You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 1 by Hussain Al akam and Version 2 by Sirius Huang.
Since the introduction of calcium silicate-based materials in dentistry, calcium silicate-based root canal sealers have become popular among dentists because of their biocompatibility, bioactivity, and sealing ability. Therefore, effective retreatment strategies are indispensable.
- calcium silicate-based root canal sealer
- retreatment
- solvent
1. Introduction
1.1. Calcium Silicate-Based Sealer (CSS)
A surge in the popularity of calcium silicate-based sealers (CSSs) has been noticed recently in the field of endodontics. Since iRoot SP™ (Innovative Bioceramics, Vancouver, Canada) was first introduced in 2007, many new brands of CSSs have been marketed, and more dentists are interested in using CSSs. The properties of CSSs are unique because of the setting process and their byproducts, which contribute to their popularity.
1.2. Properties of CSSs
The unique properties of CSSs include their setting process and their byproducts. CCSs are hydraulic sealers that require the presence of water for their setting. The setting process includes the reaction of the CSS with water. This reaction results in the formation of calcium hydroxide as a byproduct [1].
2(3CaO·SiO
2
) + 6H
2
O = 3CaO·2SiO
2
·3H
2
O + 3Ca(OH)
2
2(2CaO·SiO
2
) + 4H
2
O = 3CaO·2SiO
2
·3H
2
O+Ca(OH)
2
The set sealer produced has been found to be biocompatible and bioactive [2][3][2,3]. Hydroxyapatite, as a secondary byproduct, is deposited on the surface of the set sealer, contributing to the bioactivity of the set CSS [3]. The emanation of calcium hydroxide ions from CSSs elevates the pH, which contributes to the sealers’ antimicrobial efficacy [2][4][2,4].
1.3. Outcome of Root Canal Treatment Using CSSs
The outcomes of non-surgical initial root canal treatments and retreatments using CSSs encourages more clinicians to use CSSs for obturation. In a non-randomized clinical trial, a calcium silicate-based sealer in combination with the single-cone technique demonstrated success rates, ranging from 84% to 90%, while the epoxy resin-based sealer with a continuous wave condensation technique showed success rates from 80% to 89% [5]. In addition, a randomized clinical trial compared the success rate of a CSS with the single-cone technique and an epoxy resin-based sealer with the continuous wave condensation technique. The results showed an average success rate of 94.3% for the CSS with the single-cone technique in comparison to 92.3% for the teeth obturated with the epoxy resin-based sealer using the continuous wave condensation technique [6]. These promising results and favorable outcomes encourage and motivate clinicians to use CSSs more extensively in the practice of endodontics. The increased use of CSSs among endodontists and general practitioners has prompted the need to implement new strategies of retreatment for cases obturated with CSSs. For instance, regaining patency is a potential challenge that can occur during the removal of CSSs [7].
2. Retreatment
2.1. Reason for Retreatment
In general, the success of endodontic treatment can be evaluated by the absence of signs and symptoms of infection or inflammation, including pain, tenderness to palpation and percussion, and the absence of any soft tissue signs of infection, such as swelling, in combination with radiographic evidence of periapical lesion healing and bone formation and regaining the mastication force and normal function of the treated teeth [8][9][8,9]. The presence of signs and/or symptoms is the main reason for retreatment. The purpose of retreatment is to eliminate the presence of persistent infection in the root canal system. Radiographic presence of periapical pathology is an important diagnostic method that has been used to evaluate healing after root canal treatments [10][11][12][10,11,12]. Reinfection can occur because of various factors, such as poor coronal restoration or the presence of missed root canals [13][14][15][13,14,15]. The presence of radiographic radiolucency before the initial endodontic treatment has been found to increase the possibility of failure and the need for retreatment as a result [16]. In addition, retreatment using modern technology has been found to be beneficial to patients’ quality of life [9].
