You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Catherine Yang and Version 1 by Sascha Ott.
Pectoralis nerve blocks, serratus anterior plane blocks, erector spinae plane blocks, paravertebral blocks, and parasternal blocks can provide valuable supplements in the portfolio of multi-modal analgesic approaches in chest wall pain. While the indication spectrum and covered areas for some of these blocks might overlap, the feasibility and, thereby, the choice of one of these blocks might differ according to the specifics of the concrete ICU patient.
- regional anesthesia
- peripheral nerve blocks
- chest wall blocks
- abdominal wall blocks
1. Pectoralis Nerve Block
1.1. How to Perform the Block
The patient is supine with the arm abducted at 90 degrees or at the side. The ultrasound probe is positioned under the clavicle at the midclavicular line to locate the axillary artery and vein beneath the pectoralis major and minor muscles. Subsequently, the probe is shifted in a distal and lateral direction while visualizing the ribs as a reference point, moving it toward the axilla (Figure 1). At the level of the third and fourth rib, the major and minor pectoralis muscle and the thoracoacromial artery’s pectoral branch can be identified. For PECS I, the needle is inserted in-plane in a medial to lateral direction until the tip enters the fascial plane between the pectoralis major and minor muscle. To achieve PECS II, the needle is then further advanced to the plane between the pectoralis minor and serratus muscles. Volumes of LA are indicated in Table 1.
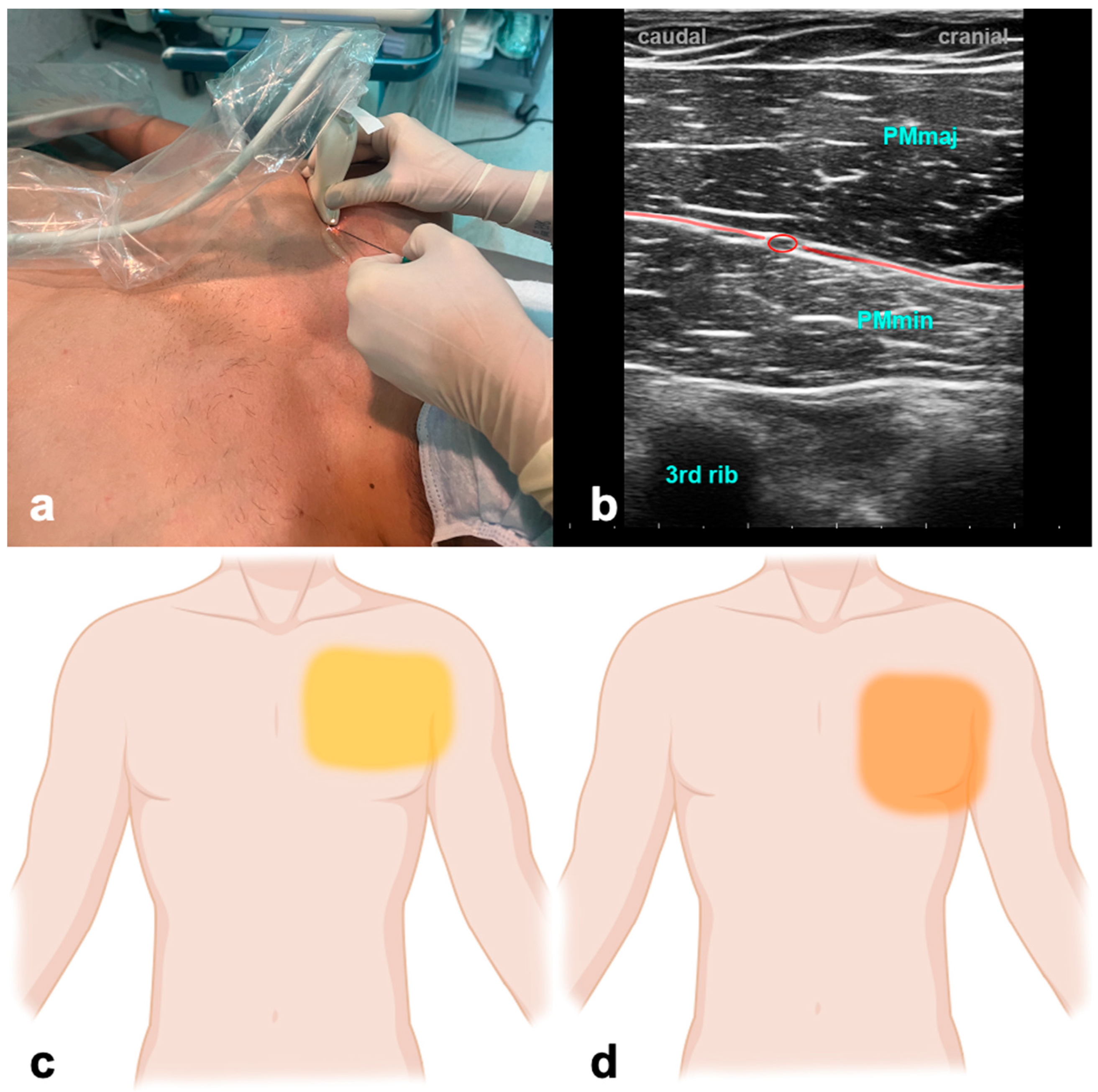
Figure 1. Pectoralis nerve block. (a) Transducer positioning. (b) Ultrasound anatomy of PECS I: PMmaj—pectoralis major muscle; PMmin—pectoralis minor muscle; red circle—pectoral branch of thoracoacromial artery; red line target space for PECS I block. (c) Spread of PECS I. (d) Spread of PECS II.
Table 1.
