Knee osteoarthritis (KOA) represents a prevalent and formidable challenge in the management and treatment of musculoskeletal disorders and exerts a substantial impact on global health, particularly in the context of the natural aging process. Post-traumatic osteoarthritis (PTOA) emerges as a distinct clinical manifestation within the realm of osteoarthritis and is interwoven within the landscape of sports injuries and trauma of the joints. Within the realm of sports, athletes are frequently exposed to joint injury and acute mechanical loading that sets the biological stage for the development of PTOA.
- osteoarthritis
- post-traumatic osteoarthritis
- mechanical loading
1. Introduction
1.1. Knee Osteoarthritis
1.2. Post-Traumatic Osteoarthritis
2. Mechanotransduction
The knee joint, in its healthy state, functions as a hinge joint, which enables vital movements like flexion and extension through the interaction of articular cartilage, synovial fluid, ligaments, and menisci that allow for smooth and continuous motion of the joint. Articular cartilage, the resilient tissue covering the ends of bones, distributes mechanical forces in order to promote frictionless movement. Ligaments provide stability, while the synovial fluid lubricates and nourishes the joint. Together, these components synergize to coordinate the typical physiological processes within the knee joint that allow for seamless motion and weight-bearing activities. In the intricate milieu of KOA, the role of mechanical loading arises as a pivotal determinant in both the pathogenesis and recovery of the knee joint and is intricately linked to mechanotransduction processes. Mechanotransduction, described as the conversion of mechanical signals into biochemical responses, is paramount to understanding how mechanical loading influences the fate of articular cartilage. In the context of this revisewarch, it is critical to note that KOA pathogenesis is deeply involved with aberrations in mechanical loading, which disrupt the delicate balance of loading force required to maintain joint health. In the widely accepted pathological scenario [40,41,42,43,44,45][37][38][39][40][41][42], supramaximal mechanical forces act as a “trigger” for maladaptive responses in chondrocytes, the cells within articular cartilage [46][43]. Research conducted by Buckwalter and colleagues sheds light on the intricate relationship between mechanical loading and articular cartilage fate [46][43]. Their research emphasizes that both acute impact events and cumulative contact stress initiate the release of reactive oxygen species from mitochondria, leading to chondrocyte death and matrix degradation. Importantly, the study illuminates a substantial difference between PTOA primarily caused by acute intense joint injury and OA resulting from chronic joint instability or incongruity. Furthermore, the study describes the capacity of joints with advanced PTOA to remodel and improve with appropriate treatment, emphasizing the dynamic nature of the mechanotransduction processes involved in joint health and repair. There is ample evidence in support of Buckwalter’s research [44,47,48,49[41][44][45][46][47][48],50,51], as it is well characterized that high-impact forces exerted on the joint lead to maladaptive responses in chondrocytes and subchondral bone. As a result, chondrocytes may exhibit increased production of matrix-degrading enzymes, leading to cartilage breakdown and the activation of several inflammatory pathway cascades [38,52,53][49][50][51]. In conjunction with their pathogenic effects, mechanotransduction pathways activated by beneficial or appropriate exercise and mechanical forces stimulate the synthesis of essential extracellular matrix components, which fosters an environment that is favorable to tissue repair and injury prevention [44,54,55,56,57,58,59][41][52][53][54][55][56][57]. While promising, the linkage between mechanical loading and KOA progression requires further investigation as a therapeutic option to understand how mechanical loading can induce beneficial regenerative responses in chondrocytes [60][58]. Through this interplay, well-regulated mechanical loading emerges as a key player in the preservation and restoration of joint health in the context of KOA and PTOA.3. Mechanical Factors in PTOA
The mechanical aspects of PTOA pathogenesis involve complex interactions between joint biomechanics, tissue biology, and the body’s capacity for repair and maintenance of joint health. For example, disrupted joint biomechanics, as a result of trauma or sports injury, will disrupt the delicate balance surrounding mechanotransduction pathways. Altering either cartilage synthesis or degradation creates a mismatch that contributes to accelerated joint degeneration [61,62][59][60]. Additionally, progressive changes in load distribution within the joint due to aging or injury, whether it be from misalignment or other contributing factors, can result in abnormal stresses, leading to the breakdown of cartilage and inflammatory responses, as seen in PTOA and KOA alike [54,63,64][52][61][62]. Research has also elucidated several variables that contribute to PTOA progression, such as variations in flexion angles and resistance [29,30,65][29][30][63]. Therefore, it is crucial to understand that PTOA is complex and under active investigation. Mechanical factors, such as the type of motion and loading stress incurred by the joint, significantly influence the severity of PTOA. Previous studies shed light on the complicated relationship between loading stress and PTOA progression. A previous study, utilizing rabbit models subjected to different impact loads, demonstrated that articular cartilage could tolerate single impact loads up to 45% of the joint fracture threshold without significant disruption or degradation [66][64]. These findings emphasize not only the resilience of articular cartilage, but also highlight the potential long-term consequences of acute mechanical injury and provide a reference point for quantifying “excessive” or supramaximal joint loading. Previous studies by D’Lima et al. [67,68][65][66], focusing on knee joint forces and their impact on OA, underscore the critical role of factors