1. Introduction
The oral cavity constitutes a complex biological system, both from a histological point of view and from a functional–biomechanical point of view
[1]. The oral system is an organ able to perform certain functions such as chewing, swallowing, phonation, breathing, facial expressions; these functions are made possible mainly by a pair of joints: the tempo-mandibular joints and naturally by the related muscles
[2]. These anatomical structures can be affected by various kinds of disorders, including genetic, congenital, inflammatory and traumatic events
[3][4][5][3,4,5]. Moreover, the niche of the oral antrum represents a favorable domain for the invasion of external agents from the external environment
[6]. The coexistence between external microbial agents and the host is guaranteed by a constant balance of the oral habitat, nowadays also known as oral microbiome
[7]. An alteration of the microbial flora, due to various intrinsic and extrinsic factors, may determine the phenomenon of dysbiosis
[8][9][10][8,9,10]. The mechanisms involved in oral dysbiosis have shown to lead to most of the dental and periodontal tissues of the oral cavity, which recognize microbiological agents—viral, bacterial and fungal—as the main nosological factors
[11][12][13][11,12,13]. Oral mucosal soft tissues, instead, are mainly affected by mycotic superinfections, with a greater prevalence for frail patients, immunosuppressed subjects and prosthesis wearers
[14][15][16][14,15,16]. Furthermore, a large group of viral agents is involved in the etiological mechanism of a wide spectrum of oral mucosa diseases, ranging from acute to chronic disorders
[17][18][19][20][21][17,18,19,20,21].
Pathological cytoarchitectural changes in the tissue layers of the oral mucosa are seen in a wide range of disorders, ranging from benign
[22] to potentially malignant and properly malignant conditions
[23][24][25][26][23,24,25,26], up to the involvement of rare syndromic manifestations involving multiple areas of the body
[27][28][27,28]. Benign disorders affecting the oral mucosa represent a large group of pathological manifestations, especially autoimmune, viral and neuropsychiatric diseases
[29][30][31][32][33][34][29,30,31,32,33,34]. However, the oral cavity is linked to the possible occurrence of malignant lesions, and 90% of them are represented by Oral Squamous Cell Carcinoma (OSCC), the 16th most common worldwide cancer
[35].
Furthermore, there are several pathological entities involving oral mucosa that may show an increased risk of malignant transformation, which are also known as Oral Potentially Malignant Disorders (OPMD), and they are represented by manifestations such as Oral Leukoplakia, Oral Eritroplakia and Proliferative Verrucous Leukoplakia
[36][37][36,37].
2. Oral Potentially Malignant Disorders
Oral Potentially Malignant Disorders (OPDMs) represent a wide scenario of pathological manifestations, which may not include the onset of oral cavity malignant neoplastic lesions; this nomenclature has been asserted because not all disorders described under this term may transform into cancer
[38].
2.1. Oral Leukoplakia, Proliferative Verrucous Leukoplakia and Erythroplakia
One of the most frequently encountered lesions classified as an OPMD in the oral cavity is Oral Leukoplakia (OL)
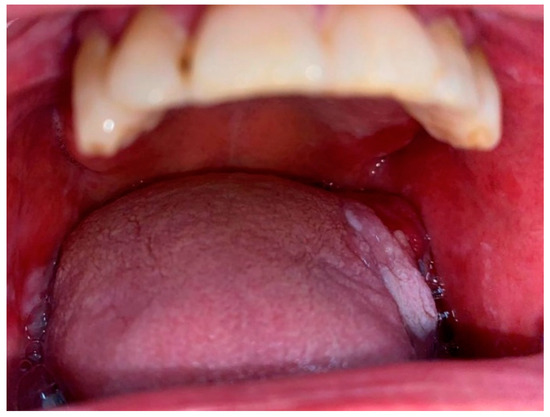
[39][44] (
Figure 1). A smoking habit has shown to be recurrently associated with leukoplakia in more than 80% of cases; OL represents a non-scraping white lesion and it is defined by the World Health Organization (WHO) as a “white plaque of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer”
[40][45]. From a clinical point of view, there are different varieties for this entity: homogeneous leukoplakia presents as a flat and uniform white plaque with well-defined margins (at least one). Non-homogeneous leukoplakia involves spots of erythema surrounded by areas of nodularity and verrucousity
[41][46]. Oral Proliferative Verrucous Leukoplakia (PVL) is a distinguishing subset of non-homogenous leukoplakia more common in females and less associated with a smoking habit. PVLs may involve a single extensive area but are often multifocal and frequently occur on the gingiva, buccal mucosa, and tongue in both bordering and non-contiguous sites of the oral cavity
[42][43][47,48]. The mechanisms underlying the transformation from hyperkeratosis or hyperplasia to various degrees of dysplasia and eventually carcinoma in situ and/or OSCC are still subject to ongoing debate. As a result, PVLs and leukoplakias necessitate multiple recurring biopsies at different sites. This ongoing need for biopsies is essential to continuously investigate the histotype and detect different grades of dysplasia or malignant transformation to OSCC
[44][45][46][49,50,51].