Recommendations of local anesthetics and dosages for PNB/FPB.
| PNB/FPB | Dosage Recommendation |
| PECS I | Bupivacaine 0.25% or Ropivacaine 0.5%: 10 mL |
| PECS II | Bupivacaine 0.25% or Ropivacaine 0.5%: 20 mL |
| SAPB | Bupivacaine 0.25%: 30–40 mL Continuous Catheter Infusion: Ropivacaine 0.2%: 6–10 mL/h; Bolus 8 mL; Lockout interval 30 min |
| ESPB | Bupivacaine 0.25% or Ropivacaine 0.5% Unilateral: 50–70 kg: 30 mL; ≥70 kg: 40 mL Bilateral (each side): 50–70 kg: 20 mL; ≥70–100 kg: 25 mL; ≥100 kg: 30 mL Continuous Catheter Infusion: Ropivacaine 0.2%: 8–10 mL/h; Bolus 5 mL, Lockout interval 60 min Alternative: Intermittent Bolus of 15 mL each 2–3 h |
| PIFB/TTPB | Bupivacaine 0.25% or Ropivacaine 0.5%: 20 mL/side |
| Intercostal Block | Ropivacaine 0.2%: 3–5 mL per level |
| TAPB | Bupivacaine 0.25% or Ropivacaine 0.5%: 20 mL Continuous Catheter Infusion: Ropivacaine 0.2%: 6–10 mL/h; Bolus 12 mL; Lockout interval 60 min |
PNB—paravertebral nerve block; FPB—fascial plane block; PECS—pectoralis nerve block; SAPB—serratus anterior plane block; EPSB—erector spinae plane block; PIFB—pecto-intercostal fascial block; TTPB—Transversus Thoracic Plane Block; TAPB—transversus abdominis plane block. Dosage recommendations according local standards.
1.2. Evidence and Indications
No studies have addressed PECS blocks in ICU patients, and the available evidence in the perioperative setting is inconsistent. However, PECS II was beneficial compared to systemic analgesia alone in mastectomy [36,37,38][1][2][3] but failed to improve postoperative analgesia or cumulative opioid consumption after robotically assisted mitral valve repair [39][4]. An ongoing trial evaluates the impact of PECS II blockade in patients undergoing minimally invasive cardiac surgery [40][5]. PEC blocks affect the intercostobrachial and intercostal nerve distribution, at T3–T6, and the long thoracic nerve, which together innervate the anterolateral chest and adjacent axilla.
1.3. Why the ICU Physician Could Love It
Postoperative pain resulting from thoracic and breast surgeries often poses challenges, impacting patients’ ability to take deep breaths and contributing to substantial morbidity. Performing PECS blocks is a favorable option due to the accessible anatomy and the relative safety afforded by the ribs shielding against an inadvertent puncture of the pleura.
2. Serratus Anterior Plane Block
2.1. How to Perform the Block
The ultrasound transducer is positioned in the mid-axillary line in the transverse plane at the level of the fifth rib (Figure 2). The USG landmarks are the ribs, pleural lines, and serratus anterior and latissimus dorsi muscles. The needle is advanced in-plane towards the fifth rib, and the LA is applied above the serratus muscle for a superficial SAPB and anteriorly to the rib and deep into the serratus muscle for a deep SAPB. Volumes of LA are indicated in Table 1.
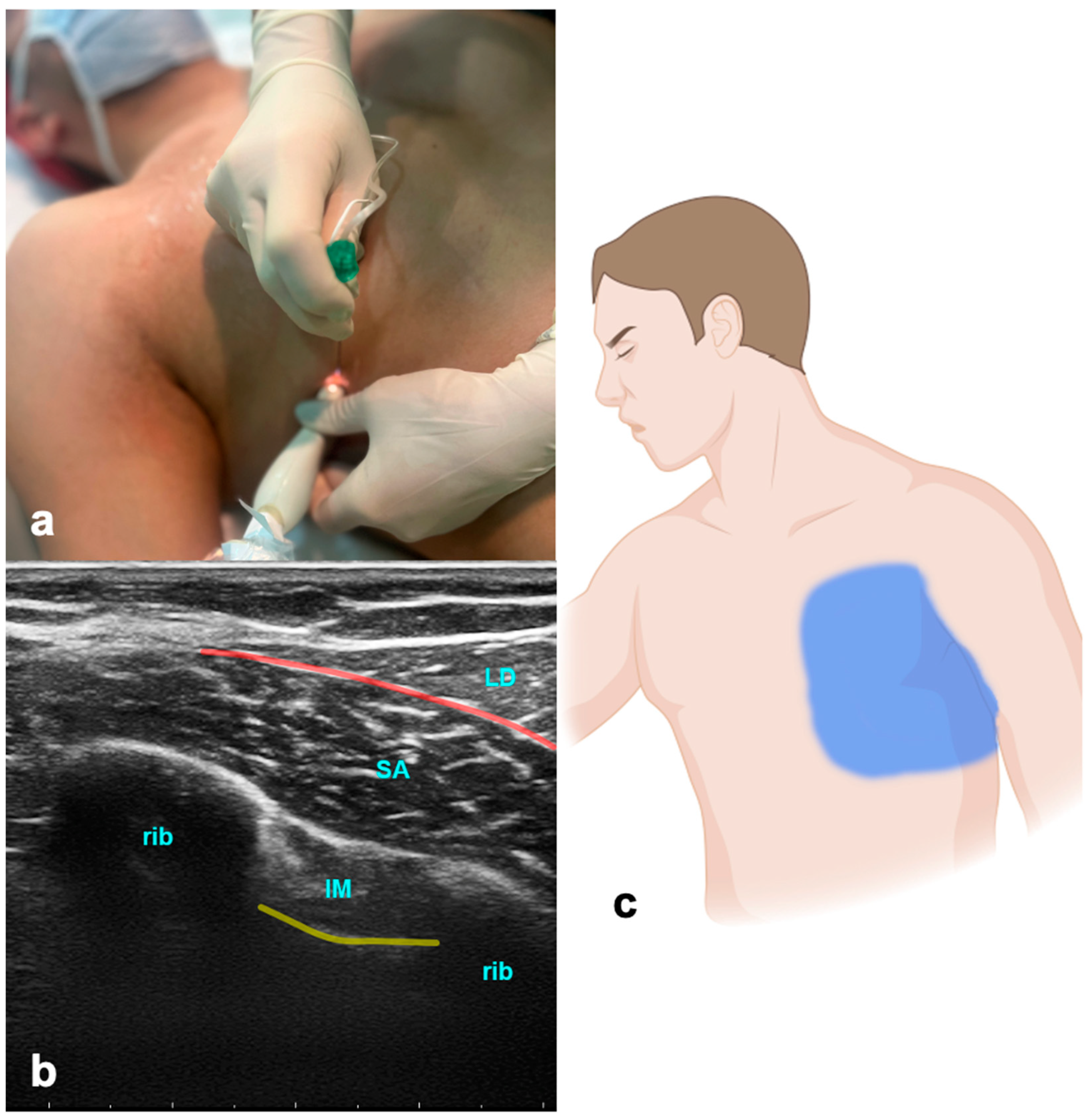
Figure 2. Serratus anterior plane block. (a) Transducer positioning. (b) Ultrasound anatomy of SAPB: LD—latissimus dorsi muscle; SA—serratus anterior muscle; IM—intercostal muscle; yellow line—pleura; red line—target space for SAPB. (c) Spread of SAPB.
