You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 1 by Daniel Burkett.
The origins of endoscopic spine surgery can be traced back many decades, with many important innovations throughout its development. It can be applied to all levels of the spine, with many robust trials supporting its clinical outcomes. Continued clinical research is needed to explore its expanding indications.
- endoscopic spine surgery
- spine
- endoscopy
- navigation
- endoscope
1. Brief History of Endoscopic Spine Surgery
Approaches for the surgical management of spinal pathology, including disc herniations and spinal stenosis, have evolved significantly since the first lumbar discectomy was described in 1908 [1]. The effort to develop minimally invasive tools and techniques to minimize tissue damage and improve visualization has evolved throughout the history of modern surgery [2]. The evolution of open un-magnified surgery to microscopic surgery has progressed over the last century. Endoscopic approaches in spine surgery represent an advancement of these techniques. Endoscopes such as laparoscopes and cystoscopes have been used consistently in general surgery, urology, and otolaryngology. The utilization of endoscopes for spine surgery has been a more recent development in the latter half of the last century.
The origins of endoscopic approaches to the spine can be traced back to Hijikata and Kambin in the 1970s. Parviz Kambin demonstrated a percutaneous approach for a lateral discectomy using a cannula in 1973. In 1974, Hijikata developed and used tubes to obtain posterolateral access to lumbar disc spaces. He coined this procedure a “percutaneous nucleotomy” [3]. These approaches at the time did not allow for the direct visualization of the spinal canal. The idea of endoscopic direct visualization was applied using a modified arthroscope by Forst and Hausman in the 1980s and later by Kambin using an endoscope. Kambin described a safe anatomical triangular working zone for endoscopic approaches in 1990 [4].
A fully functional endoscopic system (visualization, tissue manipulation, and resection) was used by Anthony Yeung in the 1990s for endoscopic transforaminal approaches [5]. This system used a multichannel, wide-angled endoscope with continuous saline irrigation and underwater bipolar dissection. Multiple endoscopic systems were being developed and utilized in several countries at that time. A description of the successful treatment of far lateral herniated discs using an endoscope through a tubular retractor was published in 1999 by Kevin Foley et al. [6]. A transforaminal approach using bone reamers to open the foraminal window was described in 2005 by Michael Schubert and Thomas Hoogland [7]. In the early 2000s, Sebastian Ruetten applied the technology to interlaminar endoscopic approaches [1].
The continued development of endoscopic techniques has included the use of two separate channels, one working channel and one for the endoscope. This technique is generally termed endoscope-assisted surgery or the unilateral biportal endoscopic (UBE) technique. In 1996, De Antoni described a UBE technique [8]. In addition to an interlaminar approach, a biportal extraforaminal endoscopic approach has also been described [9]. The UBE technique has been supported by good surgical results for the treatment of lumbar stenosis and disc herniation [10].
Today, endoscopic spinal surgery continues to make advances in equipment, techniques, and in the applications of its use. The development of endoscopic spine surgery has advanced significantly for the treatment of many spinal pathologies, but challenges to its widespread adoption remain.
2. Endoscope and Instrument Technology
Endoscope systems typically consist of a 20–30 degree rod-lens camera system with a light source, a working channel, and an irrigation channel. Higher-degree scopes are sometimes used for acute working angles such as in the thoracic spine. The interlaminar approach for lumbar discectomy was first performed with a micro endoscopic system in the late 1990s. That endoscope had an outer diameter of 6 mm and a working channel of 2.7 mm. The next generation of endoscopes to follow had an outer diameter of 7.9 mm and a 4.2 mm working channel size. The working channel was large enough to allow the use of endoscopic burrs and punches. The introduction of these instruments allowed surgeons to perform bone resection. The ability to perform bone work under endoscopic visualization expanded the number of pathologies that could be treated [11]. In 2007, the use of these instruments was shown to be effective for the removal of migrated discs [12]. Ruetten later used a 4 mm burr to perform lumbar lateral recess decompression [13].
