Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Brandon Lucke-Wold and Version 2 by Peter Tang.
Aneurysmal subarachnoid hemorrhage (SAH) can lead to devastating outcomes including vasospasm, cognitive decline, and even death. Treatment options are limited for this potentially life threatening injury. Evidence suggests that neuroinflammation plays a critical role in injury expansion and brain damage. Red blood cell breakdown products can lead to the release of inflammatory cytokines that trigger vasospasm and tissue injury. Preclinical models have been used successfully to improve understanding about neuroinflammation following aneurysmal rupture.
- aneurysmal subarachnoid hemorrhage
- cerebral vasospasm
- neuroinflammation
- novel treatments
1. Introduction
Aneurysmal subarachnoid hemorrhage (SAH) can lead to devastating outcomes for patients, including cognitive decline, cerebral vasospasm (CV), and delayed cerebral ischemia [1][2][1,2]. The underlying mechanisms contributing to injury expansion following aneurysmal SAH are poorly understood, therefore limiting the number of effective pharmaceutical treatment options. Recent evidence implicates neuroinflammation as a key mediator of injury expansion and behavioral deficits [3][4][3,4]. Peripheral immune cells are both recruited and activated in damaged tissue [5]. These cells can enter the brain parenchyma and release inflammatory cytokines [6]. Additionally, intrinsic toll-like receptors are upregulated after infarction leading to widespread neuroinflammation [7]. Furthermore, neuroinflammation has been linked to adverse secondary outcomes that occur after SAH. Vessels undergoing CV have increased leukocyte adhesion capacity contributing to delayed neurologic deterioration [8][9][8,9].
2. Neuroinflammation
2.1. The Role of Inflammation
Emerging evidence points to inflammation playing a major role in acute and chronic phases of neural injury associated with aneurysmal SAH [10][11][10,11]. In the following sections, thwe researchers reeview and explore some of the pathophysiology associated with aneursymal SAH, particularly in relation to the neuroinflammatory response. The researchers cWe conclude the section by highlighting new avenues and suggest further studies to address lingering questions within the field of aneurysmal SAH.2.2. SAH Pathophysiology: Acute Events
The initial aneurysmal rupture deposits blood within the subarachnoid space. Red blood cell breakdown and degradation over time leads to the deposition of hemoglobin. Methemoglobin, heme, and hemin resulting from red blood cell breakdown can lead to activation of TLR4, which signals inflammatory cascades that damage neurons and white matter [12][13][12,13]. Hemin has been linked with the release of redox-active iron, altering the balance of oxidants and anti-oxidants. The redox-active iron depletes anti-oxidant stores such as nicotinamide adenine dinucleotide phosphate (NADPH) and glutathione while producing superoxide and hydroxyl radicals as well as lipid peroxidation [14][15][14,15]. As blood leaves the confines of the vasculature following aneurysmal rupture, immunomodulatory cells within the CNS, such as microglia, are activated. These cells trigger the upregulation of numerous cell adhesion molecules within endothelial cells, which subsequently allows a multitude of inflammatory cells to bind and enter the subarachnoid space [16][17][16,17]. Once in the subarachnoid space, these inflammatory cells, macrophages and neutrophils, phagocytize the extravasated, degrading red blood cells [12]. This process occurs in an effort to clear free hemoglobin, and promote neurostability and recovery. Hemoglobin clearance is facilitated by the binding of hemoglobin to haptoglobin for rapid engulfment by immune cells [13].2.3. SAH Pathophysiology: Subacute-Chronic Events