2.2. Evidence and Indications
The serratus anterior plane block (SAPB) has been used effectively in managing pain in rib fractures [41][6], thoracic surgery [42][7], breast surgery, and post-mastectomy pain syndrome [43,44][8][9]. Data from a small study suggest that the SAPB is equally suitable for managing pain in patients with rib fractures compared to epidural and paravertebral blocks [45][10]. Another study showed a continuous SAPB to be similarly effective in pain control compared to intravenous fentanyl in rib-fractured patients, with superior early mobilization and shorter ICU lengths of stay [46][11]. In a recent meta-analysis, the SAPB was shown to reduce both pain scores and 24 h postoperative opioid consumption [47][12]. The SAPB is a safe and effective alternative for thoracic epidural analgesia (TEA) for postoperative analgesia after thoracotomy [48][13]. However, the erector spinae plane block (ESPB) was superior to the SAPB in the pain management of patients with lung cancer undergoing posterolateral thoracotomy [49][14]. The block effectively anesthetizes the lateral cutaneous branches of the intercostal nerves, which emerge between the layers of muscles. Additionally, it provides anesthesia to the long thoracic, thoracodorsal, and intercostobrachial nerves and thereby may be beneficial in pain originating from intercostal drainages—a common source of pain in ICU patients.
2.3. Why the ICU Physician Could Love It
The SAPB presents notable advantages over epidural or paravertebral blocks, particularly in the context of rib fractures. Aside from distinct issues and positioning challenges associated with other blocks, the SAPB offers a relatively simpler procedure, making it a more accessible and practical choice for effective pain management.
3. Erector Spinae Plane Block
The erector spinae plane block (ESPB) is a relatively new PNB with rapidly growing popularity because it is easy to perform and offers a broad scope. The ESPB can be applied as a single block or continuous analgesic approach, offering a reliable and safer alternative to neuraxial procedures [50,51,52][15][16][17]. It has been shown that the LA applied due to an ESPB spreads to the paravertebral space, the neural foramina, and partially to the epidural space [53][18]. It can be performed on different levels and applies to thoracic and abdominal procedures.
3.1. How to Perform the Block
The patient can be in a sitting, supine, prone, or lateral decubitus position. The ultrasound probe is initially positioned longitudinally over the ribs, in the middle between the scapula and spine (Figure 3). The probe is advanced medially until first the costotransverse junction and, subsequently, the transverse process appears. The latter can be differentiated from ribs due to its more superficial, wider, and rectangular shape. The needle is inserted in a cranio-caudal direction in an in-plane technique targeting the transverse process until the tip reaches contact. LA is given to the plane between the transverse process of the thoracic or lumbar vertebra and the anterior fascia of the erector spinae muscles. Volumes of LA are indicated in Table 1.