The third generation of endoscopes had an outer diameter of 9.5 mm and a working channel diameter of 5.6 mm. The increase in the working channel size allowed expanded bony resection and more efficient laminotomies.
The current generation of endoscopes has various endoscopic burrs at their disposal. These burrs have gradually increased in diameter to a working size of 4.5–5.5 mm and include articulating burrs that allow angled drilling. The flexible burrs in conjunction with angled endoscopes allow drilling outside the trajectory of the endoscope working channel. These flexible burrs have demonstrated efficiency when performing endoscopic central canal decompression [14]. Articulating burrs also provide the ability to drill calcified discs in difficult anatomical locations such as the thoracic spine [15]. Curved or angled Kerrison bony punches allow additional wide bony removal. The advancement of endoscopic tools has continued to improve the efficiency of these approaches.
3. Current Techniques
3.1. Transforaminal Approach
The endoscopic transforaminal approach is the most traditional uniportal method used in endoscopic spine surgery (ESS) (Figure 1). This approach can be successfully used for the initial treatment of foraminal disc herniations and foraminal stenosis [16]. It is also an option for revision surgeries when trying to avoid a repeat posterior approach. Studies have shown that transforaminal endoscopic surgery and open microscopic surgery did not have significant differences in reoperation and complication rates, but there was less postoperative back pain and a shorter hospital stay in the endoscopic surgery group [17]. An RCT of 143 patients demonstrated that the transforaminal endoscopic discectomy (TED) group had lower affected side leg pain at 2 years compared to the microdiscectomy group. In addition, hospital stays were significantly shorter in the TED group [18]. The anatomical limitations to this approach include the facet joint, pedicle, and the exiting nerve root that can vary with different pathologies.
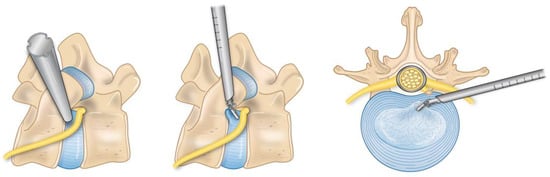
Figure 1.
This is a depiction of the foraminal anatomy involved in an endoscopic transforaminal approach.
3.2. Lumbar Interlaminar Approach
Sometimes described as the second generation of lumbar endoscopic spine surgery, the interlaminar approach provides more flexibility to an endoscopic spine surgeon’s repertoire (Figure 2). This technique allows the treatment of central and lateral recess canal stenosis and specifically the treatment of L5/S1 disc herniations due to the anatomic constraints of the iliac crest at that level. A meta-analysis reported better results with interlaminar endoscopic lumbar discectomy than transforaminal endoscopic lumbar discectomy in L5/S1 disc herniations [19].

Figure 2.
Illustration of the lumbar interlaminar approach.
The advantage with the endoscopic interlaminar approach is that the anatomical landmarks are similar to microscopic and traditional anatomic approaches. Additionally, the procedure can more easily be converted to an open operation if needed. Finally, it conserves bony anatomy compared to open surgery, specifically the facet joints. A randomized controlled trial demonstrated similar recovery rates of symptoms between endoscopic and microscopic interlaminar decompression for lateral recess stenosis but found lower rates of revisions and complications with the endoscope [13]. Multiple studies have shown similar decompression, improved clinical outcomes, and shorter hospital stays with endoscopic techniques compared to conventional MIS tubular surgery. These have shown good improvements in Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) scores postoperatively [17,20][17][20].
Endoscopic approaches to the lumbar spine have also been argued to serve as treatments for significant central stenosis due to less paraspinal muscle damage and bone resection but sufficient postoperative central decompression. These results are comparable to open surgery for the treatment of multiple levels of lumbar stenosis [21,22][21][22].