As described above, pre-clinical data suggest that aneurysmal SAH is associated with the attraction and subsequent deposition of neutrophils and macrophages in response to free hemoglobin and hemin. A key area requiring further investigation is how these neutrophils and macrophages are recruited and whether they pass through an intact or disrupted blood brain barrier. While these peripheral immune cells are essential for clearing hemoglobin, the cells can become trapped in the subarachnoid space due to alterations in cerebral spinal fluid (CSF) flow and the restoration of the endothelial tight junction barrier. Once trapped within the subarachnoid space, the macrophages and neutrophils undergo degranulation, which releases a multitude of inflammatory factors. A few of these include endothelins and oxidative radicals. These factors can cause inflammation-induced vasoconstriction, arterial narrowing, meningitis, and cerebritis [18]. Importantly, the inflammatory response is generalized, causing the release of inflammatory cytokines, endothelial adhesion molecules, and activated complement throughout the brain [19][20][19,20].2.4. Inflammatory Mediators in SAH: A Focus on Cytokines and Cell Lines
Inflammation following aneursymal SAH has been investigated in order to characterize the timing, magnitude, and site of cytokine release [21][22][21,22]. For example, IL-1β, IL-6, and TNFα are released into both the serum and cerebrospinal fluid following SAH [23][24][23,24]. Similarly, these same cytokines have been shown in animal models of SAH to be increased in the cerebral arterial wall [25]. While the role that these cytokines play in SAH warrants further investigation, prevailing clinical signs such as neutrophilia, pyrexia, and general cerebral edema are likely associated with the cytokine storm [26]. The current lack of clarity with regards to the beneficial or detrimental role inflammation plays following aneurysmal SAH is perhaps best exemplified by the mixed results of preclinical and clinical studies. Some clinical studies have found that modulating inflammation following SAH is beneficial while other studies have shown no beneficial effect at all [27]. It is likely that activation of inflammation at different time points post rupture is associated with different protective or detrimental responses depending on the surrounding milieu and type of cells recruited to the site. What is apparent is the prominent role inflammation plays in causing cerebral vasospasm (CV). Injection of pro-inflammatory materials/compounds intracisternally induces CV, even in the absence of blood breakdown products [1]. Clinically, the inflammatory response appears in close temporal relationship with the spasm and in direct proportion to the magnitude of the inflammatory response [28]. These findings have been supported by evidence suggesting that accumulation of inflammatory cells closely parallels neuronal cell death. Cell death near the vasculature has been substantially reduced by depletion of inflammatory cells in preclinical studies [29]. A substantial knowledge gap persists in understanding the adaptive immune response in SAH. Emerging evidence from preclinical studies has implicated B and T lymphocyte infiltration into the vessel wall of aneurysms, which may potentially promote aneurysmal rupture and SAH [30][31][30,31]. Preliminary data from clinical studies indicate a diffuse presence of not only innate immune cells but also adaptive immune cell populations in the CSF and serum following SAH [5]. While it is difficult to draw conclusions based upon this preliminary study, it is promising in that a new therapeutic target and avenue may be available in the future [32][33][32,33]. CSF biomarkers may be used to guide physicians on the appropriate selection of pharmaceutical agents.2.5. Inflammatory Mediators in SAH: A Focus on Proteases
Additional inflammation-specific SAH studies have focused on matrix metalloproteinases (MMPs), a family of proteases consisting of multiple subtypes. The most widely investigated of these being MMP-9 [34][35][34,35]. MMP-9 has been shown to be responsible for the degradation of tight junction proteins, which are critical in the maintenance of blood-brain barrier (BBB) integrity. Notably, clinical studies of SAH have reported an elevation of MMP-9 in brain tissue, serum, and cerebrospinal fluid [36][37][36,37]. Consistent with cytokine studies, MMP-9 is elevated not only in serum and CSF but also in the vessel wall [25]. These studies document a potential novel approach for treatment of SAH. By targeting MMP-9 in the vessel wall, it could be possible to restore BBB integrity or prevent BBB disruption from occurring in the first place. Preventing basement membrane degradation could facilitate enhanced reconstitution of tight junction protein binding.2.6. SAH-Associated Inflammation: An Inflow or an Outflow Problem?
