STwo maprophytic mites calledin species of Demodex are commonly found on the skin of adult humans. They are primarily presentmites have been described in humans: Demodex folliculorum and Demodex brevis. These mites have been implicated in the folliculosebaceous units of facial skin and are a part of the normal skin microbiota. Whenpathogenesis of certain human cutaneous disorders, including rosacea. It has been proposed that their present in low numbers, they do not cause any harm. Hce in the skin merely represents an ‘innocent bystander’ phenomenon; however, their increased density has been linked to certain skin disorders. For instance,others have advocated that Demodex infestation is frequently observed in rosacea, raising concerns about its role as a contributing factor in this condiplays a role in the pathogenesis of the disease or its exacerbation.
- Demodex Mite
- Rosacea
- Multinucleate Histiocyte
- Demodicosis
- Skin Pathogen
1. Introduction
Demodex mite is recognized as a commensal organism in many animals and humans, making it interesting in human and veterinary medicine. Two main species of Demodex mites have been described in humans: Demodex folliculorum and Demodex brevis. These mites have been implicated in the pathogenesis of certain human cutaneous disorders, including rosacea. It has been proposed that their presence in the skin merely represents an ‘innocent bystander’ epiphenomenon; however, others have advocated that Demodex plays a role in the pathogenesis of diseases or their exacerbation.
2. Demodex mites in humans
Demodex mites (famiCly Demodicidae, claass Arachnida, oOrder Acarina) are commensal inhabitants of human skin. They are saprophytic mites and are obligatory human ectoparasites. They were first reported by Jakup Henle, a professor of anatomy from Zurich, in 1841, and since then, about 65 species have been described.[1] They are ubiquitously found on the normal skin of adult humans, with a density of < 5 mites/cm2. In humans, two species have been described: Demodex folliculorum, which resides primarily in hair follicles (mainly infundibulum), and Demodex brevis, which mainly inhabits the sebaceous glands or the meibomian glands.[21]
They comprise the normal skin microbiota and, at low densities, are innocuous. However, there is no known benefit. They are usually localized in the folliculosebaceous units of cheeks, forehead, nose, nasolabial folds, and eyelids.[32][43] They feed on cellular proteins and sebum by utilizing salivary enzymes. The enzymatic reaction may induce degradation of the follicle, causing perifollicular inflammation. Overgrowth of mites may also result in mechanical blockage of follicular openings. These mites hae mites have been implicated in the pathogenesis of certain cutaneous disorders, including rosacea (especially granulomatous and papulopustular types), ‘rosacea-like’ demodicosis, perioral dermatitis, blepharitis, acne vulgaris, seborrheic dermatitis, Demodex folliculitis of the scalp, and hund Human immunodeficiency virus-associated eosinophilic folliculitis. A study found significantly higher rates of Demodex infestation in patients with rosacea, acne vulgaris, and seborrheic dermatitis.[5] The highest incidence was observed in rosacea patients.
3. Demodex Mmite and Rrosacea
RoAsacea is a common chronic inflammatory skin condition that usually onsets in the fourth decade of life and affects 1% to 10% of the world's population. The major types include erythematotelangiectatic (vascular), papulopustular (inflammatory), phymatous, ocular, and one granulomatous variant. Increased infestation by Demodex mite in rosacea and the term demodicosis was first described by Ayres in 1961.[1] As mites can be they can be present in significant numbers in about 50% of cases of rosacea, their role as an underlying contributing factor in this disorder has been debated and discussed for many years.[43] A systemic review found a high prevalence and degree of Demodex mite in erythematotelangiectatic and papulopustular rosacea.[6] They found mite infestation significantly more likely in rosacea than in healthy controls and patients with other facial dermatoses (e.g., discoid lupus erythematosus).
Rosacea is considered a disease of the immune system associated with neurogenic triggers. Its links with Demodex mites remain unclear. However, increasing evidence suggests it may play a pivotal role in this condition. Reactivation of the immune system, localized inflammation, and follicular changes caused by the mites are suggested to contribute to the development of the disease. It has been phas been proposed that facial skin affected by rosacea provides an appropriate environment or fertile ground for the multiplication of these mites, and their presence merely illustrates an ‘innocent bystander’ epiphenomenon and not a causal eventn. Others have advocated that Demodex plays a part as a root cause of rosacea, and some expressions of this condition may depict a response to the overabundance of these mites. Demodex has the necessary elements to stimulate the host’s immune system. These mites may produce local immunosuppression, permitting them to survive and play an essential role as a skin pathogen.[74] This idea is also upheld by the fact that rosacea signs and symptoms, especially papulopustules, may improve once Demodex is adequately treated with acaricidal agents (e.g., topical permethrin and ivermectin). Some have supported the argument that Demodex may not contribute to the root cause of rosacea; however, their overabundance is a cofactor in causing folliculitis and abscess formation, further aggravating and exacerbating pre-existing disease.