like body weight, muscle contractions, and biomechanics in influencing knee forces. The research emphasizes that each additional kilogram in body weight is multiplied two or three times at the knee, contributing to increased joint loading and potentially accelerating arthritis progression. Malalignment of the lower extremity, as previously discussed, is also identified as a factor associated with the progression of osteoarthritis, which is thoroughly characterized [69,70][67][68]. D’Lima et al. [67][65] also examined knee forces during exercise and recreational activities after knee arthroplasty, providing valuable insights applicable to PTOA. Their study demonstrated, like others [71[69][70][71],72,73], that activities such as running, golf, and tennis were found to produce unexpectedly high forces, especially in the leading knee, emphasizing the need for careful consideration of post-traumatic joint health in athletes engaging in such activities. While the correlation between the increased forces incurred during high-load activities and KOA is unclear [74[72][73][74],75,76], it is evident that these activities do predispose an individual to injury of the knee [77[75][76],78], which can contribute to OA progression. Furthermore, investigation into contact stresses in the knee joint during deep flexion activities by Thambyah and colleagues revealed significantly higher peak stresses, especially in the medial compartment, during squatting, a common resistance exercise [79][77]. The study raised concerns about the adequacy of articular cartilage to support high contact stresses during deep flexion and exemplifies the need to consider mechanical factors in common exercises as contributors to the development of PTOA. Wallace and colleagues quantified patellofemoral joint reaction forces and stress during the squat maneuver and found that patellofemoral joint stress increases linearly with increasing knee flexion angle and joint force [80][78]. The addition of external resistance further elevated patellofemoral joint reaction force and stress. The study suggested that limiting terminal joint flexion angles and resistance loads could help minimize patellofemoral joint stress during squatting activities and may hinder osteoarthritis progression. These insights, among those previously discussed, emphasize the importance of considering specific motions and loading conditions in understanding the mechanical factors influencing the severity of PTOA, and exemplify the multifactorial nature of OA progression (Table 1). Prior research, employing cadaver, in vivo, and in vitro animal cartilage, revealed that chondrocyte death can be triggered by impact stress as low as 18 MPa (megapascals). Furthermore, impact stress exceeding 30 MPa was observed to inflict surface damage on cartilage, ultimately contributing to cartilage degradation [34,81,82,83,84,85,86,87][34][79][80][81][82][83][84][85]. Patellofemoral joint stress linearly correlates with joint force [80][78], with the ratio of patellofemoral joint stress to force being about 2.3 MPa per body weight according to previous studies [79,88][77][86]. It suggests that exceeding eight times the body weight in patellofemoral joint forces may lead to potential cellular injury in articular cartilage by surpassing the critical threshold of 18 MPa. Joint forces are commonly quantified in terms of body weight (BW) in exercises (see next section) and can be used as a quantitative measure to evaluate various joint loading conditions to mitigate or prevent OA.|
Study Focus |
Author, Year [Source] |
Study Type |
Number of Patients |
Study Description |
|---|---|---|---|---|
|
Impact of Athletics on Development of PTOA |
Hootman et al., 2007 [26] |
Epidemiological |
182,000 |
Summarizing injury data to identify preventable risk factors for injury prevention strategies |
|
Golightly et al., 2009 [27] |
Epidemiological |
2528 |
Describes prevalence of KOA within retired football players |
|
|
Drawer et al., 2001 [28] |
Epidemiological |
500 |
Determines the prevalence of KOA within retired soccer players |
|
|
Kujala et al., 1995 [31] |
Epidemiological |
117 |
Analyzing the impact of increased mechanical loading during sport on KOA |
|
|
Swärd et al., 2010 [32] |
Epidemiological |
331 |
Compares radiographic structural changes of KOA and PTOA in athletes v non-athletes |
|
|
Epidemiological |
20 |
Investigates the effect of running on cartilage degeneration in athletes |
||
|
Epidemiological |
825 |
Analyzes the risk of KOA development in patients with sports participation and/or injury |
||
|
Epidemiological |
258 |
Evaluates the effect of triathlon training on likelihood of future injury |
||
|
Epidemiological |
535 |
Analyzes the impact of exercise on risk of knee injury and KOA development |
||
|
Epidemiological |
16 |
Analyzes the relationship between training load and injury in football players |
||
|
Epidemiological |
875 |
Investigates the impact of marathon running on prevalence of injuries in athletes |
||
|
Epidemiological |
326 |
Investigates the effect of previous knee injury on risk of future knee injury in soccer players |
||
|
Mechanical Contributors to OA |
Gillquist et al., 1999 [29] |
Literature review |
- |
Summarizes the risk of ligamentous injury for osteoarthritis progression |
|
Epidemiological |
162 |
Analyzes the effect of malalignment in KOA progression |
||
|
Systematic review |
- |
Determines the effect of running on development of KOA |
||
|
Epidemiological |
26 |
Analyzes the long-term changes of the knee via MRI in former long-distance runners |
||
|
Systematic review |
- |
Analyzes the effect of exercise on risk of KOA |
||
|
Epidemiological |
3 |
Investigates the effects of various activities on mechanical loading in the knee joint |
||
|
Literature review |
- |
Synthesizes studies characterizing forces on the knee joint during various exercises |
||
|
In vivo |
- |
Investigates the impact of varied loading conditions on knee cartilage in rabbit models |
||
|
Systematic review |
- |
Analyzes the effect of previous knee injury on PTOA progression |
||
|
Epidemiological |
11,006 |
Characterizes the effect of malalignment on KOA progression |
||
|
Epidemiological |
229 |
