Infective endocarditis represents an infection involving specific cardiac tissues: the endocardium, native heart valves at any position, prosthetic heart valves, or any implanted cardiac devices. I
nfective endocarditis (IE
) can be clinically insidious since epidemiology and natural history are in constant evolution, reflecting the complex interaction between an aging population, multiresistant microorganisms, evolving patterns of healthcare, available therapies, and the application of aggressive surgery. IE remains a relatively uncommon condition, with an annual occurrence of approximately 3–10 cases per 100,000 individuals
[1]. The characteristics of this ailment exhibit variations across the globe, particularly when comparing countries with differing income levels. In regions with limited economic resources, rheumatic heart disease continues to be the prominent risk factor. Patients in these areas are typically younger, and the primary source of infection stems from penicillin-sensitive streptococci, commonly acquired within the community. Conversely, the prevalence of rheumatic heart disease has decreased in affluent nations due to enhanced living conditions and the widespread availability of antibiotics. In higher-income countries, the principal risk factors for IE encompass degenerative valve issues, diabetes, cancer, intravenous drug usage, and congenital heart abnormalities. Furthermore, this demographic skews older, with the average age transitioning from the mid-40s in the early 1980s to surpassing 70 years between 2001 and 2006
[2]. This changing epidemiology mirrors the wide medical advances both in terms of the rise in cardiovascular device implantation procedures (prosthetic valves, pacemaker leads, transcatheter valves, and vascular devices) and in terms of the better use of multiple imaging modalities and multidisciplinary care, which also translates into escalations in diagnosis. A diagnosis of infective endocarditis needs the integration of clinical findings, microbiological analyses, and imaging results. Due to its heterogeneity, the management of patients with IE necessitates a multidisciplinary approach with physicians, cardiologists, cardiac surgeons, electrophysiologists, microbiologists, histopathologists, infectious disease specialists, radiologists, and echocardiographers. Despite advancements in both detection and treatment, results continue to exhibit unsatisfactory trends, which is evidenced by in-patient mortality rates of 18%, along with a 6-month mortality rate of 30%. The impact on outcomes is significantly influenced by factors such as S. aureus infection, age progression, the persistence of positive blood cultures despite receiving suitable antibiotic treatment, and the existence of notable concurrent health conditions
[1]. It is imperative to achieve a precise diagnosis promptly and administer antimicrobial treatment to mitigate the potential for complications and enhance the overall prognosis. Surgical intervention is carried out in approximately 40–50% of infective endocarditis cases
[3] in order to avoid progressive heart failure, irreversible structural damage in case of uncontrolled infection, and the prevention of embolism.
2. Native Valve Endocarditis: Repair versus Replacement
Native valve infective endocarditis is not frequently encountered, with an estimated occurrence of about 2 to 10 instances per 100,000 person-years
[4][7]. Damage to the valvular endothelium or endocardium exposes subendothelial collagen and matrix molecules, prompting platelet and fibrin accumulation and forming a microthrombotic lesion. Subsequently, bacteria present in the bloodstream colonize this lesion, initiating replication and leading to the development of an infected vegetation, a defining characteristic of infective endocarditis. Certain cardiac conditions can predispose individuals to the onset of infective endocarditis, such as congenital anomalies (like ventricular septal defects and bicuspid aortic valves) or acquired valvular issues (including degenerative valvular diseases, aortic stenosis, and rheumatic heart disease). In more developed nations, the principal predisposing cardiac conditions encompass degenerative valvular disorders, congenital valvular irregularities, and the presence of intracardiac devices
[5][8]. On the other hand, factors not directly related to the heart, such as poor dental health, intravenous drug usage, hemodialysis, chronic liver disease, diabetes, compromised immune function, neoplastic diseases, and the presence of indwelling intravascular devices, can also contribute to an individual’s susceptibility to this condition. The general principle of IE surgery is to obtain a radical debridement of vegetation and infected tissue and to avoid and limit, when possible, the use of foreign material. When it comes to infective endocarditis involving native heart valves, the mitral valve (MV) tends to be affected most frequently, accounting for approximately 40–50% of cases
[6][9]. Throughout history, mitral valve repair (MVr) has demonstrated better survival rates and overall outcomes, especially in comparison to valve replacement (MVR), effectively restoring life expectancy across all age brackets. Furthermore, a strong association has been observed between surgical volume and patient outcomes, both at hospital and surgeon levels. This suggests that the frequency of interventions performed by a surgeon is an independent predictor of successful repair, surgical outcomes, and enhanced survival
[7][10]. However, within the context of endocarditis, the advantages and predictors of mitral valve repair are less well established. Within this particularly challenging and intricate patient population, real-world statistics from multicenter reports indicate that rates of successful repair range only from 19% to 32%
[8][11].
