around the marrow might not be visible in other phases, and fat signal suppression in the marrow can be seen in T2 as well [68][38]. Each sacroiliac joint was divided into four quadrants, giving one point to every quadrant demonstrating an increased STIR signal [68][38]. An additional point would be given for any joint demonstrating an intense signal, and another for a continuous signal that is more than one centimeter in depth [68][38]. This is then applied to six coronal slices [68][38]. Each slice would have 12 points maximum, and the total amount of points for all six slices would be 72 points [68][38].
Other MR-based scoring systems include MR Imaging of Seronegative SpA (MISS), Leeds, Aarhus, a system proposed by Sieper and Rudwaleit, and another by Hermann and Bollow when applying the Outcome Measures in Rheumatology (OMERACT) filter on mentioned scoring systems, where 52% voted that sacroiliac joint MRI could serve as a valuable measure to be used in pharmaceutical clinical trials, while only 30% agreed that they are valuable in evaluating chronic changes for spine and sacroiliac assessment.
6. Management of Sacroiliitis
A patient with sacroiliitis should be approached by first identifying and addressing potential contributing factors, including hip osteoarthritis, kyphosis, scoliosis, leg length discrepancy, and osteoporosis. Subsequently, education and management can be initiated via a home exercise program, activity modification, and physical therapy. Lastly, pain management can be considered to maintain and facilitate activity, either via pharmacological interventions or complementary and alternative modalities (CAM) [70][39]. After 6 weeks, if a reduction in pain of approximately 30 percent and an improvement in function are observed, the used treatment and self-assessment plan should be continued. If not, the option of escalating pharmacological therapy or discussing the possibility of sacroiliac joint or periarticular corticosteroid injection with the patient, provided there are no contraindications, should be considered. If an improvement with local corticosteroids and local anesthesia is not sustained for 3 months, consideration can be given to discussing an alternative treatment plan, such as denervation, unless it is declined by the patient. In the event of the patient declining this option, a reevaluation of CAM and a stepped-care drug assessment for sacroiliac joint pain should be contemplated. If pain relief is not attained with local analgesia and corticosteroid injections, a reevaluation of the stepped-care drug assessment and CAM should be undertaken. If improvement still does not occur, a reconsideration of injection pathways or a referral to an interdisciplinary pain rehabilitation program may be warranted [70][39].References
- Baronio, M.; Sadia, H.; Paolacci, S.; Prestamburgo, D.; Miotti, D.; Guardamagna, V.A.; Natalini, G.; Bertelli, M. Etiopathogenesis of sacroiliitis: Implications for assessment and management. Korean J. Pain. 2020, 33, 294–304.
- Vleeming, A.; Schuenke, M.D.; Masi, A.T.; Carreiro, J.E.; Danneels, L.; Willard, F.H. The sacroiliac joint: An overview of its anatomy, function and potential clinical implications. J. Anat. 2012, 221, 537–567.
- Lee, A.; Gupta, M.; Boyinepally, K.; Stokey, P.J.; Ebraheim, N.A. Sacroiliitis: A Review on Anatomy, Diagnosis, and Treatment. Adv. Orthop. 2022, 2022, 3283296.
- Canella, C.; Schau, B.; Ribeiro, E.; Sbaffi, B.; Marchiori, E. MRI in Seronegative Spondyloarthritis: Imaging Features and Differential Diagnosis in the Spine and Sacroiliac Joints. Am. J. Roentgenol. 2013, 200, 149–157.
- Triantafyllou, M.; Klontzas, M.E.; Koltsakis, E.; Papakosta, V.; Spanakis, K.; Karantanas, A.H. Radiomics for the Detection of Active Sacroiliitis Using MR Imaging. Diagnostics 2023, 13, 2587.
- Zilber, K.; Gorenberg, M.; Rimar, D.; Boulman, N.; Kaly, L.; Rozenbaum, M.; Rosner, I.; Slobodin, G. Radionuclide Methods in the Diagnosis of Sacroiliitis in Patients with Spondyloarthritis: An Update. Rambam Maimonides Med. J. 2016, 7, e0037.
- Hemke, R.; Herregods, N.; Jaremko, J.L.; Åström, G.; Avenarius, D.; Becce, F.; Bielecki, D.K.; Boesen, M.; Dalili, D.; Giraudo, C.; et al. Imaging assessment of children presenting with suspected or known juvenile idiopathic arthritis: ESSR-ESPR points to consider. Eur. Radiol. 2020, 30, 5237–5249.