Investigates biomechanical predictors of KOA progression |
||
|
Epidemiological |
4435 |
Analyzes the impact of knee pain or previous injury on the likelihood of future injury |
||
|
Systematic review |
- |
Compiles evidence for the role of inflammation in joint injury and PTOA |
||
|
Literature review |
- |
Discusses risk factors and contributing elements to dysfunction in several joints |
||
|
In vivo |
- |
Evaluate effect of lessened mechanical loading on KOA in mouse model |
||
|
Systematic review |
- |
Summarize the biological underpinnings of the effect mechanical loading on KOA |
||
|
In vitro * |
5 |
Investigates the impact of mechanical loading on gene expression within chondrocytes in OA and non-OA patient samples |
||
|
Epidemiological |
237 |
Investigates the impact of alignment on KOA progression |
||
|
Systematic review |
- |
Analyzes the correlation between malalignment and KOA progression |
||
|
Systematic review |
- |
Summarizes current evidence on the effect of hip muscle weakness in KOA patients |
||
|
In vivo |
- |
Analyzes the effect of mechanical loading on subchondral bone, cartilage, and KOA |
||
|
Epidemiological |
38 |
Evaluates the effect of increased mechanical loading of functional scores of KOA patients |
||
|
Milentijevic 2005 [34] |
In vivo |
- |
Investigates the impact of loading stress on rabbit articular cartilage |
|
|
Roos et al., 1998 [30] |
Epidemiological |
123 |
Determining the effect of meniscal surgery/removal on osteoarthritis progression |
|
|
Therapeutic Potential of Mechanical Loading |
Epidemiological |
12 |
Analyzing the impact of strength-training regimen on muscle development |
|
|
In vitro * |
8 |
Investigates gene expression of human chondrocytes following total knee replacement |
||
|
Epidemiological |
45 |
Analyzes the impact of varied training loads on risk of future injury |
||
|
Systematic review |
- |
Investigates the impact of lateral wedge insoles in patients with KOA |
||
|
Epidemiological |
10 |
Analyzes the benefit of knee brace on minimizing force at the knee joint |
||
|
Epidemiological |
10 |
Investigates the impact of knee brace and orthoses in KOA treatment |
||
|
Epidemiological |
8 |
Investigates the effect of malalignment on KOA progression |
||
|
Epidemiological |
102 |
Compares the effects of high and low load training regimens on KOA functional scores |
||
|
Epidemiological |
89 |
Investigates the effect of water training (low load bearing) on KOA progression |
||
|
Epidemiological |
42 |
Analyzes the effect of quadriceps strengthening on KOA functional scores |
||
|
Epidemiological |
41 |
Analyzes variance in water v. land conditions while performing various exercises in KOA |
||
|
Epidemiological |
35 |
Investigates the effect of varied training regimens on risk of future injury |
||
|
Literature review |
- |
Summarizes the impact of loading conditions on risk of injury, and injury prevention |
||
|
Quantification of Mechanical Forces in Rehabilitation Exercises |
In vitro * |
5 |
Quantifies mechanical forces present at knee joint during walking |
|
|
In vitro * |
4 |
Analyzes mechanical forces present on knee joint during various malalignment conditions |
||
|
Computer model |
- |
Utilizes walking simulation to determine the muscles involved in walking |
||
|
In vivo |
- |
Quantifies mechanical forces during compression to elucidate beneficial loading range |
||
|
Systematic review |
- |
Analyzes the mechanical loading force of OKC and CKC exercises at the knee joint |
||
|
Computer models |
- |
Utilizes computer simulated models to analyze forces on the knee joint during leg extension |
||
|
Epidemiological |
10 |
Quantifies mechanical force at the knee joint during squat, knee extension, and leg press |
||
|
Literature review |
- |
Discusses the mechanical forces incurred at the knee joint during the squat |
||
|
Literature review |
- |
Summarizes the mechanical load incurred during the squat |
||
|
Literature review |
- |
Summarizes the mechanical load during various rehabilitation exercises |
||
|
Epidemiological |
15 |
Quantifies patellofemoral joint forces during the squat |
* Denotes that in vitro samples were conducted on clinical patient samples.
4. The Goldilocks Zone
Establishing a Goldilocks zone of loading that preserves joint health while preventing or mitigating joint injury is an essential step for developing strategies to prevent and treat PTOA (Figure 1). As delineated by Sokoloff’s excellent aphorism in 1969 [120][118], “cartilage can survive in a large range of solicitations, but below or beyond, it will suffer”, illuminating the ideal range of mechanical loading is pivotal for optimizing joint health and the management of PTOA. Studies have described, in-depth and through varied language [121,122][119][120], what wthe researchers are referring to as the Goldilocks zone. A 2016 International Olympic Committee (IOC) publication [110][108] critically analyzed the effects of underloading and overloading on athlete injury and performance. Within their discussion, the IOC cites evidence demonstrating the counterbalance between the increased risk of injury in athletes training with sub-competition loads [89[87][89][90][107],91,92,109], and the increased risk of injury with sustained, high-intensity loads [26,90,94,123,124][26][88][92][121][122]. Interestingly, however, the IOC also cites evidence demonstrating a beneficial effect of high-intensity loading on injury prevention [91,100,109,125][89][98][107][123]. This, in essence, demonstrates that high-intensity loading in the Goldilocks zone could prevent joint injury and damage, whereas exhibiting opposite effects outside the zone. Therefore, integrating the current knowledge from mechanobiology studies of knee joints into rehabilitation programs allows us to define the Goldilocks zone as a guide for the development of targeted exercises that optimize beneficial mechanical forces, fostering tissue repair and functional improvement.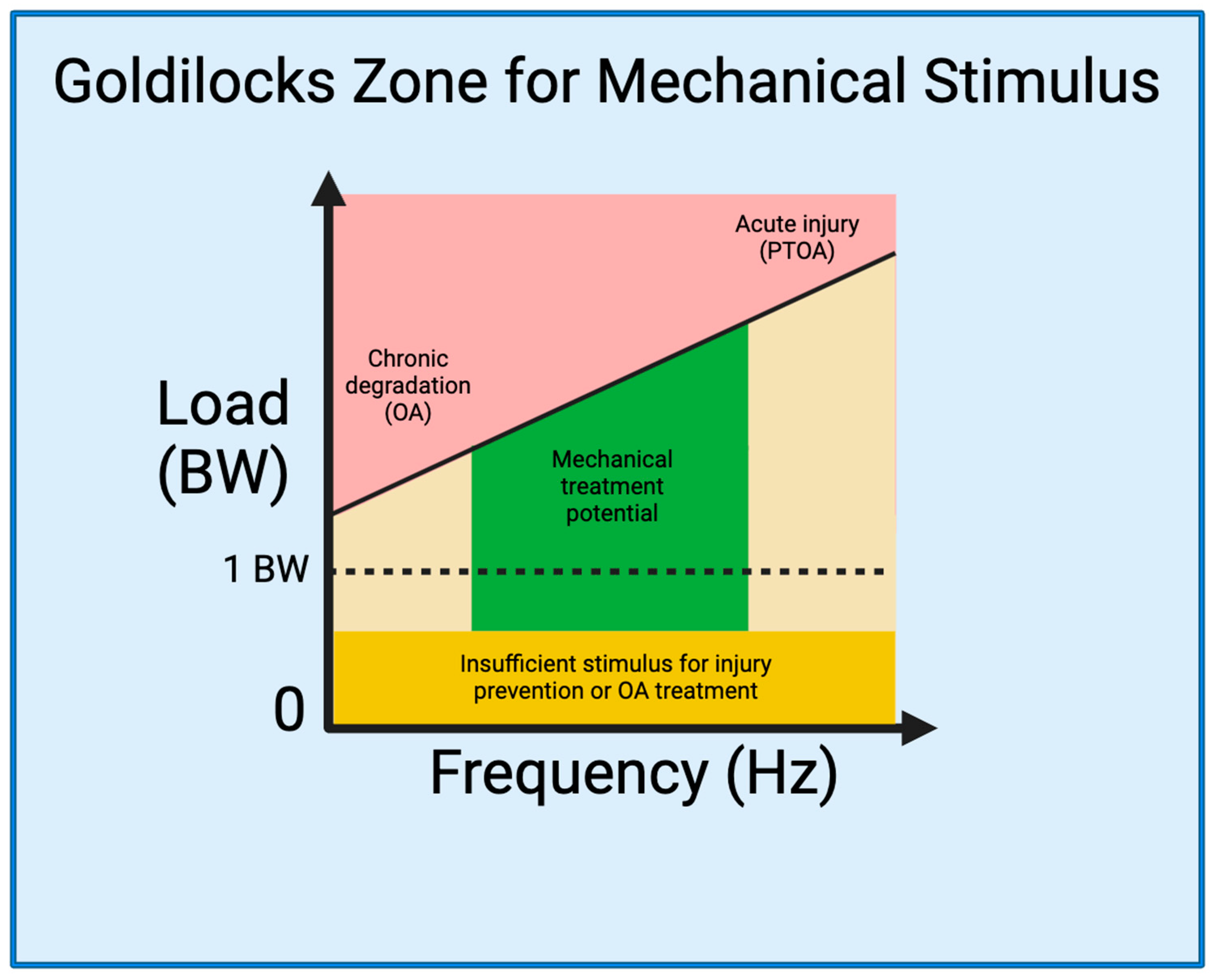
References
- Yang, G.; Wang, J.; Liu, Y.; Lu, H.; He, L.; Ma, C.; Zhao, Z. Burden of Knee Osteoarthritis in 204 Countries and Territories, 1990–2019: Results From the Global Burden of Disease Study 2019. Arthritis Care Res. 2023, 75, 2489–2500.