CSF flow disruption is associated with inflammation following SAH [38]. This is consistent with clinical symptoms where obstructive hydrocephalus is commonly reported due to the presumed breakdown of blood products in the subarachnoid space and subsequent obstruction of CSF drainage pathways. The etiology of this condition is actually poorly understood and may in fact be due to obstruction of the glymphatic system described by Nedergaard and colleagues [39]. The system is critical for CSF circulation and consists of multiple channels around the vasculature. While the glymphatic system remains under investigation in several neurological injury models such as traumatic brain injury, what has already been elucidated is that the system plays a critical role in elimination of metabolic waste products both during normal homeostasis and after injury. The glymphatic system functionality can be altered in the context of neural injury, such as traumatic brain injury, as well as in sleep deprivation [40]. Ongoing preclinical studies are being conducted to determine if the glymphatic system is disrupted following aneurysmal SAH. ThWe researchers eexpect SAH to cause a significant disruption in glymphatic flow. How this knowledge can be utilized for enhancing treatment after SAH is unclear but will likely be of value clinically and therapeutically. Agents that can restore glymphatic flow will be of value clinically. Another challenge with regards to modulating inflammation is the fact that inflammation is often observed to be biphasic in nature, with elements that are both protective as well as deleterious. Identifying this temporal relationship and when to target involved pathways for therapeutic benefit remains a substantial challenge. The magnitude of the inflammatory response may dictate outcome, and warrants further investigation with preclinical models. Advanced neuroimaging may offer a viable option to detect biphasic peaks in the neuroinflammatory cascade. Finally, utilizing current knowledge regarding SAH pathophysiology offers clear advantages therapeutically. For example, patients with the haptoglobin α1–α1 subunit compared to the haptoglobin α2–α2 subunit have decreased risk of CV following aneurysmal SAH, indicating a potential therapeutic target [41].3. Secondary Outcomes
3.1. Cerebral Vasospasm
Aneurysmal SAH can lead to CV, which is the narrowing of blood vessels within the subarachnoid space of the brain [42]. It is a serious complication often experienced by aneurysmal SAH survivors [43][44][43,44]. If CV persists, insufficient blood flow reaches affected regions of the brain, causing delayed cerebral ischemia [45]. CV is characterized by progressive narrowing of cerebral arteries beginning no earlier than day three following hemorrhage and peaking at one week [46]. Clinically, CV leads to delayed cerebral ischemia and infarction in 20%–30% of patients [47]. While the etiology of CV remains unknown, spasmogenic and neuroinflammatory substances generated from the lysis of subarachnoid blood are thought to drive the process [48]. Given that few treatments effectively target CV, novel murine models have been developed to further elucidate the mechanisms that regulate CV. Specifically, models have been designed to simulate vasodilatory mechanisms of the cerebral vasculature [49][50][51][52][49,50,51,52]. One mouse model involves endovascular perforation of the middle cerebral artery to produce the hemorrhage [51][52][51,52]. Another CV model consists of injecting femoral arterial blood intradurally through the atlanto-occipital membrane [50]. A canine model has been established with double hemorrhage that reliably produces CV [53]. Although all the models generate vascular changes consistent with CV, the endovascular perforation model is much more lethal, with a mortality of 29% [51][52][51,52], compared to the 3% in the intradural injection model [50].3.2. CV and Inflammation
Growing evidence supports a role for neuroinflammation in the pathogenesis of CV [48][54][48,54]. Preclinical models of CV have repeatedly demonstrated the presence of cytokine upregulation and neutrophil activation. Active neutrophils can promote reactive oxygen species formation, which has been implicated in vascular pathology [55]. Further work needs to be done in order to elucidate the mechanisms by which these neutrophils are recruited to the site of rupture. In human clinical studies, the cerebrospinal fluid (CSF) neutrophil percentage is an independent predictor of CV in SAH patients [55]. Specifically, a CSF neutrophil content of >62% on day three following a SAH serves as an independent predictor for developing CV [55]. Therefore, the resulting neutrophil-mediated inflammatory process offers a potential therapeutic window for the treatment and prevention of CV. While specific cell types may have unique roles in initiating CV, shared signaling pathways within these distinct populations may converge on common downstream effectors to drive CV. Heme released from hemoglobin has been shown in a preclinical model to promote a significant neuroinflammatory response, in part through signaling via toll-like receptor 4 (TLR4) [56][57][56,57]. TLR4 subsequently interacts with downstream effectors to generate a bimodal nuclear factor kappa beta (NFκB)-dependent inflammatory response (Figure 1) [58][59][60][58,59,60]. TLR4−/− mice demonstrate a significant reduction in CV following SAH when compared to wild-type mice. Interestingly, TLR4 agonists alter the degree of CV in TLR4−/− mice such that it mimics wild-type mice [58]. Furthermore, attenuation of the TLR4 and NFκB-dependent inflammatory response reduced the expression of downstream pro-inflammatory factors and provided a neuroprotective role in an aneurysmal SAH model [61]. These studies further establish TLR4 as a critical component in the CV cascade. Although TLR4 is expressed across many cell types, it is mostly expressed in microglia during the bimodal phases of CV [58]. Depletion of microglia in vivo following SAH is able to significantly reduce the extent of CV during both phases of the cascade [58]. However, the limited clinical utility in depleting microglia is apparent. Therapeutics that can dampen the microglia response may be beneficial however in reducing this inflammatory cascade.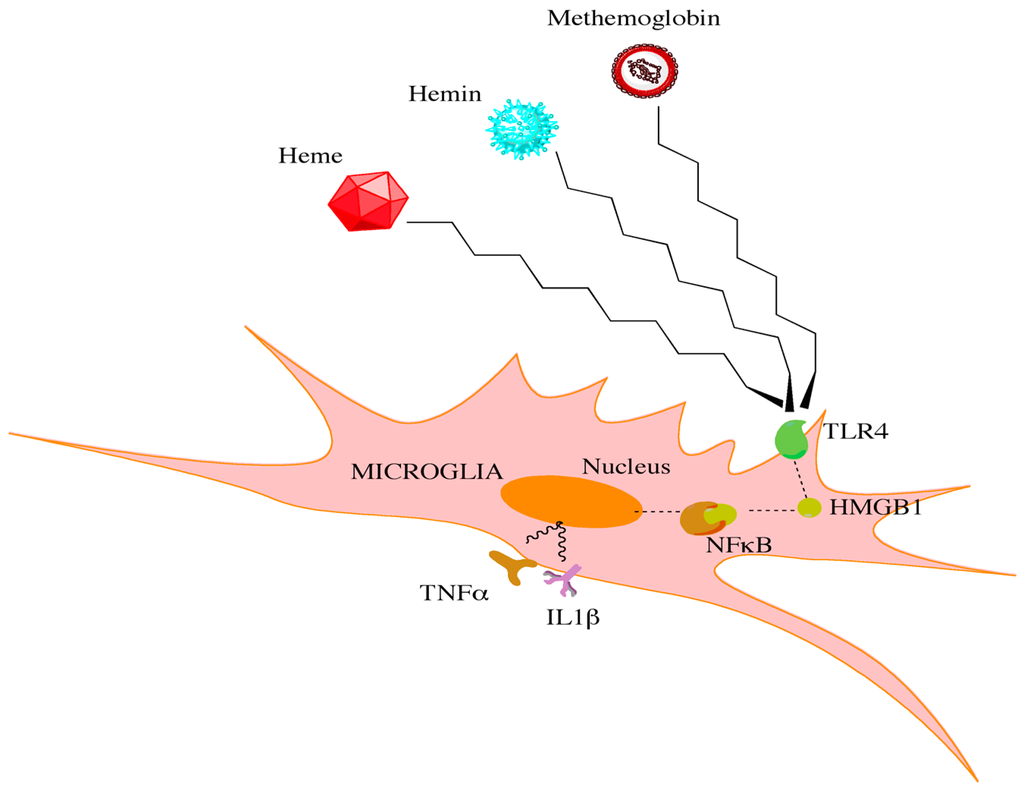
Figure 1. Red blood cell breakdown causes the release of heme, hemin, and methemoglobin. Through interactions with toll-like receptors on microglia, high mobility group box 1 protein is increased. This increase leads to downstream activation of NFκB and the release of proinflammatory cytokines.