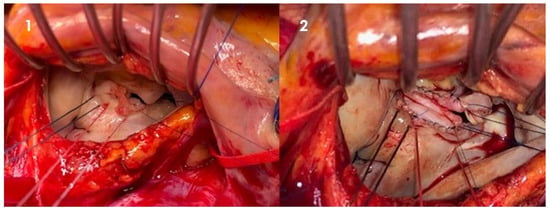
In general, techniques may vary between leaflet segmental resection for valve destruction, primary closure, or patch repair (
Figure 1) for leaflet perforation and neochordae implantation to replace ruptured chordae and support reconstructed leaflets.
Figure 1. Intraoperative picture of native mitral valve infective endocarditis. Through left atriotomy, exposure of mitral valve. (1) Large vegetation involving anterior and posterior leaflet of mitral valve suspended and resected; (2) leaflet reconstruction with a pericardial patch (Cardiovascular Department, UO of Cardiac Surgery of IRCCS Humanitas Research Hospital).
Independently of specific techniques, multiple retrospective trials have proven the effectiveness of MVr in favoring short- and long-term outcomes. Nana Toyoda et al.
[9][13] retrospectively analyzed 1970 patients undergoing isolated MVr (19%) or MVR (81%) for active infective endocarditis between 1998 and 2010. The primary outcome was long-term survival, and the secondary outcomes were recurrent endocarditis and reoperation in the follow-up period. Over the study period, MVr rates increased from 10.7% to 19.4%. Patients undergoing mitral repair tended to be younger, more often in stable hemodynamic conditions, and less likely to have staphylococcal infections. At 12 years, survival was 68.8% after MVr versus 53.5% in the MVR group. MVr was associated with a lower rate of recurrent endocarditis at 12 years (4.7% vs. 9.5%) and a similar rate of reoperation (9.1% vs. 8.6%). Feringa et al.
[10][14] conducted an analysis of 24 studies, revealing that the rates of both early and late mortality after mitral valve repair (MVr) stood at only 2% and 8%, respectively. Following MVr for infective endocarditis (IE), freedom from reoperation exceeded 90% at the 5-year mark and remained above 85% at the 10-year milestone. These findings underscore the sustained durability of MVr over the long term, with consistent results reported across various studies.
The aortic valve is affected in 35–39% of cases
[6][9]. According to data from the EUROENDO Registry
[11][18], surgical procedures were performed during hospitalization for 1596 patients, constituting 51.2% of the entire cohort. Among these cases, aortic valve procedures were carried out in 54.5% of instances, with a mere 2.3% undergoing aortic valve repair. In recent years, aortic valve repair has progressively emerged as a novel alternative to aortic valve replacement for addressing stable aortic regurgitation (AR). Aortic valve reconstruction has demonstrated not only the ability to circumvent the drawbacks of anticoagulation in younger populations but has also shown a reduced incidence of valve-related complications when compared to previously reported rates associated with aortic valve replacement. Unlike in mitral valve diseases, the potential for aortic valve repair is limited and technically demanding. Additionally, within the context of endocarditis, aortic valve repair is even less established. One of the main reports on this topic is from Mayer et al.
[12][19]. Their study retrospectively analyzed a cohort of 100 patients diagnosed with active native aortic valve infective endocarditis (IE). Among them, 33 patients underwent aortic valve repair (AVr), while 67 patients opted for aortic valve replacement (AVR). In terms of the absence of Grade II or higher recurrent aortic regurgitation, freedom from thromboembolic events at 5 years, and recurrence of endocarditis, no significant disparities were observed between the two groups. However, the survival rate at 4 years was notably superior following repair. The actuarial freedom from reoperation after 5 years stood at 65% in the AVr group, as opposed to 90% in the AVR group. The researchers also established a correlation between the size of patches used and the risk of late failure. AVr has demonstrated its worth as a viable substitute for aortic valve replacement (AVR) in case of aortic insufficiency, even with bicuspid aortic valves
[13][14][20,21].