2.2. Factors Affecting the Outcome of Retreatment
Numerous studies have discussed the outcome of endodontic retreatment. Endodontic retreatment showed high success rates in most of these studies. Ng et al. [17], in their prospective study, which included annual clinical and radiographic evaluation of teeth which had been initially treated and retreated, found that the success rate of retreatment was comparable to that of the initial treatment. The success of retreatment is influenced by many factors. These factors include the presence of periapical radiolucency and its size [17], case selection [18][19][18,19], accessibility to the obturation material throughout coronal restoration [20], and retrievability of the different obturation materials [21]. The last factor is critical for clinicians to expect a favorable prognosis before executing the retreatments of teeth obturated with CSSs due to the absence of solvents. Friedman et al. [21] divided the obturation materials based on their setting process into soft-setting pastes, which are easy to remove and clean, and hard-setting cements, which might require the usage of solvents in combination with mechanical debridement to remove [21]. In addition to the obturation material, the obturation technique is another critical factor in determining the complicity of retreatment (Figure 1). DeLong et al. [22] compared the push-out bond strength of two CSSs (MTA Plus Sealer™ (Avalon Biomed Inc, Bradenton, FL, USA) and EndoSequence BC Sealer™ (Brasseler USA, Savannah, GA, USA)) and an epoxy resin-based sealer, AH Plus™ (Dentsply De Trey Gmbh, Konstanz, Germany), using both the single-cone obturation technique and the continuous wave obturation technique. They found that the continuous wave technique decreased the bond strength of the MTA Plus Sealer™ and that the CSS with a single cone demonstrated the highest push-out resistance [22]. This study showed that the obturation technique might influence the setting properties of the sealers. Athkuri et al. [23] assessed the retrievability of root canal filling material obturated with cold lateral condensation, warm vertical condensation, and thermoplasticized injectable techniques along with the AH Plus™ sealer and BioRoot RCS™ (Septodont, Saint-Maur-des-Fossés, France). The samples that were obturated with the thermoplasticized technique demonstrated a higher percentage of root filling residuals after the removal of root fillings than the lateral condensation or warm vertical compaction techniques. However, there were no significant relationships between the type of sealer used and the amount of residual filling [23]. This indicates that the obturation technique used during the initial endodontic treatment affects the retrievability of the root filling material during retreatment. Therefore, clinically, the outcome of retreatment is affected by multiple factors, and its outcome varies depending on the various scenarios.
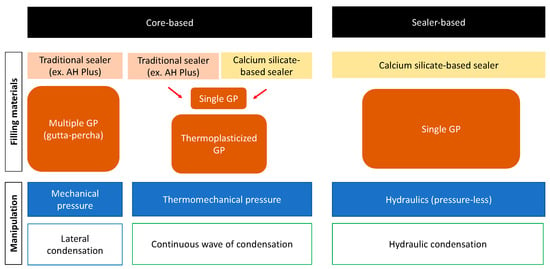
Figure 1.
Schematic concepts of obturation methods.
2.3. Challenges and Risks Specific to CSSs
No solvents have decisively proven to be effective in dissolving CSSs. For this reason, the challenges associated with the retrievability of CSSs might depend on the final setting of the sealers. Soft-setting CSSs are easier to remove from the root canal system, whereas hard-setting CSSs might necessitate the use of solvents in combination with mechanical debridement [21][22][21,22].
3. Current Retreatment Techniques
Current CSSs retrieval techniques can be divided into chemical and mechanical techniques.3.1. Solvents for Gutta-Percha
The gutta-percha cone is a semisolid obturation material. It is considered the material of choice in modern endodontics. Excessive mechanical removal of the gutta-percha can lead to alterations in the anatomy of the root canals. Solvents are commonly recommended to avoid any alteration in the anatomy and facilitate the removal of the gutta-percha. Chloroform is the most effective solvent used for the removal of gutta-percha. Its properties of fast action, strength, and fast evaporation make it a respectable choice as a solvent. However, chloroform has since been found to be cytotoxic and carcinogenic; therefore, extrusion beyond the apex should be avoided. The use of xylene and eucalyptol as alternatives to chloroform has been suggested, but they have also been found to be less effective and impractical to use clinically. Wennberg and Ørstavik suggested the use of methyl chloroform as an effective, less toxic alternative to chloroform. It has been found to be less effective than chloroform but more effective than xylene and eucalyptol [24][25][36,37].3.2. Chemical Dissolution of CSSs