3.3. CV and Long-Term Deficits
Whereas CV represents an acute concern in SAH patients, lasting cognitive deficits are a common long-term complication observed in aneurysmal SAH survivors [62]. SAH survivors also experience functional impairments in their ability to perform daily activities [62]. An assessment of grey- and white-matter damage following aneurysmal SAH in rats demonstrated a significant decrease in the neuronal marker microtubule-associated protein 2 and myelin basic protein, respectively [63]. Glial fibrillary acidic protein (GFAP), a marker of astrocytes, was increased in rat brains following SAH suggesting the presence of reactive gliosis [63]. Activated astrocytes can form glial scars, which are protective in the acute phase of brain injury by establishing a clear boundary between damaged and healthy tissue and thereby preventing the spread of pro-inflammatory signals throughout the brain [64][65][64,65]. However, ongoing reactive gliosis and scar formation may inhibit axonal regrowth and remyelination, further promoting grey- and white-matter damage in response to a persistent inflammatory response [66]. Targeting the chronic but not acute gliosis may be a viable treatment option worth further study. The effects of aneursymal SAH can also result in acute and long-term functional deficits in sensorimotor behavior [63]. Both mechanical sensitivity to innocuous stimuli and fine sensorimotor function were significantly impaired in SAH-induced rats when compared to sham-operated controls [63]. Therefore, it appears that the cognitive and functional deficits observed in SAH preclinical models and patients are primarily a consequence of the persistent neuroinflammatory process observed in these patients during the acute and later stages of recovery.4. Etiology and Comorbidities
4.1. Genetic Factors
Age is a determining factor of outcome following aneurysmal SAH [67]. Aged vessels are less compliant and have weak muscular walls. Premature vascular aging contributes to an increased risk of aneurysmal rupture and subsequent hemorrhage. Patients pre-disposed to epoxyeicosatrienoic acid upregulation are more at risk for vascular dysfunction and aneurysmal rupture [68][69][68,69]. Mutations in VCAN gene have also been linked to SAH [70]. Neuroinflammation severely damages already dysfunctional vessels. After rupture has occurred, mutations in the 9p21 locus on gene CDKN2A increases neuroinflammation [71]. Interleukin 6 polymorphisms can also augment neuroinflammation and can worsen SAH outcomes [72]. Interestingly, patients with the haptoglobin phenotype Hp2-2 have increased susceptibility for CV post-rupture [73], which, as discussed above, may be mediated by neuroinflammation. The apolipoprotein-ε4 allele has been associated with poor cognitive performance several years following aneursymal SAH in patients [74]. Certain polymorphisms of the A1166C gene, which regulates angiotensin II type 1 receptors, have also been