3.3. Cervical Spine Approach
Endoscopic techniques can be used to address both anterior and posterior cervical pathologies and minimize spinal cord manipulation and muscle dissection. Endoscopic posterior cervical foraminotomy is a successful technique for lateral and foraminal disc herniations and has a high success rate of radiculopathy resolution without serious surgical complications [23] (Figure 3). Endoscopic visualization also allows a view of the intervertebral disc not normally seen with conventional open or tubular approaches. After the foraminotomy is performed, the endoscope can be manipulated around the nerve root to remove any parts of the disc causing compression. An RCT showed that endoscopic posterior cervical foraminotomies had similar outcomes to conventional anterior cervical discectomy and fusion (ACDF) [24]. That study noted that the full endoscopic technique had an advantage because it does not require the implantation of hardware. Compared to open foraminotomy, endoscopic surgery also has the advantage of less blood loss, shorter operative times, and shorter lengths of hospital stays [25].
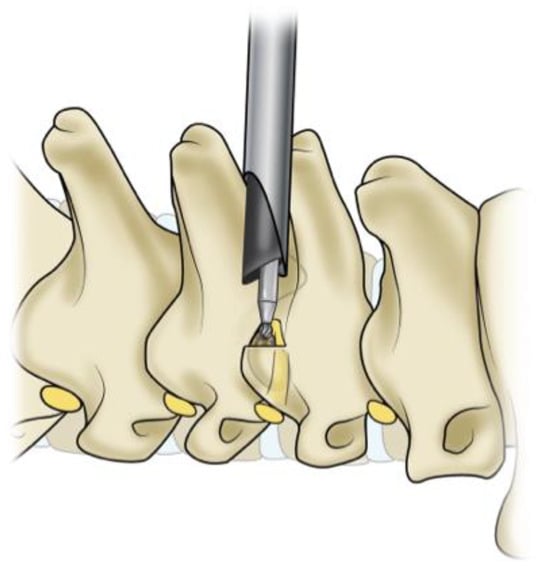
Figure 3.
This is an illustration of the posterior cervical foraminotomy approach.
Full endoscopic bilateral decompression for cervical stenosis has been described. Carr et al. reported their first 10 cases with the technique and demonstrated improvement in postoperative Nurick grades and modified Japanese Orthopaedic Association scores without any permanent neurologic complications [26]. Biportal endoscopic laminectomy for the treatment of cervical myelopathy has also been demonstrated and is gaining favor [27]. Full endoscopic and endoscopic-assisted posterior cervical lateral mass screw fixation, C1–2 screw fixation, and laminoplasty procedures have been described without sufficient reports of clinical results.
Long-term clinical results comparing full endoscopic ACDF to conventional ACDF are still needed. Full endoscopic anterior cervical discectomy without fusion in select patients with soft disc herniations, unilateral radiculopathy, and central disc herniations has demonstrated good clinical outcomes [28]. This has been shown to have comparable results with conventional ACDF surgery after a 5-year follow up [29].
3.4. Thoracic Spine Approach
Conventional thoracic approaches require extensive muscle dissection and bony resection. Endoscopic approaches allow surgeons to address thoracic disc and spinal canal pathologies directly without significantly disrupting surrounding tissue. Endoscopic transforaminal thoracic discectomy for the treatment of soft disc herniations has demonstrated clinical improvements in VAS and ODI scores after a 5-year follow up [30]. Endoscopic interlaminar, extraforaminal, and transthoracic retropleural approaches for the treatment of disc herniations and thoracic stenosis have shown sufficient spinal cord decompression and successful clinical results [31,32][31][32]. The extraforaminal group had a significantly lower complication rate. The treatment of calcified disc herniations via endoscopic approaches has limited data, but these procedures have been performed. Unilateral biportal endoscopic techniques for thoracic fusion surgery have also been described [33]. The same surgical risks and challenges that occur with open thoracic approaches can also challenge endoscopic approaches if the approach is not accurate. This includes injury to the vasculature, lungs, ribs, and postoperative neurological deficits [30].