- Calvillo, O.; Skaribas, I.; Turnipseed, J. Anatomy and pathophysiology of the sacroiliac joint. Curr. Rev. Pain. 2000, 4, 356–361.
- Gartenberg, A.; Nessim, A.; Cho, W. Sacroiliac joint dysfunction: Pathophysiology, diagnosis, and treatment. Eur. Spine J. 2021, 30, 2936–2943.
- Navallas, M.; Ares, J.; Beltrán, B.; Lisbona, M.P.; Maymó, J.; Solano, A. Sacroiliitis associated with axial spondyloarthropathy: New concepts and latest trends. Radiographics 2013, 33, 933–956.
- Tsoi, C.; Griffith, J.F.; Lee, R.K.L.; Wong, P.C.H.; Tam, L.S. Imaging of sacroiliitis: Current status, limitations and pitfalls. Quant. Imaging Med. Surg. 2019, 9, 318–335.
- Cohen, S.P. Sacroiliac joint pain: A comprehensive review of anatomy, diagnosis, and treatment. Anesth. Analg. 2005, 101, 1440–1453.
- Kennedy, D.J.; Engel, A.; Kreiner, D.S.; Nampiaparampil, D.; Duszynski, B.; MacVicar, J. Fluoroscopically Guided Diagnostic and Therapeutic Intra-Articular Sacroiliac Joint Injections: A Systematic Review. Pain. Med. 2015, 16, 1500–1518.
- Slobodin, G.; Rimar, D.; Boulman, N.; Kaly, L.; Rozenbaum, M.; Rosner, I.; Odeh, M. Acute sacroiliitis. Clin. Rheumatol. 2016, 35, 851–856.
- Vyskocil, J.J.; McIlroy, M.A.; Brennan, T.A.; Wilson, F.M. Pyogenic infection of the sacroiliac joint. Case reports and review of the literature. Medicine 1991, 70, 188–197.
- Cohn, S.M.; Schoetz, D.J., Jr. Pyogenic sacroiliitis: Another imitator of the acute abdomen. Surgery 1986, 100, 95–98.
- Cohen, S.P.; Chen, Y.; Neufeld, N.J. Sacroiliac joint pain: A comprehensive review of epidemiology, diagnosis and treatment. Expert. Rev. Neurother. 2013, 13, 99–116.
- Prather, H. Sacroiliac joint pain: Practical management. Clin. J. Sport. Med. 2003, 13, 252–255.
- Zelle, B.A.; Gruen, G.S.; Brown, S.; George, S. Sacroiliac joint dysfunction: Evaluation and management. Clin. J. Pain. 2005, 21, 446–455.
- Kurnutala, L.N.; Ghatol, D.; Upadhyay, A. Clostridium Sacroiliitis (Gas Gangrene) Following Sacroiliac Joint Injection--Case Report and Review of the Literature. Pain. Physician 2015, 18, E629–E632.
- Horowitz, D.L.; Katzap, E.; Horowitz, S.; Barilla-LaBarca, M.L. Approach to septic arthritis. Am. Fam. Physician 2011, 84, 653–660.
- Carovac, A.; Smajlovic, F.; Junuzovic, D. Application of ultrasound in medicine. Acta Inf. Med. 2011, 19, 168–171.
- Berger, M.; Müller, K.; Aichert, A.; Unberath, M.; Thies, J.; Choi, J.H.; Fahrig, R.; Maier, A. Marker-free motion correction in weight-bearing cone-beam CT of the knee joint. Med. Phys. 2016, 43, 1235–1248.
- Raza, K.; Lee, C.Y.; Pilling, D.; Heaton, S.; Situnayake, R.D.; Carruthers, D.M.; Buckley, C.D.; Gordon, C.; Salmon, M. Ultrasound guidance allows accurate needle placement and aspiration from small joints in patients with early inflammatory arthritis. Rheumatology 2003, 42, 976–979.
- Carotti, M.; Benfaremo, D.; Di Carlo, M.; Ceccarelli, L.; Luchetti, M.M.; Piccinni, P.; Giovagnoni, A.; Salaffi, F. Dual-energy computed tomography for the detection of sacroiliac joints bone marrow oedema in patients with axial spondyloarthritis. Clin. Exp. Rheumatol. 2021, 39, 1316–1323.