Compared to left-sided infective endocarditis (IE), the incidence of right-sided IE tends to be lower, possibly due to the relatively infrequent prevalence of typical pathological conditions affecting the right-sided valves. This variation may stem from differences in the properties of the right-sided endothelium and disparities in right-side hemodynamic patterns, characterized by lower pressure gradients and jet velocities across the right-sided valves, as well as reduced right-sided wall stress and lower oxygen content in venous blood
[15][26]. Over the past two decades, there has been a steady increase in the occurrence of tricuspid valve (TV) IE. This rise is attributable to the growing prevalence of factors such as intravenous drug use, the implantation of right-sided cardiac devices, central venous catheterization, and repaired congenital defects
[16][27]. Similar to what has been emphasized regarding mitral valve IE, the guiding principles for surgical intervention in TV IE continue to favor repair over replacement. This approach helps mitigate the risks of prosthetic valve deterioration and lowers the likelihood of recurrence.
The outcomes of tricuspid valve repair (TVr) and tricuspid valve replacement (TVR) are indeed comparable in terms of long-term survival. Yanagawa B. et al.
[17][28] conducted an analysis of 12 unmatched retrospective observational studies encompassing 1165 patients. Their goal was to compare the early and late outcomes of tricuspid valve repair versus replacement. The primary indications for surgery included septic pulmonary embolism, left-sided infective endocarditis (IE), right-sided heart failure, and persistent bacteremia. Across the studies, the median proportion of repairs was 59%, while replacements constituted 41%. Common repair strategies included vegetectomy, the De Vega procedure, annuloplasty ring insertion, bicuspidization, and leaflet patch augmentation. Among valve replacements, bioprosthetic valves accounted for 83%, while mechanical prostheses comprised 17%. The analysis revealed no significant differences between TVr and TVR in terms of perioperative mortality and long-term all-cause mortality. However, TVr was linked to lower rates of recurrent IE and a reduced need for reoperation, although a trend toward a greater risk of moderate to severe tricuspid regurgitation was noted. Additionally, TVr was associated with a decreased requirement for a permanent pacemaker.
In cases of right-sided IE, an alternative to surgery involves the utilization of percutaneous, vacuum-assisted devices designed for removing intracardiac masses. Such devices serve as a means to remove large tricuspid valve vegetations when the risks associated with surgery are prohibitive. In 2014, the US Food and Drug Administration approved the AngioVac system (AngioDynamics, Latham, NY, USA), a device designed for removing undesired intravascular materials, such as thrombi and emboli
[18][35]. George et al.
[19][36] retrospectively analyzed 33 patients with tricuspid valve IE in which a percutaneous aspiration device was employed to manage large vegetations. Reductions in vegetation size were observed in 61% of cases, and 91% of patients were discharged home.
3. Prosthetic Valve and Implantable Device Endocarditis
The epidemiology of infective endocarditis is changing and the incidence of prosthetic valve (PV) IE is increasing, as proven by the comparison of the different registries provided through the years. According to the latest, PV IE accounts for 30% of cases in the EURO-ENDO Registry, 25% in the 2008 French registry, and 21% in the International Collaboration on Endocarditis Prospective Cohort Study reported in 2009
[5][11][20][21][8,18,39,40]. Prosthetic valve endocarditis represents a significant complication of valve replacement, occurring at a rate of 0.3% to 1.2% per patient-year. This corresponds to approximately 3% to 6% of individuals who receive a prosthetic valve experiencing this complication within the first 5 years following implantation
[22][41]. Patients undergoing surgery for prosthetic valve infective endocarditis (PV IE) present a diverse range of clinical scenarios, often being older and more prone to nosocomial infections. In comparison to cases of native valve endocarditis, PV IE continues to be a severe condition associated with notably higher in-hospital mortality rates, ranging from 19% to 50%, as opposed to the 7% to 13% rates observed in patients with native valve IE. If not addressed promptly, PV IE can lead to severe anatomical consequences such as valvular apparatus destruction, abscess formation, pseudoaneurysms, fistulas, perforations, heart block, and strokes.