3.5. Lumbar Interbody Fusion
Endoscopic lumbar interbody fusion is gaining favor due to the small incision size and quick postoperative recovery. The approach angle is similar to the current minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) technique. The instruments are docked and ipsilateral facetectomy and laminotomy are performed. This is then followed by discectomy, endplate preparation, and interbody cage placement [34]. Current indications for endoscopic TLIF are for patients with unilateral foraminal stenosis and mild central stenosis [35]. Other endoscopic TLIF techniques avoid removing the ipsilateral facet altogether in patients who will improve with just indirect decompression [36]. Biportal endoscopic TLIF has shown no significant differences in clinical outcomes compared to conventional MIS-TLIF [37,38][37][38]. There are also no reported differences in early and midterm fusion rates between biportal and uniportal endoscopic fusion [39].
In patients with bilateral foraminal stenosis, severe central stenosis, or high-grade spondylolisthesis, unilateral endoscopic lumbar interbody fusion may have limited utility [40]. Endoscopic TLIF has shown promising results, but further long-term studies are needed.
3.6. Uniportal and Biportal Approaches
Biportal endoscopy involves the use of an endoscope portal and a working portal. The two channels are placed according to surgeon preference centered on the surgical pathology. A retrospective study compared unilateral biportal endoscopic (UBE) discectomy to open microdiscectomy, and they showed similar results in postoperative pain control, leg pain, and functional disability. UBE had less operative blood loss, shorter hospital stays, and better immediate postoperative back pain [41]. A randomized controlled trial (RCT) published in 2020 compared biportal endoscopic lumbar decompression versus microscopic lumbar decompression and demonstrated equivocal postoperative ODI, EQ-5D, and VAS scores at a 12-month follow up [42].
A comparative analysis studied the differences between biportal endoscopy, uniportal endoscopy, and microsurgery for the treatment of lumbar stenosis via bilateral decompression. Microdiscectomy and biportal endoscopy resulted in more significant dural expansion on postoperative MRI compared to uniportal endoscopy. The mean angle of facetectomy was significantly lower in the biportal endoscopy group compared to the other two. Immediate postoperative VAS scores for back pain were significantly lower in both endoscopy groups compared to the microsurgical group. However, at final follow up, there were no significant differences in the VAS scores for back pain or leg pain and no difference in ODI for all three groups [43].
When comparing uniportal and biportal endoscopic surgery, both procedures demonstrated similar efficacy, but the operative time was shorter and central canal decompression was improved in the UBE group [44].
References
- Mayer, M. A History of Endoscopic Lumbar Spine Surgery: What Have We Learnt? BioMed Res. Int. 2019, 2019, 4583943.
- Ahmad, H.; Yoon, J.W. Intra-operative wearable visualization in spine surgery: Past, present, and future. J. Spine Surg. 2022, 8, 132–138.
- Hijikata, S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin. Orthop. Relat. Res. 1989, 238, 9–23.
- Kambin, P. Arthroscopic microdiskectomy. Mt. Sinai J. Med. 1991, 58, 159–164.
- Yeung, A. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS). Surg. Technol. Int. 1999, 8, 267–277.
- Foley, K.; Smith, M.M.; Rampersaud, Y.R. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg. Focus 1999, 7, e5.
- Schubert, M.; Hoogland, T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper. Orthop. Und Traumatol. 2005, 17, 641–661.
- De Antoni, D.J.; Claro, M.L.; Poehling, G.G.; Hughes, S.S. Translaminar lumbar epidural endoscopy: Anatomy, technique, and indications. Arthroscopy 1996, 12, 330–334.
- Ahn, J.-S.; Lee, H.-J.; Choi, D.-J.; Lee, K.-Y.; Hwang, S.-J. Extraforaminal approach of biportal endoscopic spinal surgery: A new endoscopic technique for transforaminal decompression and discectomy. J. Neurosurg. Spine 2018, 28, 492–498.
- Min, W.-K.; Kim, J.-E.; Choi, D.-J.; Park, E.; Heo, J. Clinical and radiological outcomes between biportal endoscopic decompression and microscopic decompression in lumbar spinal stenosis. J. Orthop. Sci. 2020, 25, 371–378.
- Chen, K.-T.; Jabri, H.; Lokanath, Y.; Song, M.-S.; Kim, J.-S. The evolution of interlaminar endoscopic spine surgery. J. Spine Surg. 2020, 6, 502–512.