- Deshpande, B.R.; Katz, J.N.; Solomon, D.H.; Yelin, E.H.; Hunter, D.J.; Messier, S.P.; Suter, L.G.; Losina, E. Number of Persons With Symptomatic Knee Osteoarthritis in the US: Impact of Race and Ethnicity, Age, Sex, and Obesity. Arthritis Care Res. 2016, 68, 1743–1750.
- Felson, D.T.; Naimark, A.; Anderson, J.; Kazis, L.; Castelli, W.; Meenan, R.F. The prevalence of knee osteoarthritis in the elderly. the framingham osteoarthritis study. Arthritis Rheum. 1987, 30, 914–918.
- Sudo, A.; Miyamoto, N.; Horikawa, K.; Urawa, M.; Yamakawa, T.; Yamada, T.; Uchida, A. Prevalence and risk factors for knee osteoarthritis in elderly Japanese men and women. J. Orthop. Sci. 2008, 13, 413–418.
- Ji, S.; Liu, L.; Li, J.; Zhao, G.; Cai, Y.; Dong, Y.; Wang, J.; Wu, S. Prevalence and factors associated with knee osteoarthritis among middle-aged and elderly individuals in rural Tianjin: A population-based cross-sectional study. J. Orthop. Surg. Res. 2023, 18, 266.
- Saase, J.L.v.; Romunde, L.K.v.; Cats, A.; Vandenbroucke, J.P.; Valkenburg, H.A. Epidemiology of osteoarthritis: Zoetermeer survey. Comparison of radiological osteoarthritis in a Dutch population with that in 10 other populations. Ann. Rheum. Dis. 1989, 48, 271–280.
- Heidari, B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Casp. J. Intern. Med. 2011, 2, 205–212.
- Robinson, D.L.; Kersh, M.E.; Walsh, N.C.; Ackland, D.C.; de Steiger, R.N.; Pandy, M.G. Mechanical properties of normal and osteoarthritic human articular cartilage. J. Mech. Behav. Biomed. Mater. 2016, 61, 96–109.
- Donell, S. Subchondral bone remodelling in osteoarthritis. EFORT Open Rev. 2019, 4, 221–229.
- Sanchez-Lopez, E.; Coras, R.; Torres, A.; Lane, N.E.; Guma, M. Synovial inflammation in osteoarthritis progression. Nat. Rev. Rheumatol. 2022, 18, 258–275.
- Kean, W.F.; Kean, R.; Buchanan, W.W. Osteoarthritis: Symptoms, signs and source of pain. Inflammo. Pharmacol. 2004, 12, 3–31.
- Cicuttini, F.M.; Spector, T.D. Genetics of osteoarthritis. Ann. Rheum. Dis. 1996, 55, 665–667.
- Spector, T.D.; MacGregor, A.J. Risk factors for osteoarthritis: Genetics11supported by Procter & Gamble Pharmaceuticals, Mason, OH. Osteoarthr. Cartil. 2004, 12, 39–44.
- Vrezas, I.; Elsner, G.; Bolm-Audorff, U.; Abolmaali, N.; Seidler, A. Case–control study of knee osteoarthritis and lifestyle factors considering their interaction with physical workload. Int. Arch. Occup. Environ. Health 2010, 83, 291–300.
- Georgiev, T.; Angelov, A.K. Modifiable risk factors in knee osteoarthritis: Treatment implications. Rheumatol. Int. 2019, 39, 1145–1157.
- Connelly, A.E.; Tucker, A.J.; Kott, L.S.; Wright, A.J.; Duncan, A.M. Modifiable lifestyle factors are associated with lower pain levels in adults with knee osteoarthritis. Pain Res. Manag. 2015, 20, 389084.
- Jeong, J.N.; Kim, S.H.; Park, K.N. Relationship between objectively measured lifestyle factors and health factors in patients with knee osteoarthritis: The STROBE Study. Medicine 2019, 98, e16060.
- Rhon, D.I.; Perez, K.G.; Eskridge, S.L. Risk of post-traumatic knee osteoarthritis after knee injury in military service members. Musculoskelet. Care 2019, 17, 113–119.
- Whittaker, J.L.; Losciale, J.M.; Juhl, C.B.; Thorlund, J.B.; Lundberg, M.; Truong, L.K.; Miciak, M.; Meer, B.L.v.; Culvenor, A.G.; Crossley, K.M.; et al. Risk factors for knee osteoarthritis after traumatic knee injury: A systematic review and meta-analysis of randomised controlled trials and cohort studies for the OPTIKNEE Consensus. Br. J. Sports Med. 2022, 56, 1406–1421.
- Krakowski, P.; Karpiński, R.; Jojczuk, M.; Nogalska, A.; Jonak, J. Knee MRI Underestimates the Grade of Cartilage Lesions. Appl. Sci. 2021, 11, 1552.