- Sanghavi, P.S.; Jankharia, B.G. Applications of dual energy CT in clinical practice: A pictorial essay. Indian J. Radiol. Imaging 2019, 29, 289–298.
- Mathews, C.J.; Kingsley, G.; Field, M.; Jones, A.; Weston, V.C.; Phillips, M.; Walker, D.; Coakley, G. Management of septic arthritis: A systematic review. Ann. Rheum. Dis. 2007, 66, 440–445.
- Zell, M.; Zhang, D.; FitzGerald, J. Diagnostic advances in synovial fluid analysis and radiographic identification for crystalline arthritis. Curr. Opin. Rheumatol. 2019, 31, 134–143.
- Zahar, A.; Lausmann, C.; Cavalheiro, C.; Dhamangaonkar, A.C.; Bonanzinga, T.; Gehrke, T.; Citak, M. How Reliable Is the Cell Count Analysis in the Diagnosis of Prosthetic Joint Infection? J. Arthroplast. 2018, 33, 3257–3262.
- Sudoł-Szopinska, I.; Urbanik, A. Diagnostic imaging of sacroiliac joints and the spine in the course of spondyloarthropathies. Pol. J. Radiol. 2013, 78, 43–49.
- Al-Zaghal, A.; Yellanki, D.P.; Kothekar, E.; Werner, T.J.; Høilund-Carlsen, P.F.; Alavi, A. Sacroiliac Joint Asymmetry Regarding Inflammation and Bone Turnover: Assessment by FDG and NaF PET/CT. Asia Ocean. J. Nucl. Med. Biol. 2019, 7, 108–114.
- Pialat, J.B.; Di Marco, L.; Feydy, A.; Peyron, C.; Porta, B.; Himpens, P.H.; Ltaief-Boudrigua, A.; Aubry, S. Sacroiliac joints imaging in axial spondyloarthritis. Diagn. Interv. Imaging 2016, 97, 697–708.
- Wagle, S.; Gu, J.T.; Courtier, J.L.; Phelps, A.S.; Lin, C.; MacKenzie, J.D. Value of dedicated small-field-of-view sacroiliac versus large-field-of-view pelvic magnetic resonance imaging for evaluating pediatric sacroiliitis. Pediatr. Radiol. 2019, 49, 933–940.
- Kehl, A.S.; Corr, M.; Weisman, M.H. Review: Enthesitis: New Insights Into Pathogenesis, Diagnostic Modalities, and Treatment. Arthritis Rheumatol. 2016, 68, 312–322.
- Kinno, M.; Sutter, J. Gadolinium-Based Contrast Agents. In Magnetic Resonance Imaging of Congenital Heart Disease; Syed, M.A., Mohiaddin, R.H., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 51–57.
- Van den Wyngaert, T.; Strobel, K.; Kampen, W.U.; Kuwert, T.; van der Bruggen, W.; Mohan, H.K.; Gnanasegaran, G.; Delgado-Bolton, R.; Weber, W.A.; Beheshti, M.; et al. The EANM practice guidelines for bone scintigraphy. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1723–1738.
- Koç, Z.P.; Kin Cengiz, A.; Aydın, F.; Samancı, N.; Yazısız, V.; Koca, S.S.; Karayalçın, B. Sacroiliac indicis increase the specificity of bone scintigraphy in the diagnosis of sacroiliitis. Mol. Imaging Radionucl. Ther. 2015, 24, 8–14.
- Maksymowych, W.P.; Inman, R.D.; Salonen, D.; Dhillon, S.S.; Williams, M.; Stone, M.; Conner-Spady, B.; Palsat, J.; Lambert, R.G. Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. Arthritis Rheum. 2005, 53, 703–709.
- Polsunas, P.J.; Sowa, G.; Fritz, J.M.; Gentili, A.; Morone, N.E.; Raja, S.N.; Rodriguez, E.; Schmader, K.; Scholten, J.D.; Weiner, D.K. Deconstructing Chronic Low Back Pain in the Older Adult—Step by Step Evidence and Expert-Based Recommendations for Evaluation and Treatment: Part X: Sacroiliac Joint Syndrome. Pain. Med. 2016, 17, 1638–1647.
More