Both mechanical and bioprosthetic valves are susceptible to infection, exhibiting no significant difference in prevalence within the first 5 years (5.7%). Interestingly, mechanical valves present a heightened risk of infection during the initial 3 months following operation
[23][45], whereas bioprosthetic valves demonstrate an elevated risk at the 18-month mark post valve replacement
[24][46]. The population of pathogens that contribute to infective endocarditis (IE) in prosthetic valves varies depending on whether the period being considered is within 1 year from the operation or beyond. This one-year timeframe is conventionally used as a cutoff to differentiate early and late prosthetic valve IE
[25][47]. Instances of early prosthetic valve IE (occurring within the first year) are most prevalent in the initial two months following valve replacement. This is attributed to microorganisms that either invade the prosthesis during the surgical intervention or disseminate hematogenously in the early days or months post-surgery. Notably, a similar microbiologic profile has been observed between cases of prosthetic valve IE within 2 months of valve replacement and those occurring between 2 and 12 months after the surgery
[26][48].
Additionally, a noteworthy and emergent concern in the context of prosthetic valve IE involves infections associated with transcatheter-implanted valves and percutaneous edge-to-edge mitral valve repair. Incidences of IE following transcatheter aortic valve implantation (TAVI) appear to be relatively low, with certain studies reporting around 1% incidence
[27][50], albeit being slightly higher among male patients. However, in studies with longer follow-up periods and larger patient cohorts, the occurrence of infective endocarditis is more notable, with a cumulative incidence of TAVI prosthesis infection reaching up to 5% during the initial 5 years
[28][51]. The majority of TAVI endocarditis cases (90%) are managed conservatively, resulting in high in-hospital mortality and suboptimal short-term survival
[29][52]. Surgical approaches involving TAVI prosthesis explantation have not demonstrated superior survival rates, although such reports are scarce. This specific context still presents limited experience with treatment strategies, and a significant number of patients are often considered inoperable or at high surgical risk in elective settings. As indications for TAVI expand to encompass intermediate- to low-risk patients, a comprehensive understanding of TAVI endocarditis treatment, comparative evaluations of medical versus surgical options, and well-defined surgical treatment pathways are essential. Conversely, the risk of IE in patients undergoing percutaneous edge-to-edge mitral valve repair using the MitraClip (Abbott, Abbott Park, IL, USA) appears to be quite low. A comprehensive registry of MitraClip patients did not document a single instance of IE throughout a 5-year follow-up period
[30][53].
4. Surgery in Complex Infective Endocarditis: Current Trends
Endocarditis is a potentially destructive disease and the treatment can widely range in complexity from medical antimicrobial treatment to complex cardiac reconstruction. Endocarditic lesions may manifest as small vegetations originating from the cusps or leaflets, or fenestrations, which can often be easily treated with excision and valve replacement or valve repair, as already mentioned. If the disease progresses locally, it may lead to valvular annulus involvement and the development of an annular abscess. In turn, a deeper myocardial involvement may lead to damage to the fibrous skeleton of the heart and to the conduction system, as well as perforation into other cardiac chambers. The scope and nature of surgical intervention are directly contingent upon the extent of tissue damage, consistently adhering to the principle of thorough debridement, and may necessitate annular reconstruction. The choice of material for the new annulus is generally a matter of surgeon preference, with options including bovine pericardium, both fixed and fresh autologous pericardium, as well as Dacron, all being documented choices. Pericardial tissue holds the advantage of increased pliability and the capacity to conform to the underlying myocardium, thereby reducing the likelihood of flow beneath the patch that could potentially lead to the development of a pseudoaneurysm or shunt. Additionally, the utilization of autologous or heterologous pericardium has not demonstrated an elevated risk of reinfection. Following the placement of the patch, the decision between valve repair and replacement is determined by the extent of valve leaflet or cusp destruction. Approximately 15% of cases of mitral valve infective endocarditis (MVE) may involve a mitral annular abscess
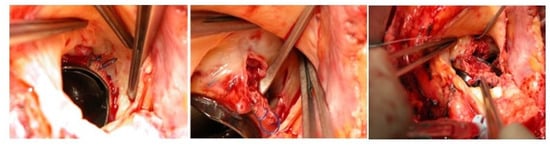
[31][54]. These abscesses are typically located in the posterior mitral annulus, encompassing the posterior leaflet, the annulus itself, and the underlying myocardium. When an annular abscess is present or substantial destruction of the posterior annulus is evident, this implies the necessity of debridement and subsequent reconstruction of the atrioventricular groove using a patch, prior to proceeding with mitral valve surgery. The patch aims to reconstruct atrioventricular continuity and should always be oversized in order to comfortably cover the defect circumferentially. Attention must be paid to the underlying left circumflex coronary artery. Oversizing the patch guarantees good sealing, thanks to the intracavitary ventricular pressure against the myocardium, and contributes to hemostasis. Aortic annular erosion and abscess can be detected in both native and prosthetic aortic valve endocarditis (
Figure 23).