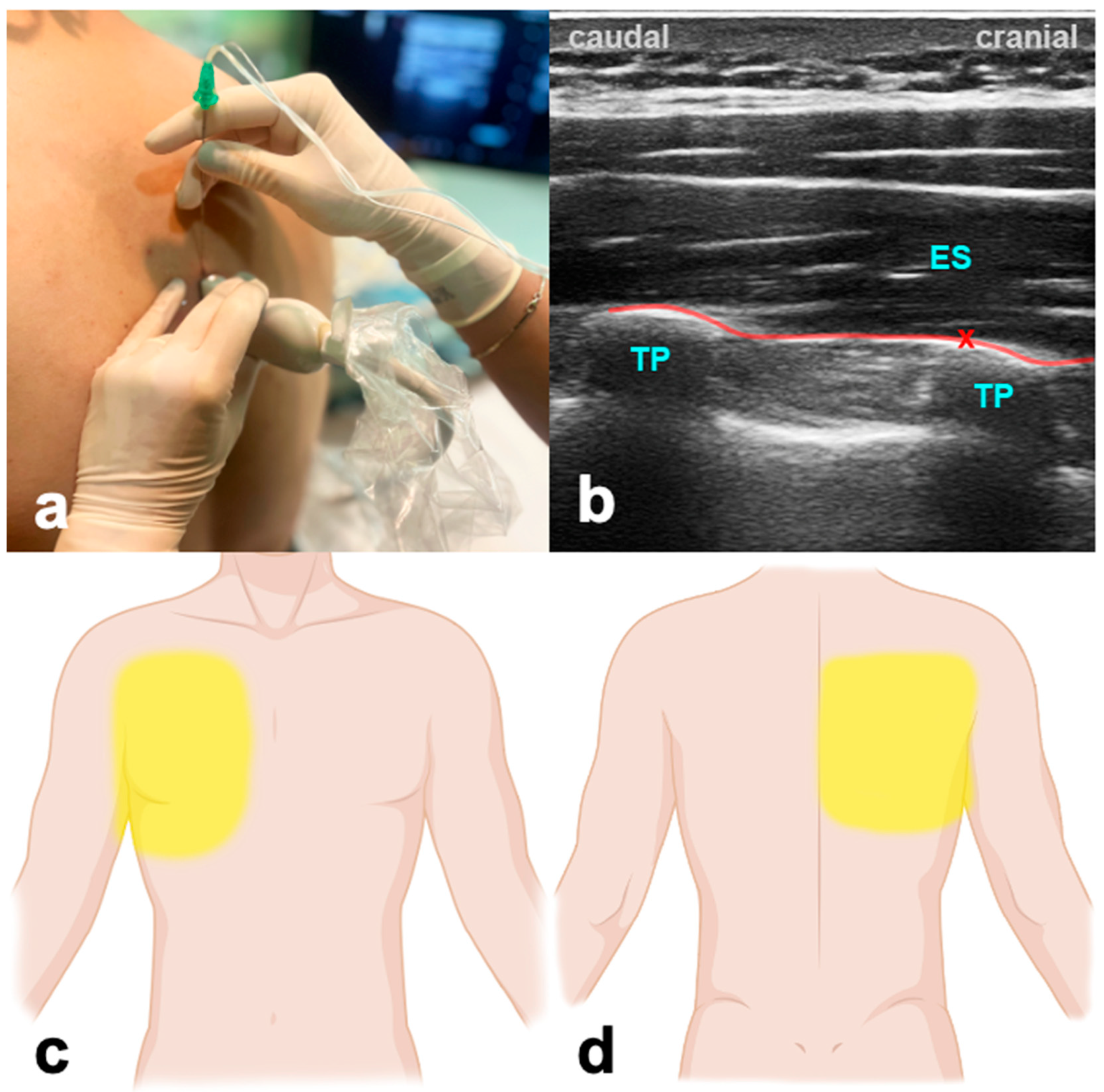
Figure 3. Erector spinae plane block. (a) Transducer positioning. (b) Ultrasound anatomy of ESPB: ES—erector spinae muscle; TP—transverse process; red cross—target point for the injection at the edge of the TP; red line—target space for ESPB. (c) Frontal spread of ESPB. (d) Dorsal spread of ESPB.
3.2. Evidence and Indications
Although the ESPB is a relatively new fascial block, there is much data available; however, most studies do not focus primarily on the ICU population. Plenty of data in cardiac surgery show that the ESPB provides opioid-sparing perioperative analgesia, facilitates early mobilization and extubation, allows earlier ICU discharge, and is superior in a multi-modal approach compared to mono-modal intravenous strategies [54,55,56,57,58][19][20][21][22][23]. The ESPB contributes to early recovery after cardiac surgery (ERACS) pathways in this context [59][24]. In addition, the ESPB is beneficial in reducing chronic postsurgical pain in CABG patients [60][25]. Beyond that, the ESPB is a valuable, low-risk, and high-success-rated tool in patients with thoracic trauma and rib fractures [61,62][26][27]. In abdominal surgery, the ESPB offers a variety of scopes. Compared to the transabdominal plane block, the bilateral ESPB was a more feasible and effective intra- and postoperative analgesia method in patients undergoing laparoscopic bariatric surgery [63][28]. A recent publication showed a significant reduction in intra- and postoperative opioid consumption, a major trigger for postoperative constipation and ileus [64][29].
3.3. Why the ICU Physician Could Love It
The ESPB can prove to be a valuable tool during the weaning and extubation of patients following thoracic procedures, especially when challenges arise due to inadequate pain control. This is particularly relevant in cases where achieving optimal pain management compromises the patient’s ability for adequate spontaneous breathing efforts, such as in lung transplant patients [65][30]. Furthermore, the EPSB provides a superior safety profile regarding the coagulation status of the patients when compared to neuraxial blocks.
4. Paravertebral Block
4.1. How to Perform the Block
When conducting paravertebral blocks, it is essential always to be aware of potential hazards, including a small risk of pneumothorax, the unintended injection of the drug into the epidural or intrathecal space, and the faster absorption of LA [66][31]. The ultrasound probe is placed in a transverse position, targeting the bony structures, specifically the transverse process connecting the rib. It is crucial to differentiate the pleura, which exhibits movement with each breath. The needle is then guided between the costotransverse ligament and the pleura, and during the injection, the observation of pleural displacement is essential to confirm precise positioning.