The possible chemicals that can be employed in the retrieval of CSSs have been evaluated in many studies. Numerous studies have examined the difference in solubility between CSSs and epoxy resin-based sealers and the effect of different solvents on CSSs. Borges et al. [26][38] subjected AH Plus™, iRoot SP™, MTA Fillapex™, Sealapex™ (Sybron Endo/Kerr Co, Orange, CA, USA), and MTA-Angelus™ (Angelus, Londrina, PR, Brazil) to solubility tests to compare their surface structure changes and ion release (Table 1). The samples of the sealers were assessed using scanning electron microscopy and energy-dispersive spectroscopy. The study found that iRoot™, MTA Fillapex™, and Sealapex™ have a higher solubility than AH Plus™ and MTA-A™. The study also revealed that CSSs exhibit a high release of calcium ions [26][38]. The pH of the surrounding environment was shown to be a critical factor in the solubility of CSSs (Table 1). Endo Sequence BC Sealer™ was found to be significantly more soluble than AH Plus™ in a low pH [27][39]. This implies that acids might have the potential to serve as solvents for CSSs. Thermal treatment as a physical means was found to be effective in altering the structure of CSSs and impacting their solubility [28][40]. Ideal solvents are intended to only affect sealers without affecting the integrity of dentine. Garrib et al. [29][41] studied the effect of irrigating with 17% EDTA along with either 10% or 20% formic acid on the integrity of TotalFill BC sealer™ and the integrity of dentine (Table 2). The study found that irrigating with 17% EDTA and 10% formic acid did not affect the integrity of the dentine. However, irrigation affected the integrity of the CSS used in the study and aided its mechanical removal. The use of 20% formic acid was found to corrode the integrity of dentine [29][41]. The efficacy of 20% hydrochloric acid and chloroform in comparison with 10% formic acid in regaining apical potency has been investigated. There is no significant difference among them in terms of regaining patency [30][31]. Therefore, 10% formic acid is deemed to be a promising solvent when used to penetrate CSSs and regain patency.3.3. Mechanical Removal of CSSs
The use of conventional hand files and modern rotary and NiTi files in the removal of CSSs has been assessed in multiple studies. Donnermeyer et al. [31][35] compared the efficacy and retreatment time of Hedström files, Reciproc R40, Mtwo retreatment file R 25/0.06, Mtwo 40.06, and F6 SkyTaper size 040 in the removal of CSSs and epoxy resin-based sealers (Table 2). Regarding the amount of sealer remnants, all NiTi rotary files performed much better than the Hedström hand files, regardless of the sealer type. The F6 SkyTaper instruments were found to be the fastest when compared with all the files that were being assessed [31][35]. Furthermore, the use of reciprocating files occupied a portion of the interest in the mechanical techniques for removing CSSs. Kırıcı et al. [32][42] compared two reciprocal systems, M-Wire Reciproc and Reciproc Blue, and evaluated their efficacy in the removal of CSSs and their competence in preserving the root canal’s anatomy in curved canals using micro-CT. No significant difference in the amount of residual was found between the two systems. However, apical canal transportation was found to be significantly higher in the M-Wire Reciproc group, but the formation of incomplete and complete cracks was witnessed with both systems [32][42]. Despite the positive results that were reached in these past studies with different mechanical means for the removal of CSSs, no mechanical technique was found to completely remove CSSs from the root canal system.3.4. Integrating Technology into Retreatment of CSSs
The use of modern mechanical techniques has been discussed in various studies. Fruchi et al. [33][43] conducted a micro-CT evaluation to measure the efficacy of sealer removal using the Reciproc R25 instrument or WaveOne Primary files along with xylene and passive ultrasonic irrigation in curved canals (Table 2). The Reciproc instrument and the WaveOne Primary files showed a removal efficacy of 93% and 92%, respectively. The use of xylene and PUI helped in the removal of the root canal filling material but did not increase the percentage of the removed filling material significantly [33][43]. Wright et al. compared the usage of two modern irrigation protocols, EndoVac and GentleWave, to the efficacy of the usage of a side-vented needle in the removal of root canal filling materials. Micro-CT imaging was used to evaluate the percentage of the removal of the root canal filling material for all three irrigation techniques. GentleWave removed the highest ratio of the residuals of the root canal filling material, followed by the side-vented needle. EndoVac was found to remove the least amount of residuals of the root canal filling material [34][44]. Wright and Fruchi [33][34][43,44] found that AH Plus was more difficult to remove than CSSs (Table 2). The efficacy of shock wave-enhanced emission photoacoustic streaming (SWEEPS) in CSS removal has also been evaluated. Angerame et al. [35][45] compared the efficacy of SWEEPS with the efficacy of passive ultrasonic irrigation (PUI) in the removal of CSSs ex vivo (Table 2). The combination of reciprocating instrumentation with SWEEPS provided more satisfying results than the usage of reciprocating instrumentation combined with PUI [35][45]. The XP-endo Finisher R system removed more CSSs compared to the ultrasonic-assisted irrigation or EndoActivator [36][46]. Despite continuous effort to assess the efficacy of mechanical techniques and modern irrigation technology in the removal of CSSs, no technique has been proved to completely remove CSSs from the root canal system in the literature (Table 2).Table 1.