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Use of newly developed instruments and endoscopes: Full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J. Neurosurg. Spine 2007, 6, 521–530.
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: A prospective, randomized, controlled study. J. Neurosurg. Spine 2009, 10, 476–485.
- Tang, S.; Jin, S.; Liao, X.; Huang, K.; Luo, J.; Zhu, T. Transforaminal Percutaneous Endoscopic Lumbar Decompression by Using Rigid Bendable Burr for Lumbar Lateral Recess Stenosis: Technique and Clinical Outcome. BioMed Res. Int. 2018, 2018, 2601232.
- Zhang, L.-M.; Lv, W.-Y.; Cheng, G.; Wang, D.-Y.; Zhang, J.-N.; Zhang, X.-F. Percutaneous endoscopic decompression for calcified thoracic disc herniation using a novel T rigid bendable burr. Br. J. Neurosurg. 2023, 37, 439–441.
- Lewandrowski, K.-U. Incidence, Management, and Cost of Complications After Transforaminal Endoscopic Decompression Surgery for Lumbar Foraminal and Lateral Recess Stenosis: A Value Proposition for Outpatient Ambulatory Surgery. Int. J. Spine Surg. 2019, 13, 53–67.
- Hasan, S.; Hofstetter, C.P. Endoscopic Spine Surgery Past, Present, and Future. Bull. Hosp. Jt. Dis. 2019, 77, 75–84.
- Gibson, A.; Subramanian, A.; Scott, C. A randomised controlled trial of transforaminal endoscopic discectomy vs microdiscectomy. Eur. Spine J. 2017, 26, 847–856.
- Chen, J.; Jing, X.; Li, C.; Jiang, Y.; Cheng, S.; Ma, J. Percutaneous Endoscopic Lumbar Discectomy for L5S1 Lumbar Disc Herniation Using a Transforaminal Approach Versus an Interlaminar Approach: A Systematic Review and Meta-Analysis. World Neurosurg. 2018, 116, 412–420.
- Lee, C.-H.; Choi, M.; Ryu, D.S.; Choi, I.; Kim, C.H.; Kim, H.S.; Sohn, M.-J. Efficacy and Safety of Full-endoscopic Decompression via Interlaminar Approach for Central or Lateral Recess Spinal Stenosis of the Lumbar Spine: A Meta-analysis. Spine 2018, 43, 1756–1764.
- Ahn, Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev. Med. Devices 2014, 11, 605–616.
- Jasper, G.; Francisco, G.; Telfeian, A. A retrospective evaluation of the clinical success of transforaminal endoscopic discectomy with foraminotomy in geriatric patients. Pain Physician 2013, 16, 225–229.
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. A New Full-Endoscopic Technique for Cervical Posterior Foraminotomy in the Treatment of Lateral Disc Herniations Using 6.9-mm Endoscopes: Prospective 2-Year Results of 87 Patients. Minim. Invasive Neurosurg. 2007, 50, 219–226.
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: A prospective, randomized, controlled study. Spine 2008, 33, 940–948.
- Clark, J.; Abdullah, K.; Steinmetz, M.; Benzel, E.; Mroz, T. Minimally Invasive versus Open Cervical Foraminotomy: A Systematic Review. Glob. Spine J. 2011, 1, 9–14.
- Carr, D.; Abecassis, I.; Hofstetter, C. Full endoscopic unilateral laminotomy for bilateral decompression of the cervical spine: Surgical technique and early experience. J. Spine Surg. 2020, 6, 447–456.
- Kim, J.; Heo, D.H.; Lee, D.C.; Chung, H.T. Biportal endoscopic unilateral laminotomy with bilateral decompression for the treatment of cervical spondylotic myelopathy. Acta Neurochir. 2021, 163, 2537–2543.
- Ahn, Y. Endoscopic spine discectomy: Indications and outcomes. Int. Orthop. 2019, 43, 909–916.
- Ahn, Y.; Keum, H.J.; Shin, S.H. Percutaneous Endoscopic Cervical Discectomy Versus Anterior Cervical Discectomy and Fusion: A Comparative Cohort Study with a Five-Year Follow-Up. J. Clin. Med. 2020, 9, 371.