Figure 23. Intraoperative picture of mechanical prosthetic aortic valve endocarditis and aortic annular erosion and abscess, detected during the prosthesis removal (Cardiovascular Department, UO of Cardiac Surgery of IRCCS Humanitas Research Hospital).
Managing such lesions can be intricate due to extensive tissue damage, limited available area for prosthesis implantation, and, in more severe cases, potential left ventricular aortic discontinuity. Surgical intervention involves the thorough removal of the infected region and rectification of the annular defect. Multiple techniques have been outlined to address this condition. Typically, closure of the abscess cavity involves the implementation of a patch to rebuild the left ventricle outflow tract, followed by valve or root replacement. In instances where profound circumferential destruction of the aortic annulus is observed, some experts propose an alternative approach involving the reconstruction of the left ventricle outflow tract and the translocation of the aortic valve into the ascending aorta. This technique aims to position the new valve prosthesis away from the infected area
[32][55].
The aortic mitral curtain (AMC) is a complex component of the heart’s fibrous skeleton, situated between the lateral and medial trigones of the mitral valve. It forms connections between the left and non-coronary cusps of the aortic valve and links the anterior leaflet of the mitral valve to the aortic valve cusps and the roof of the left atrium, effectively separating the mitral valve from the aortic root. Given its invasive nature, managing this structure typically necessitates a complex surgical procedure. Initially proposed by Tirone David, the surgical approach involves double valve replacement using pericardial or Dacron patches to reestablish “neoaortomitral continuity”
[33][56]. This procedure has been termed the “Commando procedure” by the Cleveland Clinic group and referred to as the “UFO procedure” by the Leipzig group
[34][57]. For cases in which the infection has not affected the posterior mitral leaflet and at least the free edge of the anterior mitral leaflet remains viable, a modified version of the Commando procedure, known as the “Hemi-Commando procedure”, has been suggested
[35][58]. The Commando procedure, being an invasive surgical option, offers several advantages in cases of infective endocarditis (IE). It ensures the complete removal of infected material and reduces the risk of prosthesis dehiscence, paravalvular leaks, and patient–prosthesis mismatch, all of which could lead to the need for re-intervention
[36][59]. However, comparing the outcomes of the Commando procedure to less aggressive strategies, both in terms of mortality rates and the risk of re-intervention, is challenging due to the rarity of the disease, the generally poor health of patients requiring this procedure, and the extensive involvement and damage to cardiac structures. It is widely recognized that this aggressive approach should be considered whenever feasible, particularly under the care of experienced surgeons.
5. Conclusions
The literature and guidelines on the surgical management of infective endocarditis are based mainly on observational studies, given the difficulty in designing randomized trials in such a complex setting often present in urgent contexts. Due to the varying anatomical and clinical scenarios, heart teams are often brought to difficult decisions on the most appropriate strategy to adopt; moreover, the best choices are made through a shared decision-making process that should include the patient too. Decision making should take into account the localization and extent of the infection, patient preoperative status and comorbidities, and the choice of the best timing for surgery. Special relevance should be given to timing, which influences the risk of neurological complications and the extent of the infection, which, in turn, have a strong impact on post-operative outcomes and mortality rates. Whenever possible, surgeons should prefer a repair strategy over replacement in order to avoid the insertion of prosthetic material into infected tissue, limit the extent of the infection process, and better preserve ventricular function. Another important key step is the choice of the prosthesis or conduit. To date, guidelines do not support the selection of one substitute over another, and the selection of the most appropriate valve replacement strategy or conduit should consider the longevity of the substitutes, especially when biological, the potential recurrence of infection, and the risk of redo surgery. Surgeons should be able to maneuver and master all the reconstructive techniques described in the literature in order to manage all possible anatomical and pathological settings, particularly in consideration of the recent and future rise in cardiovascular device implantation and the consequent need for removal in case of endocarditis.