- Krakowski, P.; Karpiński, R.; Maciejewski, R.; Jonak, J.; Jurkiewicz, A. Short-Term Effects of Arthroscopic Microfracturation of Knee Chondral Defects in Osteoarthritis. Appl. Sci. 2020, 10, 8312.
- Karpiński, R. Knee joint osteoarthritis diagnosis based on selected acoustic signal discriminants using machine learning. Appl. Comput. Sci. 2022, 18, 71–85.
- Chen, S.; Fu, P.; Wu, H.; Pei, M. Meniscus, articular cartilage and nucleus pulposus: A comparative review of cartilage-like tissues in anatomy, development and function. Cell Tissue Res. 2017, 370, 53–70.
- Cooper, C.; McAlindon, T.; Coggon, D.; Egger, P.; Dieppe, P. Occupational activity and osteoarthritis of the knee. Ann. Rheum. Dis. 1994, 53, 90–93.
- Anderson, J.J.; Felson, D.T. Factors Assocciated With Osteoarthritis Of The Knee In The First National Health And Nutrition Examination Survey (HANES I): Evidence For An Association With Overweight, Race, And Physical Demands Of Work. Am. J. Epidemiol. 1988, 128, 179–189.
- Hootman, J.M.; Dick, R.; Agel, J. Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. J. Athl. Train. 2007, 42, 311–319.
- Golightly, Y.M.; Marshall, S.W.; Callahan, L.F.; Guskiewicz, K. Early-onset arthritis in retired National Football League players. J. Phys. Act. Health 2009, 6, 638–643.
- Drawer, S.; Fuller, C. Propensity for osteoarthritis and lower limb joint pain in retired professional soccer players. Br. J. Sports Med. 2001, 35, 402–408.
- Gillquist, J.; Messner, K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999, 27, 143–156.
- Roos, H.; Laurén, M.; Adalberth, T.; Roos, E.M.; Jonsson, K.; Lohmander, L.S. Knee osteoarthritis after meniscectomy: Prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998, 41, 687–693.
- Kujala, U.M.; Kettunen, J.; Paananen, H.; Aalto, T.; Battié, M.C.; Impivaara, O.; Videman, T.; Sarna, S. Knee osteoarthritis in former runners, soccer players, weight lifters, and shooters. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1995, 38, 539–546.
- Swärd, P.; Kostogiannis, I.; Neuman, P.; Von Porat, A.; Boegård, T.; Roos, H. Differences in the radiological characteristics between post-traumatic and non-traumatic knee osteoarthritis. Scand. J. Med. Sci. Sports 2010, 20, 731–739.
- Anderson, D.D.; Chubinskaya, S.; Guilak, F.; Martin, J.A.; Oegema, T.R.; Olson, S.A.; Buckwalter, J.A. Post-traumatic osteoarthritis: Improved understanding and opportunities for early intervention. J. Orthop. Res. 2011, 29, 802–809.
- Milentijevic, D.; Rubel, I.F.; Liew, A.S.; Helfet, D.L.; Torzilli, P.A. An in vivo rabbit model for cartilage trauma: A preliminary study of the influence of impact stress magnitude on chondrocyte death and matrix damage. J. Orthop. Trauma 2005, 19, 466–473.
- Nyvang, J.; Hedström, M.; Gleissman, S.A. It’s not just a knee, but a whole life: A qualitative descriptive study on patients’ experiences of living with knee osteoarthritis and their expectations for knee arthroplasty. Int. J. Qual. Stud. Health Well-Being 2016, 11, 30193.
- Hunter, D.J.; Schofield, D.; Callander, E. The individual and socioeconomic impact of osteoarthritis. Nat. Rev. Rheumatol. 2014, 10, 437–441.
- Hartmann, H.; Wirth, K.; Klusemann, M. Analysis of the Load on the Knee Joint and Vertebral Column with Changes in Squatting Depth and Weight Load. Sports Med. 2013, 43, 993–1008.
- Henriksen, M.; Creaby, M.W.; Lund, H.; Juhl, C.; Christensen, R. Is there a causal link between knee loading and knee osteoarthritis progression? A systematic review and meta-analysis of cohort studies and randomised trials. BMJ Open 2014, 4, e005368.
- Robbins, S.M.; Birmingham, T.B.; Callaghan, J.P.; Jones, G.R.; Chesworth, B.M.; Maly, M.R. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Care Res. 2011, 63, 991–997.
- Guilak, F.; Hung, C.T. Physical regulation of cartilage metabolism. In Basic Orthopaedic Biomechanics; Lippincott-Raven: Philadelphia, PA, USA, 2005; pp. 259–300.
- Griffin, T.M.; Guilak, F. The Role of Mechanical Loading in the Onset and Progression of Osteoarthritis. Exerc. Sport Sci. Rev. 2005, 33, 195–200.
- Goldring, S.R.; Goldring, M.B. The role of cytokines in cartilage matrix degeneration in osteoarthritis. Clin. Orthop. Relat. Res. 2004, 427, S27–S36.
- Buckwalter, J.A.; Anderson, D.D.; Brown, T.D.; Tochigi, Y.; Martin, J.A. The roles of mechanical stresses in the pathogenesis of osteoarthritis: Implications for treatment of joint injuries. Cartilage 2013, 4, 286–294.
- Zhu, J.; Zhu, Y.; Xiao, W.; Hu, Y.; Li, Y. Instability and excessive mechanical loading mediate subchondral bone changes to induce osteoarthritis. Ann. Transl. Med. 2020, 8, 350.
- Chen, L.; Zheng, J.J.Y.; Li, G.; Yuan, J.; Ebert, J.R.; Li, H.; Papadimitriou, J.; Wang, Q.; Wood, D.; Jones, C.W.; et al. Pathogenesis and clinical management of obesity-related knee osteoarthritis: Impact of mechanical loading. J. Orthop. Transl. 2020, 24, 66–75.
- Egloff, C.; Hügle, T.; Valderrabano, V. Biomechanics and pathomechanisms of osteoarthritis. Swiss Med. Wkly. 2012, 142, w13583.
- Schröder, A.; Nazet, U.; Muschter, D.; Grässel, S.; Proff, P.; Kirschneck, C. Impact of mechanical load on the expression profile of synovial fibroblasts from patients with and without osteoarthritis. Int. J. Mol. Sci. 2019, 20, 585.