- Choi, K.Y.; Eun, S.S.; Lee, S.H.; Lee, H.Y. Percutaneous endoscopic thoracic discectomy; transforaminal approach. Minim. Invasive Neurosurg. 2010, 53, 25–28.
- Ruetten, S.; Hahn, P.; Oezdemir, S.; Baraliakos, X.; Merk, H.; Godolias, G.; Komp, M. Full-endoscopic uniportal decompression in disc herniations and stenosis of the thoracic spine using the interlaminar, extraforaminal, or transthoracic retropleural approach. J. Neurosurg. Spine 2018, 29, 157–168.
- Cheng, X.-K.; Chen, B. Percutaneous Endoscopic Thoracic Decompression for Thoracic Spinal Stenosis Under Local Anesthesia. World Neurosurg. 2020, 139, 488–494.
- Kang, M.-S.; Chung, H.-J.; You, K.-H.; Park, H.-J. How i do it: Biportal endoscopic thoracic decompression for ossification of the ligamentum flavum. Acta Neurochir. 2022, 164, 43–47.
- Kim, M.; Kim, H.-S.; Oh, S.W.; Adsul, N.M.; Singh, R.; Kashlan, O.N.; Noh, J.H.; Jang, I.T.; Oh, S.H. Evolution of Spinal Endoscopic Surgery. Neurospine 2019, 16, 6–14.
- Brusko, G.D.; Wang, M.Y. Endoscopic Lumbar Interbody Fusion. Oper. Neurosurg. 2020, 31, 17–24.
- Hussain, I.; Hofstetter, C.; Wang, M. Innovations in Spinal Endoscopy. World Neurosurg. 2022, 160, 138–148.
- Heo, D.H.; Park, C.K. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg. Focus 2019, 46, E18.
- Kang, M.-S.; You, K.-H.; Choi, J.-Y.; Heo, D.-H.; Chung, H.-J.; Park, H.-J. Minimally invasive transforaminal lumbar interbody fusion using the biportal endoscopic techniques versus microscopic tubular technique. Spine J. 2021, 21, 2066–2077.
- Heo, D.H.; Lee, D.C.; Kim, H.S.; Park, C.K.; Chung, H. Clinical Results and Complications of Endoscopic Lumbar Interbody Fusion for Lumbar Degenerative Disease: A Meta-Analysis. World Neurosurg. 2021, 145, 396–404.
- Kim, H.S.; Wu, P.H.; Sairyo, K.; Jang, I.-T. A Narrative Review of Uniportal Endoscopic Lumbar Interbody Fusion: Comparison of Uniportal Facet-Preserving Trans-Kambin Endoscopic Fusion and Uniportal Facet-Sacrificing Posterolateral Transforaminal Lumbar Interbody Fusion. Int. J. Spine Surg. 2021, 15, 72–83.
- Kim, S.-K.; Kang, S.-S.; Hong, Y.-H.; Park, S.-W.; Lee, S.-C. Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: A multicenter, retrospective analysis. J. Orthop. Surg. Res. 2018, 13, 22.
- Park, S.-M.; Park, J.; Jang, H.S.; Heo, Y.W.; Han, H.; Kim, H.-J.; Chang, B.-S.; Lee, C.-K.; Yeom, J. Biportal endoscopic versus microscopic lumbar decompressive laminectomy in patients with spinal stenosis: A randomized controlled trial. Spine J. 2020, 20, 156–165.
- Heo, D.H.; Lee, D.C.; Park, C.K. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: Biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg. Focus 2019, 46, E9.
- Hua, W.; Liao, Z.; Chen, C.; Feng, X.; Ke, W.; Wang, B.; Li, S.; Wang, K.; Zeng, X.; Wu, X.; et al. Clinical Outcomes of Uniportal and Biportal Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression in Patients with Lumbar Spinal Stenosis: A Retrospective Pair-Matched Case-Control Study. World Neurosurg. 2022, 161, e134–e145.
More