Figure 1. Oral Leukoplakia involving the tongue.
Furthermore, the lesion called “Oral erythroplakia” (OE) has been defined by the WHO as “a fiery red patch that cannot be characterized clinically or pathologically as any other definable disease” and it has long been deemed as the oral mucosal lesion with the greatest potential for malignant transformation in the oral cavity
[47][52]. OE does not occur on any traumatic, vascular, or inflammatory basis, but appears with comparable frequency in both sexes in middle-aged and elderly patients. A diagnostic biopsy is required to detect this potentially malignant lesion, more accurately analyze this histological subset and even prevent the risk of transformation
[48][53].
2.2. Oral Lichen Planus
To date, experts adhere to the distinction between precancerous lesions and precancerous conditions for the main reason that the onset of a malignancy in the mouth of a patient known to have a precancerous lesion would correspond with the site of precancer, while in precancerous conditions, malignancy may originate in any anatomical site of the oral cavity
[40][45].
One of the most recognized oral potentially malignant conditions is represented by Oral Lichen Planus (OLP), a chronic immunological inflammatory disease that usually affects middle-aged patients, particularly women
[49][54]. This disorder may involve the skin and mucosal membranes; moreover, OLP is usually linked to various patterns and the subtypes can be categorized as follows: reticular form, which is the most common subtype, distinguished by Wickham striae and hyperkeratotic plaques or papules; atrophic–erosive form, with areas of ulceration usually associated with keratotic white striae, and also ulcerations
[50][55]. The plaque form of Oral Lichen Planus can mimic Oral Leukoplakias, which highlights the importance of biopsy
[51][56]. OLP generally involves the buccal mucosa, followed by the gingiva and tongue, usually with multiple, bilateral lesions. Erosive and atrophic OLP can provoke intense discomfort and inhibit speech and swallowing
[50][55]. It is still debated whether Oral Lichen Planus can progress into Oral Squamous Cell Carcinoma: data concerning the transformation rates range between 0% and 12.5%, and no clinical or histopathological suggestion can support the prognosis of potential malignant transformation
[52][53][57,58]. The erosive form bears the highest risk rate of malignant transformation, followed by atrophic OLP, while the reticular white type has the lowest risk rate
[54][55][59,60].
2.3. Submucosal Fibrosis
Another characteristic oral potentially malignant condition is represented by Submucosal Fibrosis
[56][61]. This condition presents as a chronic fibrotic lesion of the oral mucosa, possibly as the expression of a large wound overhealing, based on a chronic mechanical or chemical insult
[57][62]. With a predominance in males, the most commonly affected sites are the buccal mucosa, the lingual margins, the lip, the palate, and the gums
[58][63]. Clinically, Submucosal Fibrosis is characterized by a loss of elasticity in the affected tissues, with palpable fibrous bands that involve the mobility of the tongue and restrict mouth opening
[59][64].
To date, Submucosal Fibrosis has been widely recognized to carry a malignant potential; an estimated transformation rate of 8% has been reported
[60][65].
2.4. Actinic Keratosis
Actinic Keratosis (AK) is a common precancerous skin lesion that may also affect oral and peri-oral tissues, caused by long-term sun exposure. It appears as a rough, scaly patch on sun-exposed areas of the skin, such as the face, neck, arms, and hands. If left untreated, AK can develop into squamous cell cancer. Early detection and treatment, such as cryotherapy or topical medications, can prevent the progression of AK to malignant transformation. Regular use of sun protection, such as sunscreen and protective clothing, can also reduce the risk of developing AK. It is important to seek the advice of a healthcare professional for proper diagnosis and management of actinic keratosis
[61][66].
2.5. Graft versus Host Disease
According to the WHO Classification of Tumours, 4th Edition (2017)
[62][67], Oral Graft versus Host Disease (GVHD) is considered as a potentially malignant disorder, and it describes a condition that can occur after a bone marrow or stem cell transplant, when the transplanted cells attack the recipient’s body. In Oral GVHD, the mouth, including the lips, gums, tongue, and inside of the cheeks, is affected
[63][68]. Symptoms may include redness, swelling, sores, and painful or difficulty in swallowing. Oral GVHD can be a severe and life-threatening condition, and early detection and prompt treatment are important for the best outcome. Treatment may include topical or systemic medications, and in severe cases, additional interventions such as surgery may be necessary. Regular monitoring by a healthcare professional is important for the management of Oral GVHD. Nevertheless, no Oral Potentially Malignant Disorder is considered as a compulsory forerunner to cancer; likewise, most Oral Potentially Malignant Disorders do not lead to cancer
[64][69]. Hence, the most challenging struggle involves determining lesions that display a higher risk of transformation from those carrying a lower risk. Dysplastic features are supposed to be the most valuable indicator of potential malignant progression
[65][66][70,71].