- He, Z.; Nie, P.; Lu, J.; Ling, Y.; Guo, J.; Zhang, B.; Hu, J.; Liao, J.; Gu, J.; Dai, B.; et al. Less mechanical loading attenuates osteoarthritis by reducing cartilage degeneration, subchondral bone remodelling, secondary inflammation, and activation of NLRP3 inflammasome. Bone Jt. Res. 2020, 9, 731–741.
- Cai, X.; Warburton, C.; Perez, O.F.; Wang, Y.; Ho, L.; Finelli, C.; Ehlen, Q.T.; Wu, C.; Rodriguez, C.D.; Kaplan, L.; et al. Hippo Signaling Modulates the Inflammatory Response of Chondrocytes to Mechanical Compressive Loading. bioRxiv 2023.
- Fang, T.; Zhou, X.; Jin, M.; Nie, J.; Li, X. Molecular mechanisms of mechanical load-induced osteoarthritis. Int. Orthop. 2021, 45, 1125–1136.
- Jørgensen, A.E.M.; Kjær, M.; Heinemeier, K.M. The Effect of Aging and Mechanical Loading on the Metabolism of Articular Cartilage. J. Rheumatol. 2017, 44, 410–417.
- Leong, D.J.; Sun, H.B. Mechanical loading: Potential preventive and therapeutic strategy for osteoarthritis. J. Am. Acad. Orthop. Surg. 2014, 22, 465–466.
- Galloway, M.T.; Lalley, A.L.; Shearn, J.T. The role of mechanical loading in tendon development, maintenance, injury, and repair. J. Bone Jt. Surg. Am. 2013, 95, 1620–1628.
- Frontera, W.R.; Meredith, C.N.; O’Reilly, K.P.; Knuttgen, H.G.; Evans, W.J. Strength conditioning in older men: Skeletal muscle hypertrophy and improved function. J. Appl. Physiol. 1988, 64, 1038–1044.
- Vanrenterghem, J.; Nedergaard, N.J.; Robinson, M.A.; Drust, B. Training Load Monitoring in Team Sports: A Novel Framework Separating Physiological and Biomechanical Load-Adaptation Pathways. Sports Med. 2017, 47, 2135–2142.
- Nebelung, S.; Gavenis, K.; Lüring, C.; Zhou, B.; Mueller-Rath, R.; Stoffel, M.; Tingart, M.; Rath, B. Simultaneous anabolic and catabolic responses of human chondrocytes seeded in collagen hydrogels to long-term continuous dynamic compression. Ann. Anat. Anat. Anz. 2012, 194, 351–358.
- Lin, W.Y.; Chang, Y.H.; Wang, H.Y.; Yang, T.C.; Chiu, T.K.; Huang, S.B.; Wu, M.H. The study of the frequency effect of dynamic compressive loading on primary articular chondrocyte functions using a microcell culture system. Biomed. Res. Int. 2014, 2014, 762570.
- Sanchez-Adams, J.; Leddy, H.A.; McNulty, A.L.; O’Conor, C.J.; Guilak, F. The mechanobiology of articular cartilage: Bearing the burden of osteoarthritis. Curr. Rheumatol. Rep. 2014, 16, 1–9.
- Lieberthal, J.; Sambamurthy, N.; Scanzello, C.R. Inflammation in joint injury and post-traumatic osteoarthritis. Osteoarthr. Cartil. 2015, 23, 1825–1834.
- Wang, L.-J.; Zeng, N.; Yan, Z.-P.; Li, J.-T.; Ni, G.-X. Post-traumatic osteoarthritis following ACL injury. Arthritis Res. Ther. 2020, 22, 57.
- Hunter, D.J.; Zhang, Y.; Niu, J.; Tu, X.; Amin, S.; Goggins, J.; Lavalley, M.; Guermazi, A.; Gale, D.; Felson, D.T. Structural factors associated with malalignment in knee osteoarthritis: The Boston osteoarthritis knee study. J. Rheumatol. 2005, 32, 2192–2199.
- Felson, D.T.; Niu, J.; Gross, K.D.; Englund, M.; Sharma, L.; Cooke, T.D.V.; Guermazi, A.; Roemer, F.W.; Segal, N.; Goggins, J.M.; et al. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: Findings from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Rheum. 2013, 65, 355–362.
- Whittaker, J.L.; Losciale, J.M.; Juhl, C.; Thorlund, J.B.; Lundberg, M.; Troung, L.K.; Miciak, M.; van Meer, B.L.; Culvenor, A.G.; Crossley, K.M. Risk factors for knee osteoarthritis after knee trauma: A systematic review and meta-analysis of randomised controlled trials and cohort studies for the optiknee initiative. Osteoarthr. Cartil. 2022, 30, S223–S224.
- Borrelli, J., Jr.; Zhu, Y.; Burns, M.; Sandell, L.; Silva, M.J. Cartilage tolerates single impact loads of as much as half the joint fracture threshold. Clin. Orthop. Relat. Res. 2004, 426, 266–273.
- D’Lima, D.D.; Steklov, N.; Patil, S.; Colwell Jr, C.W. The Mark Coventry Award: In vivo knee forces during recreation and exercise after knee arthroplasty. Clin. Orthop. Relat. Res. 2008, 466, 2605–2611.
- D’Lima, D.D.; Fregly, B.J.; Patil, S.; Steklov, N.; Colwell, C.W. Knee joint forces: Prediction, measurement, and significance. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2012, 226, 95–102.
- Sharma, L.; Song, J.; Felson, D.T.; Cahue, S.; Shamiyeh, E.; Dunlop, D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001, 286, 188–195.
- Tanamas, S.; Hanna, F.S.; Cicuttini, F.M.; Wluka, A.E.; Berry, P.; Urquhart, D.M. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Care Res. Off. J. Am. Coll. Rheumatol. 2009, 61, 459–467.
- Lequesne, M.G.; Dang, N.; Lane, N.E. Sport practice and osteoarthritis of the limbs. Osteoarthr. Cartil. 1997, 5, 75–86.
- Boocock, M.; McNair, P.; Cicuttini, F.; Stuart, A.; Sinclair, T. The short-term effects of running on the deformation of knee articular cartilage and its relationship to biomechanical loads at the knee. Osteoarthr. Cartil. 2009, 17, 883–890.