4.2. Evidence and Indications
Thoracic paravertebral blocks (PVBs) are as effective as thoracic epidurals for pain relief in chest wall trauma, rib fractures, post-thoracotomy cases, and situations where epidural anesthesia is not recommended [67,68][32][33]. The paravertebral block is a more straightforward procedure with fewer minor complications such as pneumothorax and, rarely, urinary retention, itching, nausea, and low blood pressure [69,70][34][35]. This makes it suitable for patients with varying degrees of hemodynamic instability. In patients with rib fractures, the paravertebral block is more effective for pain control than systemic opioid therapy [71][36]. After video-assisted thoracoscopic lobectomy for lung cancer, however, continuous paravertebral analgesia had significantly higher pain scores at rest and while coughing at 24 and 48 h than an epidural approach [72][37]. The PVB anesthetizes spinal nerves emerging from intervertebral foramina and produces unilateral, segmental, somatic, and sympathetic nerve block.
4.3. Why the ICU Physician Could Love It
The PVB and ESPB have overlapping possible applications, and the ESPB might provide the superior safety profile in most cases. However, especially in anatomical deviations like severe scoliosis, the PVB might be easier to perform.
5. Parasternal Block
Parasternal block techniques serve as valuable methods for administering regional analgesia to the central chest region. They are suitable to complement lateral chest wall blocks or as stand-alone blocks after median sternotomy. Parasternal blocks include the pecto-intercostal fascial block (PIFB) and the Transversus Thoracic Plane Block (TTPB) [73,74][38][39]. Both blocks address the same area of action. While the PIFB is more superficial and usually due to an incomplete fascial spread, it needs two injections per site. The TTPB is a deeper technique, where one injection per site is generally sufficient at the cost of a slightly higher potential for complications due to its proximity to the pleural line. Both blocks target the sensory dermatomes T2–T6 by blocking anterior branches of the intercostal nerves to provide analgesia of the area along the sternum.
5.1. How to Perform the Block
With the patient in the supine position, for the PIFB, the ultrasound probe is positioned in a craniocaudal direction at the level of the second intercostal space about 2 cm off the sternal edge (Figure 4). USG landmarks are the pectoralis major, the internal intercostal muscle, and the ribs. The target is the fascial plane between the pectoralis major and the external intercostal muscle. The procedure is repeated at the level of the fourth intercostal space. For the TTPB, the transducer is positioned in a transverse orientation at the level of the second intercostal space. The reason for that is the need to explicitly identify the internal mammary vessels located in the neurovascular plane between the intercostal and the transverse thoracic muscle, which is the target for the LA application. Volumes of LA are indicated in Table 1.
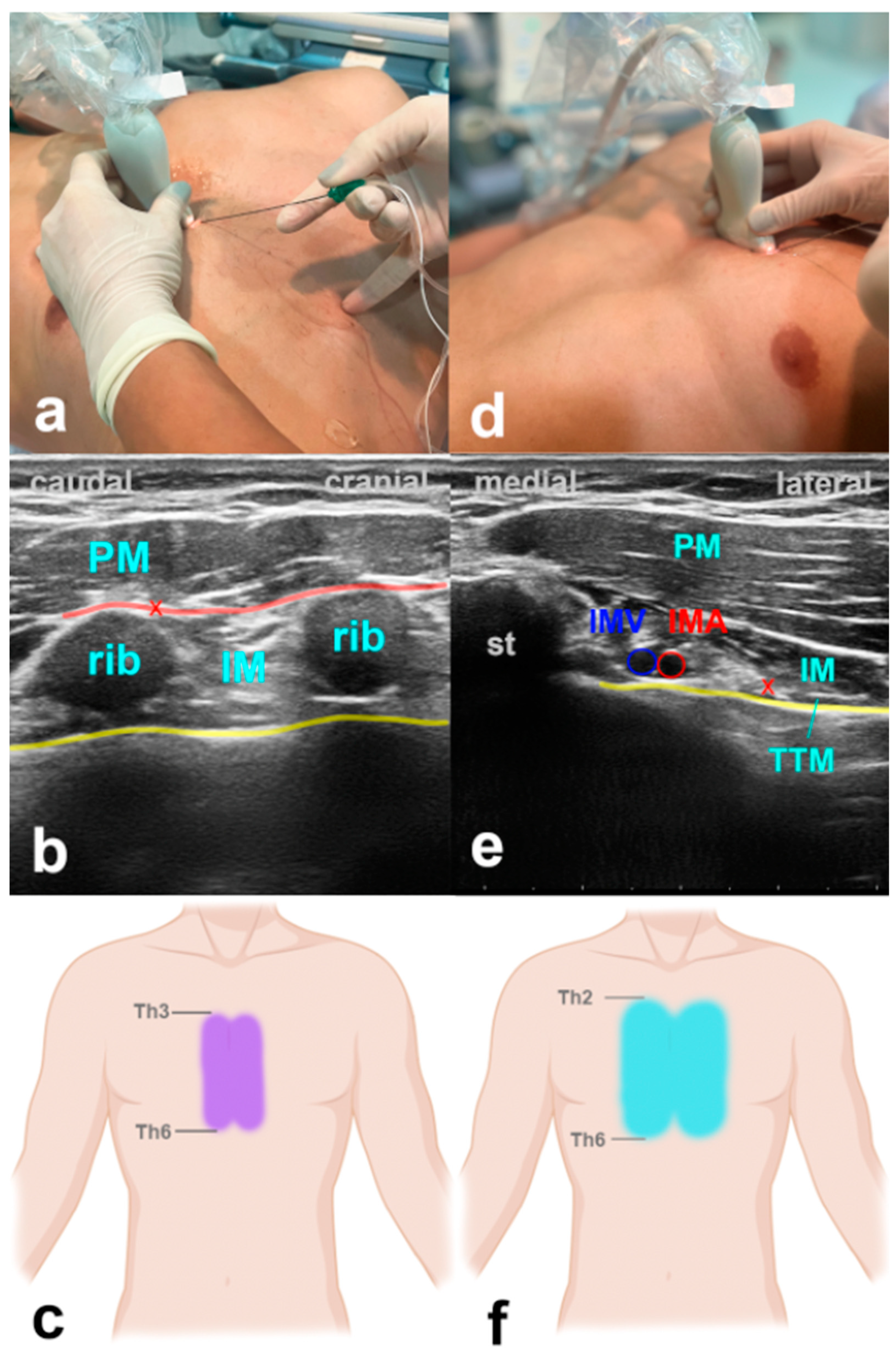
Figure 4. Parasternal blocks. (a) Transducer positioning for PIFB. (b) Ultrasound anatomy of PIFB: PM—pectoralis muscle; IM—intercostal muscle; yellow line—pleura; red cross—target point for the injection at the edge of the rib; red line—target space for PIFB. (c) Spread of PIFB. (d) Transducer positioning for TTPB. (e) Ultrasound anatomy of TTPB: PM—pectoralis muscle; IM—intercostal muscle; TTM—transverse thoracic muscle; st—sternum; IMV—internal mammary vein; IMA—internal mammary artery; yellow line—pleura; red cross—target point for the injection between IM and TTM. (f) Spread of TTPB.