Nonetheless, a lesion with no sign of dysplasia carries the potential to transform into cancer, and there are no specific clinical signs directly associated with dysplastic features; therefore, a biopsy is invariably mandatory to assess whether dysplasia is present
[67][72].
3. Oral Malignancies
Oral malignant neoplasms belong to the variety of head and neck cancers (H&N cancers), which represent a wide group of epithelial malignant tumors involving the lining mucosa of the nasal cavity and paranasal sinuses, nasopharynx, hypopharynx, larynx and trachea, oropharynx, oral cavity and salivary glands
[68][73]. Although there is a large group of mostly rare malignant neoplasms affecting the oromaxilofacial area
[69][70][71][74,75,76], Oral Squamous Cell Carcinoma (OSCC) represents a malignant neoplasm involving the oral cavity, leading to more than 90% of malignant tumors of the head and neck area, ranking as the 16th most common worldwide cancer
[72][77], and it stands as the most common malignancy in South-East Asia (India, Sri Lanka, Pakistan, Bangladesh, and Taiwan) and the Pacific regions (Papua New Guinea and Melanesia) due to the betel chewing habit
[73][78] (
Figure 2). Tobacco and alcohol consumption represent two of the major risk factors for the development of oral cancer
[74][79]; nevertheless, many other elements have been reported to increase the risk of OSCC, such as micronutrient depletion, hormonal, protein and enzyme imbalances
[75][76][77][78][79][80,81,82,83,84], poor oral hygiene, chronic traumatism, and viruses
[80][81][85,86]. Poor oral hygiene has been always associated with the risk of the development of periodontal disease, so current investigations are focusing on the possible association between the periodontal status of health and oral cancer risk
[82][87]. The potential role of human papillomavirus (HPV) infection and its relationship with cancerogenesis are the most explored but still debated topics among all human viruses. Human papillomavirus infection has a potential role in carcinogenesis. To date, more than 100 genotypes of HPV are known, divided into low risk and high risk. The viral proteins E6 and E7 play a key role in pathogenesis, particularly by inhibiting the oncosuppressors p53 and Rb, with overexpression of the p16 protein. Data in the literature show that HPV16 represents about 86% of HPV+ oropharyngeal squamous cell carcinomas (OPSCC) cases, while the association between OSCC and human papillomavirus infection is still debated
[83][84][85][86][88,89,90,91]. From a purely clinical point of view, various forms have been reported, including the endophytic form, infiltrative exophytic form, vegetative or papillary, ulcerative form and mixed form
[87][92]. The recurrence and prognosis of OSCC have been deeply investigated in different studies and a close relationship with histological malignancy grading and different clinical parameters has been found
[35][88][89][35,93,94]. Besides the recurrence of OSCC, survival and mortality rely on multiple and additional biological, histological, macroscopic, and microscopic aspects that have been analyzed in order to determine the causalities, support early diagnosis and develop suitable remedies for the different characteristics and grades of Oral Squamous Cell Carcinomas
[90][91][95,96]. Site, size and thickness—or the depth of invasion—of the cancer have been the most examined prognostic factors for achieving the current survival rates. The closer the tumor origin is to the inner sites of the mouth, the lower the survival rates
[92][97]; furthermore, the survival rate decreases in relation to the advanced involvement of regional lymph nodes
[93][98]. To date, approximately 60% of OSCC lesions are detected in locally advanced stages, when the 5-year survival rate is <50–60%
[94][99]. In addition, conventional histopathological data seem to be unsatisfactory in accurately foretelling the clinical evolution of OSCC
[95][100]; consequently, the need for a label of molecular markers that can predictively demarcate which cancer will display an aggressive behavior and poorer prognosis should be highlighted
[96][97][98][101,102,103]. Treatment options include surgery, radiation therapy, chemotherapy, and targeted therapy
[88][93]. The type and extent of treatment will depend on the size and location of the tumor and the overall health of the patient. It is important to work with a healthcare team to develop an individualized treatment plan. Regular dental check-ups and oral cavity screenings can help detect OSCC in its early stages and increase the chances of successful treatment
[62][67].
Figure 2. Oral Squamous Cell Carcinoma involving the tongue.
The early diagnosis of the asymptomatic first stages of oral cancer is still the pivotal and most demanding step to achieving an adequate clinical outcome in most patients.