- Cole, M.H.; Grimshaw, P.N. The Biomechanics of the Modern Golf Swing: Implications for Lower Back Injuries. Sports Med. 2016, 46, 339–351.
- Hansen, P.; English, M.; Willick, S.E. Does Running Cause Osteoarthritis in the Hip or Knee? PMR 2012, 4, S117–S121.
- Timmins, K.A.; Leech, R.D.; Batt, M.E.; Edwards, K.L. Running and Knee Osteoarthritis: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2017, 45, 1447–1457.
- Bosomworth, N.J. Exercise and knee osteoarthritis: Benefit or hazard? Can. Fam. Physician 2009, 55, 871–878.
- James, S.L. Running Injuries to the Knee. JAAOS J. Am. Acad. Orthop. Surg. 1995, 3, 309–318.
- Thelin, N.; Holmberg, S.; Thelin, A. Knee injuries account for the sports-related increased risk of knee osteoarthritis. Scand. J. Med. Sci. Sports 2006, 16, 329–333.
- Thambyah, A.; Goh, J.C.; De, S.D. Contact stresses in the knee joint in deep flexion. Med. Eng. Phys. 2005, 27, 329–335.
- Wallace, D.A.; Salem, G.J.; Salinas, R.; Powers, C.M. Patellofemoral joint kinetics while squatting with and without an external load. J. Orthop. Sports Phys. Ther. 2002, 32, 141–148.
- Hurtig, M.; Chubinskaya, S.; Dickey, J.; Rueger, D. BMP-7 protects against progression of cartilage degeneration after impact injury. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2009, 27, 602–611.
- Rundell, S.A.; Baars, D.C.; Phillips, D.M.; Haut, R.C. The limitation of acute necrosis in retro-patellar cartilage after a severe blunt impact to the in vivo rabbit patello-femoral joint. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2005, 23, 1363–1369.
- Farquhar, T.; Xia, Y.; Mann, K.; Bertram, J.; Burton-Wurster, N.; Jelinski, L.; Lust, G. Swelling and fibronectin accumulation in articular cartilage explants after cyclical impact. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1996, 14, 417–423.
- Radin, E.L.; Burr, D.B.; Caterson, B.; Fyhrie, D.; Brown, T.D.; Boyd, R.D. Mechanical determinants of osteoarthrosis. Semin. Arthritis Rheum. 1991, 21, 12–21.
- Radin, E.L.; Martin, R.B.; Burr, D.B.; Caterson, B.; Boyd, R.D.; Goodwin, C. Effects of mechanical loading on the tissues of the rabbit knee. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1984, 2, 221–234.
- Donohue, J.M.; Buss, D.; Oegema, T.R., Jr.; Thompson, R.C., Jr. The effects of indirect blunt trauma on adult canine articular cartilage. J. Bone Jt. Surg. Am. Vol. 1983, 65, 948–957.
- Meyer, E.G.; Baumer, T.G.; Slade, J.M.; Smith, W.E.; Haut, R.C. Tibiofemoral contact pressures and osteochondral microtrauma during anterior cruciate ligament rupture due to excessive compressive loading and internal torque of the human knee. Am. J. Sports Med. 2008, 36, 1966–1977.
- Salem, G.J.; Powers, C.M. Patellofemoral joint kinetics during squatting in collegiate women athletes. Clin. Biomech. 2001, 16, 424–430.
- Shaw, T.; Howat, P.; Trainor, M.; Maycock, B. Training patterns and sports injuries in triathletes. J. Sci. Med. Sport 2004, 7, 446–450.
- Koplan, J.P.; Rothenberg, R.B.; Jones, E.L. The natural history of exercise: A 10-yr follow-up of a cohort of runners. Med. Sci. Sports Exerc. 1995, 27, 1180–1184.
- Piggott, B. The Relationship between Training Load and Incidence of Injury and Illness over a Pre-Season at an Australian Football League Club. Master’s Thesis, Edith Cowan University, Joondalup, WA, Australia, 2008.
- Satterthwaite, P.; Norton, R.; Larmer, P.; Robinson, E. Risk factors for injuries and other health problems sustained in a marathon. Br. J. Sports Med. 1999, 33, 22–26.
- Clausen, M.B.; Tang, L.; Zebis, M.K.; Krustrup, P.; Hölmich, P.; Wedderkopp, N.; Andersen, L.L.; Christensen, K.B.; Møller, M.; Thorborg, K. Self-reported previous knee injury and low knee function increase knee injury risk in adolescent female football. Scand. J. Med. Sci. Sports 2016, 26, 919–926.
- Schueller-Weidekamm, C.; Schueller, G.; Uffmann, M.; Bader, T. Incidence of chronic knee lesions in long-distance runners based on training level: Findings at MRI. Eur. J. Radiol. 2006, 58, 286–293.
- D’Lima, D.D.; Patil, S.; Steklov, N.; Slamin, J.E.; Colwell, C.W., Jr. Tibial forces measured in vivo after total knee arthroplasty. J. Arthroplast. 2006, 21, 255–262.
- Aljehani, M.S.; Christensen, J.C.; Snyder-Mackler, L.; Crenshaw, J.; Brown, A.; Zeni, J.A., Jr. Knee biomechanics and contralateral knee osteoarthritis progression after total knee arthroplasty. Gait Posture 2022, 91, 266–275.
- Driban, J.B.; Lo, G.H.; Eaton, C.B.; Price, L.L.; Lu, B.; McAlindon, T.E. Knee pain and a prior injury are associated with increased risk of a new knee injury: Data from the osteoarthritis initiative. J. Rheumatol. 2015, 42, 1463–1469.
- September, A.V.; Schwellnus, M.P.; Collins, M. Tendon and ligament injuries: The genetic component. Br. J. Sports Med. 2007, 41, 241–246.
- Raghava Neelapala, Y.V.; Bhagat, M.; Shah, P. Hip Muscle Strengthening for Knee Osteoarthritis: A Systematic Review of Literature. J. Geriatr. Phys. Ther. 2020, 43, 89–98.
- Veugelers, K.R.; Young, W.B.; Fahrner, B.; Harvey, J.T. Different methods of training load quantification and their relationship to injury and illness in elite Australian football. J. Sci. Med. Sport 2016, 19, 24–28.