5.2. Evidence and Indications
Several studies provide data on parasternal blocks decreasing intra- and postoperative opioid use, time to extubation, and improved postoperative performance at spirometry in cardiac surgery patients [73,75,76,77][38][40][41][42]. A recent meta-analysis showed a significant reduction in postoperative pain and opioid use in patients after median sternotomy [78][43].
5.3. Why the ICU Physician Could Love It
There is currently no alternative to these blocks other than intravenous analgesics. USG parasternal blocks offer an easy-to-perform, fast, and reliable possibility to control unexpected or insufficiently controlled post-sternotomy pain. Mainly, when performed after a CABG procedure with the harvesting of the mammary artery due to the altered anatomy, the PIFB might provide advantages in feasibility over the TTPB.
6. Intercostal Block
Intercostal blocks have been shown to offer reasonable pain control for invasive procedures such as chest tube insertion or in patients with rib fractures [79,80,81][44][45][46]. Compared to neuraxial methods or the ESPB, a significant disadvantage is the need for several punctures when targeting multiple levels, and some studies have yielded inferior performance regarding pain control compared to paravertebral or epidural block [70][35]. When performing intercostal block for pain control in rib fractures, it is recommended to perform the block at each level of costal fracture plus one level below and above to ensure complete coverage. Consequently, a minimum of three punctures would be needed in the case of one fractured rib, which might make the ESPB the favorable option.
References
- Kaur, U.; Shamshery, C.; Agarwal, A.; Prakash, N.; Valiveru, R.C.; Mishra, P. Evaluation of postoperative pain in patients undergoing modified radical mastectomy with pectoralis or serratus-intercostal fascial plane blocks. Korean J. Anesthesiol. 2020, 73, 425–433.
- Abu Elyazed, M.M.; Abdelghany, M.S.; Mostafa, S.F. The Analgesic Efficacy of Pecto-Intercostal Fascial Block Combined with Pectoral Nerve Block in Modified Radical Mastectomy: A Prospective Randomized Trial. Pain Physician 2020, 23, 485–493.
- Barrington, M.J.; Seah, G.J.; Gotmaker, R.; Lim, D.; Byrne, K. Quality of Recovery After Breast Surgery: A Multicenter Randomized Clinical Trial Comparing Pectoral Nerves Interfascial Plane (Pectoral Nerves II) Block With Surgical Infiltration. Anesth. Analg. 2020, 130, 1559–1567.
- Alfirevic, A.; Marciniak, D.; Duncan, A.E.; Kelava, M.; Yalcin, E.K.; Hamadnalla, H.; Pu, X.; Sessler, D.I.; Bauer, A.; Hargrave, J.; et al. Serratus anterior and pectoralis plane blocks for robotically assisted mitral valve repair: A randomised clinical trial. Br. J. Anaesth. 2023, 130, 786–794.
- Hoerner, E.; Stundner, O.; Naegele, F.; Fiala, A.; Bonaros, N.; Mair, P.; Holfeld, J.; Gasteiger, L. The impact of PECS II blockade in patients undergoing minimally invasive cardiac surgery-a prospective, randomized, controlled, and triple-blinded trial. Trials 2023, 24, 570.
- Durant, E.; Dixon, B.; Luftig, J.; Mantuani, D.; Herring, A. Ultrasound-guided serratus plane block for ED rib fracture pain control. Am. J. Emerg. Med. 2017, 35, 197.e193–197.e196.
- Park, M.H.; Kim, J.A.; Ahn, H.J.; Yang, M.K.; Son, H.J.; Seong, B.G. A randomised trial of serratus anterior plane block for analgesia after thoracoscopic surgery. Anaesthesia 2018, 73, 1260–1264.
- Blanco, R.; Parras, T.; McDonnell, J.G.; Prats-Galino, A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anaesthesia 2013, 68, 1107–1113.
- Piracha, M.M.; Thorp, S.L.; Puttanniah, V.; Gulati, A. “A Tale of Two Planes”: Deep Versus Superficial Serratus Plane Block for Postmastectomy Pain Syndrome. Reg. Anesth. Pain Med. 2017, 42, 259–262.
- Bhalla, P.I.; Solomon, S.; Zhang, R.; Witt, C.E.; Dagal, A.; Joffe, A.M. Comparison of serratus anterior plane block with epidural and paravertebral block in critically ill trauma patients with multiple rib fractures. Trauma. Surg. Acute Care Open 2021, 6, e000621.