correlated to worsened outcome after aneurysmal SAH [75]. These genetic associations are poorly understood in the clinical population. Pre-clinical genetic studies however have shed light on the role that neuroinflammation plays in injury progression. In a rat SAH model, high-mobility group box 1 triggers NFκB translocation thereby promoting neuroinflammation (Figure 1) [76]. The subsequent release of TNFα severely compromises vascular integrity around the site of SAH [77]. Recently, Chen and colleagues discovered that the P2X7R/cryopyrosin inflammasome axis is genetically primed in certain rodent strains, which contributes to a surge in interleukin 1β (IL-1β) following aneurysmal SAH [78]. Future clinical studies are needed to verify how these pathways are altered in patients with SAH. The sulfonylurea receptor 1-transient receptor potential melastatin 4 (Sur1-TRPM4) channel was found to be transcriptionally upregulated by Abcc8 and Trpm4 in rodents and humans following SAH [79]. This phylogenetically conserved phenomenon makes it an ideal target for pharmacologic intervention, which thwe researchers will discuss further in the concluding sections.4.2. Comorbidities and Physical Correlates
Patients with underlying comorbidities often fare worse following aneursymal SAH. Patients with migraine headaches are at increased risk for SAH [80]. Diabetes mellitus type II is associated with an increased risk for CV following SAH [81]. Patients with hypertension have larger subdural clot volumes following SAH [82]. Only recently have investigators begun to look at the mechanistic links between these comorbidities and outcome. The heart and brain are intimately connected through the vasculature and nerves. Once the brain becomes damaged from aneurysmal SAH, parasympathetic dysfunction may contribute to cardiac arrhythmias, leading to the release of inflammatory cytokines that enter the vasculature [83]. Modified vascular markers released following aneurysm rupture can interact with cytokines from damaged heart tissue and have been shown in a preclinical model to perpetuate inflammation within the brain (Figure 2) [84]. Preclinical data have shown that activated neutrophils in the peripheral vasculature can likewise damage brain microvessels following SAH [85]. Leukocyte diapedesis can occur through damaged microvessels following injury. Many peripheral immune cells migrate into the cerebral spinal fluid and the brain [86].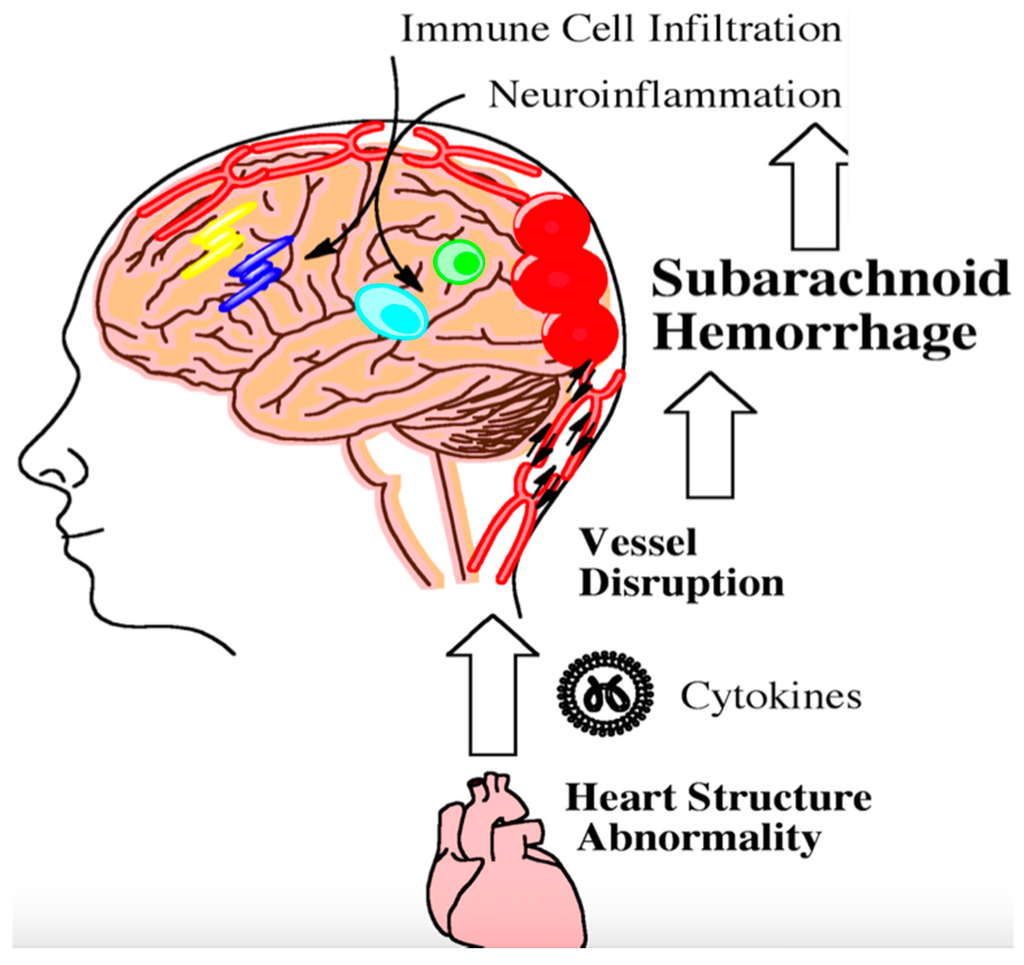
Figure 2. Following aneursym rupture, the brain stem can become ischemic and trigger heart damage. Damaged heart tissue can subsequently contribute to the inflammatory milieu following subarachnoid hemorrhage. Inflammation from heart abnormalities triggers the infiltration of peripheral immune cells into the brain as indicated by the arrows. This step-wise process further exacerbates neuroinflammation. Persistent neuroinflammation can lead to long-term cognitive and behavioral deficits.