Sealers used in the solubility studies mentioned herein.
| Sealers | Manufacturers | Composition | Solubility (%) | Reference |
|---|
Materials and instruments used in the treatment studies.
| Name | Company | Type | Reference | |||||
|---|---|---|---|---|---|---|---|---|
| iRoot SP | Innovative BioCeramix Inc., Vancouver, Canada | Zirconium oxide, calcium silicates, calcium phosphate, calcium hydroxide filler, and thickening agents | 20.64 ± 1.42 | [26][38] | ||||
| XP-endo Finisher R instrument | FKG Dentaire, La Chaux-de-Fonds, Switzerland | Mechanical | [37][33] | |||||
| MTA Fillapex | Angelus, Londrina, PR, Brazil | Components after mixture: resins (salicylate, diluting, natural), radiopaque bismuth, nanoparticulated silica, mineral trioxide aggregate, and pigments |
14.89 ± 0.73 | [37][26 | ||||
| Eucalyptol | [ | 33 | ] | [ | Biodinamica, Ibiporã, PR, Brazil]38] | |||
| Chemical | Sealapex | Sybron Endo/Kerr Co, Orange, CA, USA |
Calcium oxide, bismuth trioxide, zinc oxide, submicron silica, titanium dioxide, zinc stearate, tricalcium phosphate, ethyl toluene sulphonamide, poly(methylene methyl salicylate) resin, isobutyl salicylate, and pigments |
5.65 ± 0.80 | ||||
| Reciproc R40 NiTi files | [ | 26 | ] | [38 | VDW, Munich, Germany] | |||
| Mechanical | [ | 31 | ][35] | MTA-A | Angelus, Londrina, PR, Brazil | Tricalcium silicate, dicalcium silicate, tricalcium aluminate, tetracalcium aluminoferrite, bismuth oxide, iron oxide, calcium carbonate, magnesium oxide, crystalline silica, and residues (calcium oxide, free magnesium oxide, potassium, and sodium sulphate compounds) |
−1.24 ± 0.19 | [26 |
| Mtwo retreatment file R 25/0.06 | VDW GmbH, Munich, Germany | Mechanical | [31][35] | ][38] | ||||
| AH Plus | Dentsply De Trey Gmbh, Konstanz, Germany |
Component A: epoxy resin, calcium tungstate, zirconium oxide, aerosil, and iron oxide. Component B: adamantane amine, | ||||||
| F6 SkyTaper size 040 | N,N-Dibenzyl-5-oxanonane, TCD-Diamine, calcium tungstate, |
KOMET, Lemgo, Germanyzirconium oxide, and aerosi | 0.28 ± 0.08 | Mechanical | [31][35][26][38] | |||
| AH Plus Jet | Dentsply DeTrey Gmbh, Konstanz, Germany |
Bisphenol A/F epoxy resin, calcium tungstate, zirconium oxide, silica, iron oxide pigments dibenzyldiamine, aminoadamantane, and silicone oil |
0.04 ± 0.11 to 0.26 ± 0.15 2 |
[27][39] | ||||
| EndoSequence BC Sealer | Brasseler USA, Savannah, GA, USA | Zirconium oxide, calcium silicates, calcium phosphate monobasic, calcium hydroxide filler, and thickening agents | 4.96 ± 0.94 to 12.88 ± 0.94 2 |
[27][39] |
2 The study demonstrated a difference in the solubility related to the time and the pH. The difference in solubility was demonstrated with a range of values.
Table 2.
| 10% formic acid | |||
| Sigma Aldrich, Gillingham, UK | |||
| Chemical | [ | 29 | ][41] |
| 20% formic acid | Sigma Aldrich, Gillingham, UK | Chemical | [29][41] |
| ProTaper Gold finisher file | Dentsply, Charlotte, USA | Mechanical | [29][41] |
| M-Wire Reciproc | VDW GmbH, Munich, Germany | Mechanical | [32][42] |
| Reciproc Blue | VDW GmbH, Munich, Germany | Mechanical | [32][42] |
| xylene | Not mentioned | Chemical | [33][43] |
| Reciproc R25 instrument | VDW, Munich, Germany | Mechanical | [33][43] |
| WaveOne Primary instrument | Dentsply Maillefer, Tulsa, USA | Mechanical | [33][43] |
| Reciproc Blue files | VDW GmbH, Munich, Germany | Mechanical | [35][45] |
| XP-endo Finisher R system | XPR; FKG Dentaire, La Chaux-de-Fonds, Switzerland | Mechanical | [36][46] |