- Diwan, S.; Nair, A. A retrospective study comparing analgesic efficacy of ultrasound-guided serratus anterior plane block versus intravenous fentanyl infusion in patients with multiple rib fractures. J. Anaesthesiol. Clin. Pharmacol. 2021, 37, 411–415.
- Liu, X.; Song, T.; Xu, H.Y.; Chen, X.; Yin, P.; Zhang, J. The serratus anterior plane block for analgesia after thoracic surgery: A meta-analysis of randomized controlled trails. Medicine 2020, 99, e20286.
- Khalil, A.E.; Abdallah, N.M.; Bashandy, G.M.; Kaddah, T.A. Ultrasound-Guided Serratus Anterior Plane Block Versus Thoracic Epidural Analgesia for Thoracotomy Pain. J. Cardiothorac. Vasc. Anesth. 2017, 31, 152–158.
- Elsabeeny, W.Y.; Ibrahim, M.A.; Shehab, N.N.; Mohamed, A.; Wadod, M.A. Serratus Anterior Plane Block and Erector Spinae Plane Block Versus Thoracic Epidural Analgesia for Perioperative Thoracotomy Pain Control: A Randomized Controlled Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2928–2936.
- Statzer, N.J.; Plackis, A.C.; Woolard, A.A.; Allen, B.F.S.; Siegrist, K.K.; Shi, Y.; Shotwell, M. Erector Spinae Plane Catheter Analgesia in Minimally Invasive Mitral Valve Surgery: A Retrospective Case-Control Study for Inclusion in an Enhanced Recovery Program. Semin. Cardiothorac. Vasc. Anesth. 2022, 26, 266–273.
- Nagaraja, P.S.; Ragavendran, S.; Singh, N.G.; Asai, O.; Bhavya, G.; Manjunath, N.; Rajesh, K. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann. Card. Anaesth. 2018, 21, 323–327.
- Ragavendran, S.; Raghu, C.; Prasad, S.R.; Arasu, T.; Nagaraja, P.S.; Singh, N.G.; Manjunath, N.; Muralikrishna, N.; Yogananth, N. Comparison of epidural analgesia with ultrasound-guided bilateral erector spinae plane block in aorto-femoral arterial bypass surgery. Ann. Card. Anaesth. 2022, 25, 26–33.
- Sørenstua, M.; Zantalis, N.; Raeder, J.; Vamnes, J.S.; Leonardsen, A.L. Spread of local anesthetics after erector spinae plane block: An MRI study in healthy volunteers. Reg. Anesth. Pain Med. 2023, 48, 74–79.
- Toscano, A.; Capuano, P.; Costamagna, A.; Canavosio, F.G.; Ferrero, D.; Alessandrini, E.M.; Giunta, M.; Rinaldi, M.; Brazzi, L. Is continuous Erector Spinae Plane Block (ESPB) better than continuous Serratus Anterior Plane Block (SAPB) for mitral valve surgery via mini-thoracotomy? Results from a prospective observational study. Ann. Card. Anaesth. 2022, 25, 286–292.
- Finnerty, D.T.; McMahon, A.; McNamara, J.R.; Hartigan, S.D.; Griffin, M.; Buggy, D.J. Comparing erector spinae plane block with serratus anterior plane block for minimally invasive thoracic surgery: A randomised clinical trial. Br. J. Anaesth. 2020, 125, 802–810.
- Nair, A.; Saxena, P.; Borkar, N.; Rangaiah, M.; Arora, N.; Mohanty, P.K. Erector spinae plane block for postoperative analgesia in cardiac surgeries—A systematic review and meta-analysis. Ann. Card. Anaesth. 2023, 26, 247–259.
- Morkos, M.; DeLeon, A.; Koeckert, M.; Gray, Z.; Liao, K.; Pan, W.; Tolpin, D.A. The Use of Unilateral Erector Spinae Plane Block in Minimally Invasive Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2023, 37, 432–436.
- Krishna, S.N.; Chauhan, S.; Bhoi, D.; Kaushal, B.; Hasija, S.; Sangdup, T.; Bisoi, A.K. Bilateral Erector Spinae Plane Block for Acute Post-Surgical Pain in Adult Cardiac Surgical Patients: A Randomized Controlled Trial. J. Cardiothorac. Vasc. Anesth. 2019, 33, 368–375.
- D’Hondt, N.; Rex, S.; Verbrugghe, P.; Van den Eynde, R.; Hoogma, D. Erector spinae plane block for enhanced recovery after cardiac surgery in minimally invasive mitral valve surgery. J. Cardiothorac. Vasc. Anesth. 2020, 34, S22–S24.
- Wiech, M.; Żurek, S.; Kurowicki, A.; Horeczy, B.; Czuczwar, M.; Piwowarczyk, P.; Widenka, K.; Borys, M. Erector Spinae Plane Block Decreases Chronic Postoperative Pain Severity in Patients Undergoing Coronary Artery Bypass Grafting. J. Clin. Med. 2022, 11, 5949.
- Syal, R.; Mohammed, S.; Kumar, R.; Jain, N.; Bhatia, P. Continuous erector spinae plane block for analgesia and better pulmonary functions in patients with multiple rib fractures: A prospective descriptive study. Braz. J. Anesthesiol. (Engl. Ed.) 2021, 74, 744289.
- Hamilton, D.L.; Manickam, B. Erector spinae plane block for pain relief in rib fractures. Br. J. Anaesth. 2017, 118, 474–475.
- Elshazly, M.; El-Halafawy, Y.M.; Mohamed, D.Z.; Wahab, K.A.E.; Mohamed, T.M.K. Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: A randomized comparative trial. Korean J. Anesthesiol. 2022, 75, 502–509.