- Baert, I.A.; Nijs, J.; Meeus, M.; Lluch, E.; Struyf, F. The effect of lateral wedge insoles in patients with medial compartment knee osteoarthritis: Balancing biomechanics with pain neuroscience. Clin. Rheumatol. 2014, 33, 1529–1538.
- Fantini Pagani, C.H.; Hinrichs, M.; Brüggemann, G.P. Kinetic and kinematic changes with the use of valgus knee brace and lateral wedge insoles in patients with medial knee osteoarthritis. J. Orthop. Res. 2012, 30, 1125–1132.
- Robert-Lachaine, X.; Dessery, Y.; Belzile, É.L.; Corbeil, P. Knee braces and foot orthoses multimodal treatment of medial knee osteoarthritis. Gait Posture 2022, 96, 251–256.
- Barrios, J.A.; Crossley, K.M.; Davis, I.S. Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment. J. Biomech. 2010, 43, 2208–2213.
- Jan, M.-H.; Lin, J.-J.; Liau, J.-J.; Lin, Y.-F.; Lin, D.-H. Investigation of Clinical Effects of High- and Low-Resistance Training for Patients With Knee Osteoarthritis: A Randomized Controlled Trial. Phys. Ther. 2008, 88, 427–436.
- Kunduracilar, Z.; Guvenir Sahin, H.; Sonmezer, E.; Sozay, S. The effects of two different water exercise trainings on pain, functional status and balance in patients with knee osteoarthritis. Complement. Ther. Clin. Pract. 2018, 31, 374–378.
- Tagesson, S.; Oberg, B.; Good, L.; Kvist, J. A comprehensive rehabilitation program with quadriceps strengthening in closed versus open kinetic chain exercise in patients with anterior cruciate ligament deficiency: A randomized clinical trial evaluating dynamic tibial translation and muscle function. Am. J. Sports Med. 2008, 36, 298–307.
- Heywood, S.; McClelland, J.; Geigle, P.; Rahmann, A.; Villalta, E.; Mentiplay, B.; Clark, R. Force during functional exercises on land and in water in older adults with and without knee osteoarthritis: Implications for rehabilitation. Knee 2019, 26, 61–72.
- Vleck, V.E.; Bentley, D.J.; Millet, G.P.; Cochrane, T. Triathlon Event Distance Specialization: Training and Injury Effects. J. Strength Cond. Res. 2010, 24, 30–36.
- Soligard, T.; Schwellnus, M.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R. How much is too much?(Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041.
- Wong, J.; Steklov, N.; Patil, S.; Flores-Hernandez, C.; Kester, M.; Colwell, C.W., Jr.; D’Lima, D.D. Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J. Orthop. Res. 2011, 29, 347–353.
- Sasaki, K.; Neptune, R.R. Individual muscle contributions to the axial knee joint contact force during normal walking. J. Biomech. 2010, 43, 2780–2784.
- Holyoak, D.T.; Chlebek, C.; Kim, M.J.; Wright, T.M.; Otero, M.; van der Meulen, M.C.H. Low-level cyclic tibial compression attenuates early osteoarthritis progression after joint injury in mice. Osteoarthr. Cartil. 2019, 27, 1526–1536.
- Glass, R.; Waddell, J.; Hoogenboom, B. The Effects of Open versus Closed Kinetic Chain Exercises on Patients with ACL Deficient or Reconstructed Knees: A Systematic Review. N. Am. J. Sports Phys. Ther. 2010, 5, 74–84.
- Bini, R.R. Patellofemoral and tibiofemoral forces during knee extension: Simulations to strength training and rehabilitation exercises. Fisioter. Em. Mov. 2017, 30, 267–275.
- Escamilla, R.F.; Fleisig, G.S.; Zheng, N.; Barrentine, S.W.; Wilk, K.E.; Andrews, J.R. Biomechanics of the knee during closed kinetic chain and open kinetic chain exercises. Med. Sci. Sports Exerc. 1998, 30, 556–569.
- Escamilla, R.F. Knee biomechanics of the dynamic squat exercise. Med. Sci. Sports Exerc. 2001, 33, 127–141.
- Schoenfeld, B.J. Squatting kinematics and kinetics and their application to exercise performance. J. Strength Cond. Res. 2010, 24, 3497–3506.
- Perez, J.; Kaplan, L.; C Huang, C.-Y. Mechanical Injury of Knee Articular Cartilage in Sports-Related Exercise and Potential Post-Injury Preventative Therapy. Curr. Tissue Eng. (Discontin.) 2015, 4, 67–76.
- Sokoloff, L. The biology of degenerative joint disease. Perspect. Biol. Med. 1963, 7, 94–106.
- Gabbett, T.J. The training—Injury prevention paradox: Should athletes be training smarter and harder? Br. J. Sports Med. 2016, 50, 273–280.
- Fry, R.W.; Morton, A.R.; Keast, D. Overtraining in athletes: An update. Sports Med. 1991, 12, 32–65.
- Bovens, A.; Janssen, G.; Vermeer, H.; Hoeberigs, J.; Janssen, M.; Verstappen, F. Occurrence of running injuries in adults following a supervised training program. Int. J. Sports Med. 1989, 10, S186–S190.
- Van Middelkoop, M.; Kolkman, J.; Van Ochten, J.; Bierma-Zeinstra, S.; Koes, B.W. Risk factors for lower extremity injuries among male marathon runners. Scand. J. Med. Sci. Sports 2008, 18, 691–697.
- Orchard, J.W.; Blanch, P.; Paoloni, J.; Kountouris, A.; Sims, K.; Orchard, J.J.; Brukner, P. Cricket fast bowling workload patterns as risk factors for tendon, muscle, bone and joint injuries. Br. J. Sports Med. 2015, 49, 1064–1068.
- Hao, X.; Wang, S.; Zhang, J.; Xu, T. Effects of body weight-supported treadmill training on cartilage-subchondral bone unit in the rat model of posttraumatic osteoarthritis. J. Orthop. Res. 2021, 39, 1227–1235.
- Hazbun, L.; Martinez, J.A.; Best, T.M.; Kaplan, L.; Huang, C.Y. Anti-inflammatory effects of tibial axial loading on knee articular cartilage post traumatic injury. J. Biomech. 2021, 128, 110736.