- Wan, F.T.; Chin, S.E.; Gwee, R.; Chong, Y.; Au-Yong, A.; Matthews, A.; Zaw, M.W.; Lie, S.A.; Loh, L.; Koh, D.; et al. Pre-operative erector spinae plane block should be considered a viable option for laparoscopic colectomies. Surg. Endosc. 2023, 37, 7128–7135.
- Kelava, M.; Anthony, D.; Elsharkawy, H. Continuous Erector Spinae Block for Postoperative Analgesia After Thoracotomy in a Lung Transplant Recipient. J. Cardiothorac. Vasc. Anesth. 2018, 32, e9–e11.
- Schnabel, A.; Reichl, S.U.; Kranke, P.; Pogatzki-Zahn, E.M.; Zahn, P.K. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br. J. Anaesth. 2010, 105, 842–852.
- Mohta, M.; Verma, P.; Saxena, A.K.; Sethi, A.K.; Tyagi, A.; Girotra, G. Prospective, randomized comparison of continuous thoracic epidural and thoracic paravertebral infusion in patients with unilateral multiple fractured ribs--a pilot study. J. Trauma. 2009, 66, 1096–1101.
- Casati, A.; Alessandrini, P.; Nuzzi, M.; Tosi, M.; Iotti, E.; Ampollini, L.; Bobbio, A.; Rossini, E.; Fanelli, G. A prospective, randomized, blinded comparison between continuous thoracic paravertebral and epidural infusion of 0.2% ropivacaine after lung resection surgery. Eur. J. Anaesthesiol. 2006, 23, 999–1004.
- Karmakar, M.K.; Greengrass, R.A.; Latmore, M.; Levin, M. Thoracic & Lumbar Paravertebral Block. In Hadzic’s Textbook of Regional Anesthesia and Acute Pain Management, 2nd ed.; Hadzic, A., Ed.; McGraw-Hill Education: New York, NY, USA, 2017.
- Joshi, G.P.; Bonnet, F.; Shah, R.; Wilkinson, R.C.; Camu, F.; Fischer, B.; Neugebauer, E.A.; Rawal, N.; Schug, S.A.; Simanski, C.; et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth. Analg. 2008, 107, 1026–1040.
- Malekpour, M.; Hashmi, A.; Dove, J.; Torres, D.; Wild, J. Analgesic Choice in Management of Rib Fractures: Paravertebral Block or Epidural Analgesia? Anesth. Analg. 2017, 124, 1906–1911.
- Lai, J.; Situ, D.; Xie, M.; Yu, P.; Wang, J.; Long, H.; Lai, R. Continuous Paravertebral Analgesia versus Continuous Epidural Analgesia after Video-Assisted Thoracoscopic Lobectomy for Lung Cancer: A Randomized Controlled Trial. Ann. Thorac. Cardiovasc. Surg. 2021, 27, 297–303.
- Zhang, Y.; Gong, H.; Zhan, B.; Chen, S. Effects of bilateral Pecto-intercostal Fascial Block for perioperative pain management in patients undergoing open cardiac surgery: A prospective randomized study. BMC Anesthesiol. 2021, 21, 175.
- Desire, S.M.; Hayward, G. Transversus Thoracic Muscle Plane Block (TTMPB). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Schiavoni, L.; Nenna, A.; Cardetta, F.; Pascarella, G.; Costa, F.; Chello, M.; Agrò, F.E.; Mattei, A. Parasternal Intercostal Nerve Blocks in Patients Undergoing Cardiac Surgery: Evidence Update and Technical Considerations. J. Cardiothorac. Vasc. Anesth. 2022, 36, 4173–4182.
- Pascarella, G.; Costa, F.; Nonnis, G.; Strumia, A.; Sarubbi, D.; Schiavoni, L.; Di Pumpo, A.; Mortini, L.; Grande, S.; Attanasio, A.; et al. Ultrasound Guided Parasternal Block for Perioperative Analgesia in Cardiac Surgery: A Prospective Study. J. Clin. Med. 2023, 12, 2060.
- Chen, H.; Song, W.; Wang, W.; Peng, Y.; Zhai, C.; Yao, L.; Xia, Z. Ultrasound-guided parasternal intercostal nerve block for postoperative analgesia in mediastinal mass resection by median sternotomy: A randomized, double-blind, placebo-controlled trial. BMC Anesthesiol. 2021, 21, 98.
- King, M.; Stambulic, T.; Hassan, S.M.A.; Norman, P.A.; Derry, K.; Payne, D.M.; El Diasty, M. Median sternotomy pain after cardiac surgery: To block, or not? A systematic review and meta-analysis. J. Card. Surg. 2022, 37, 3729–3742.
- Luketich, J.D.; Land, S.R.; Sullivan, E.A.; Alvelo-Rivera, M.; Ward, J.; Buenaventura, P.O.; Landreneau, R.J.; Hart, L.A.; Fernando, H.C. Thoracic epidural versus intercostal nerve catheter plus patient-controlled analgesia: A randomized study. Ann. Thorac. Surg. 2005, 79, 1845–1849.
- De Pinto, M.; Edwards, W. Management of Pain in the Critically Ill Patient in Irwin-Rippe’s Intensive Care Medicine, 6th ed.; Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 2016.
- Britt, T.; Sturm, R.; Ricardi, R.; Labond, V. Comparative evaluation of continuous intercostal nerve block or epidural analgesia on the rate of respiratory complications, intensive care unit, and hospital stay following traumatic rib fractures: A retrospective review. Local Reg. Anesth. 2015, 8, 79–84.
More