4. MHicroscopic Cstopathologic changes in the Skin Dskin due to Demodex
Standardized skin surface biopsy technique with cyanoacrylate glue is a semi-invasive method used to measure the density of Demodex mite.[5] Other sampling or examination methods include the tape method, pressuring method to express follicular contents, conventional skin biopsy, confocal microscopy, and polymerase chain reaction-based method.[6] The mere presence of mites does not indicate pathogenicity, and their increased density, extrafollicular location, and inflammatory response are better indicators. Demodex infestation, defined as a density of ≥ 5 mites/cm2, is closely related to pathogenic activity.
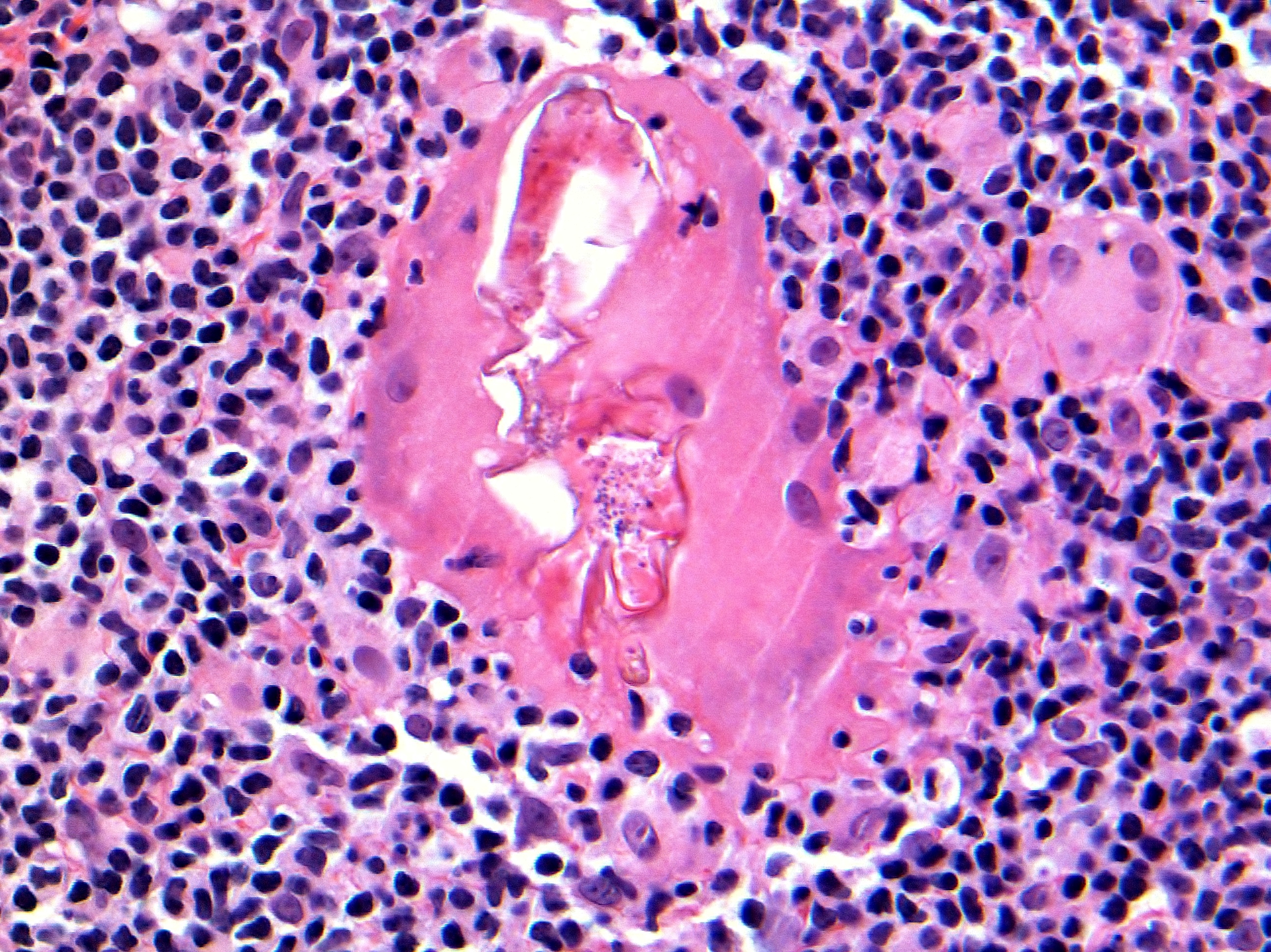
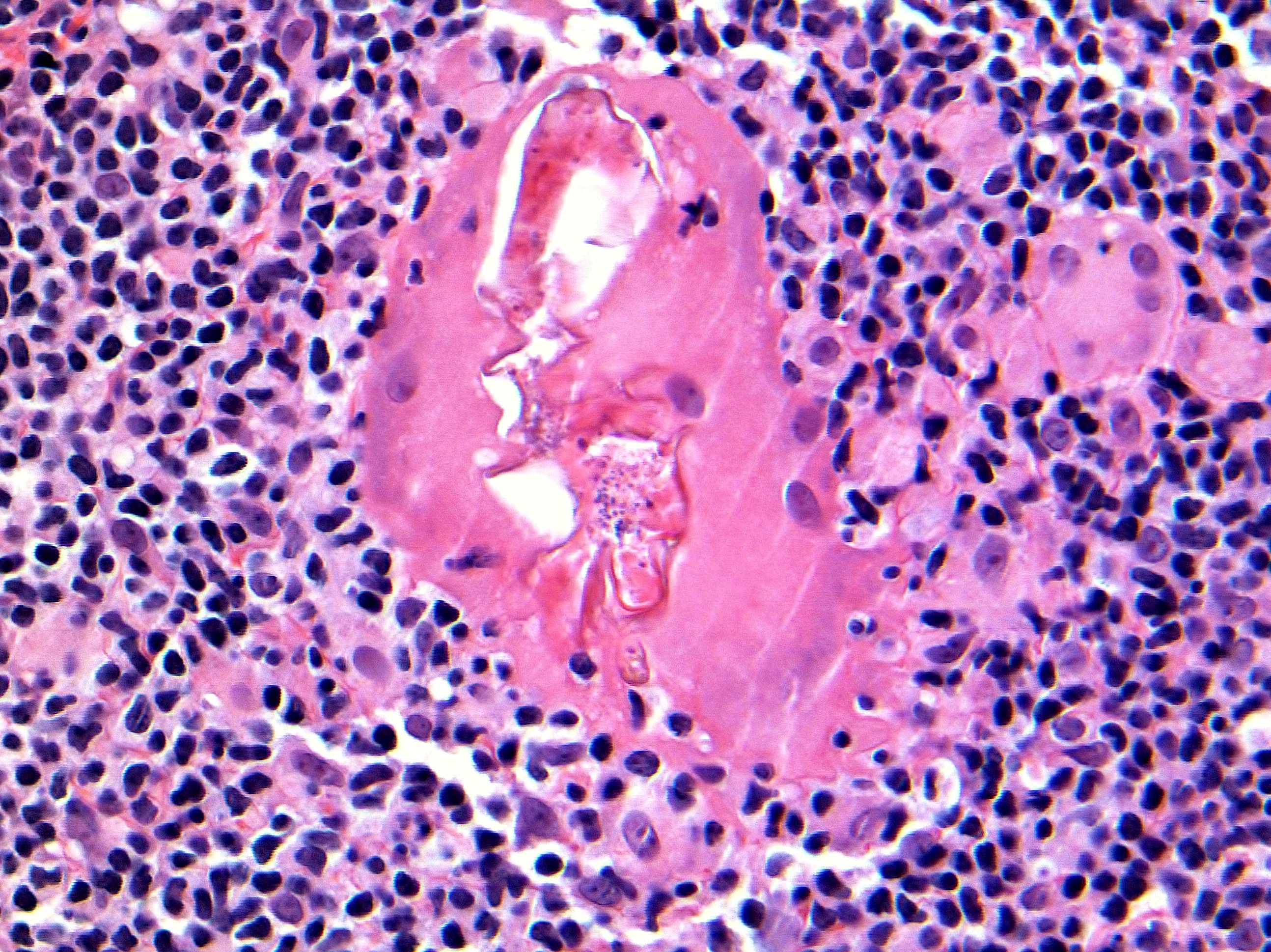
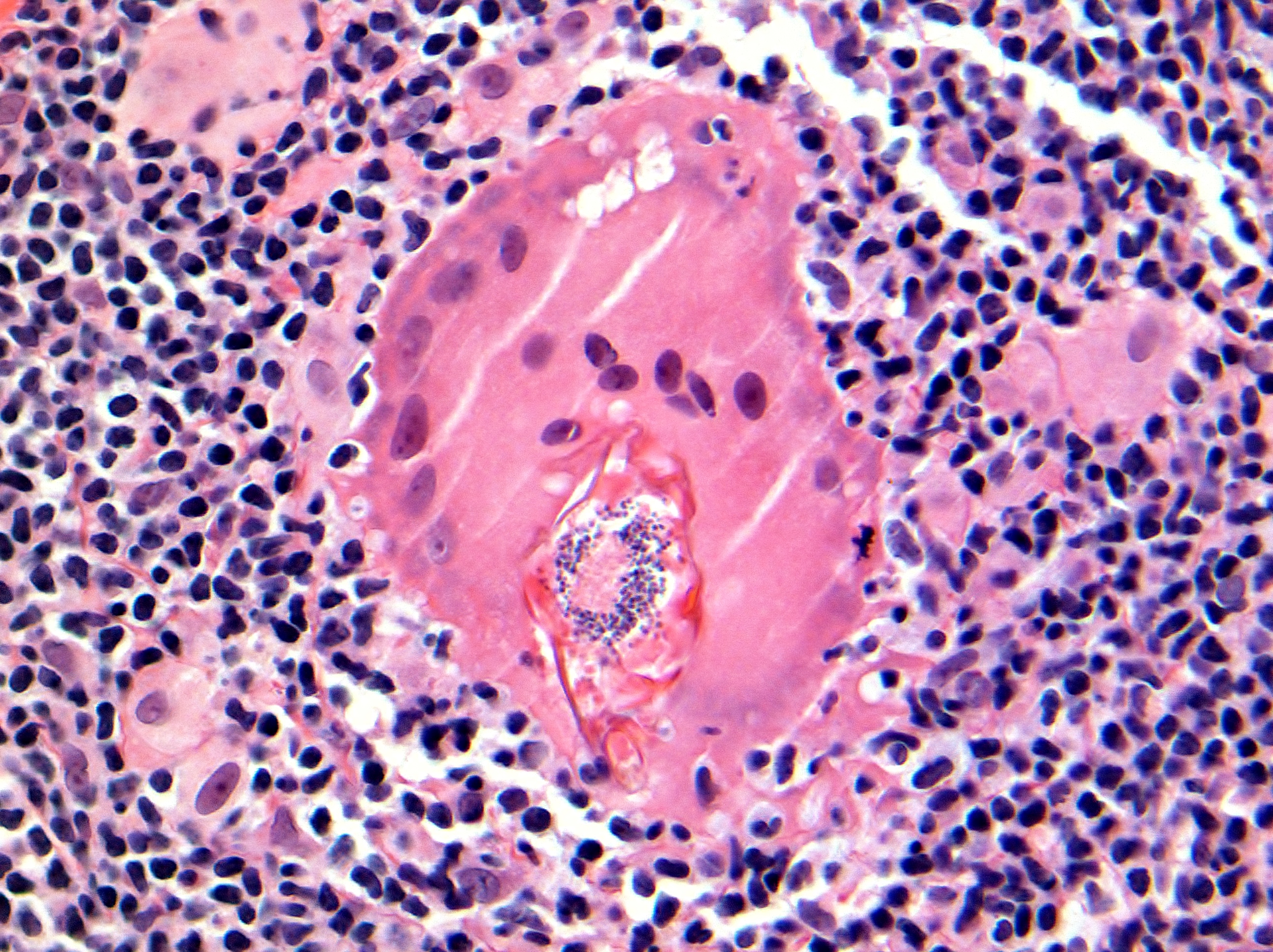
A conventional skin biopsy, such as a punch biopsy, can be more helpful in assessing the inflammatory changes. From a histopathologic point of view, it is common to see Demodex mites in facial biopsies from patients suffering from rosacea. Most often, they are observed residing within folliculosebaceous units; however, occasionally, folliculitis with extrafollicular mites surrounded by dermal granulomatous or suppurative inflammation is noted.[8] Gicant cell granulomas with multinucleated histiocytes attempting to phagocytize the mite are noted (Figures 1 and 2)also be noted.[5] The perifollicular infiltrate correlates with the number of Demodex mites residing in the hair follicle. An abnormal number of mites or their position in an abnormal location (such as the dermis) has been endorsed as a measure to be considered a causative agent in thea case of rosacea.[96] In up
Botoh 66% of cases of granulomatous rosacea, Demodex mites have been found. A marked decrease in the inflammatory infiltrate after acaricidal therapy has been demonstrated, which suggests that the mites had caused the inflammation.[10]
Figure 1. Multinucleated giant histiocyte containing Demodex mite (Hematoxylin and Eosin, original magnification x400).
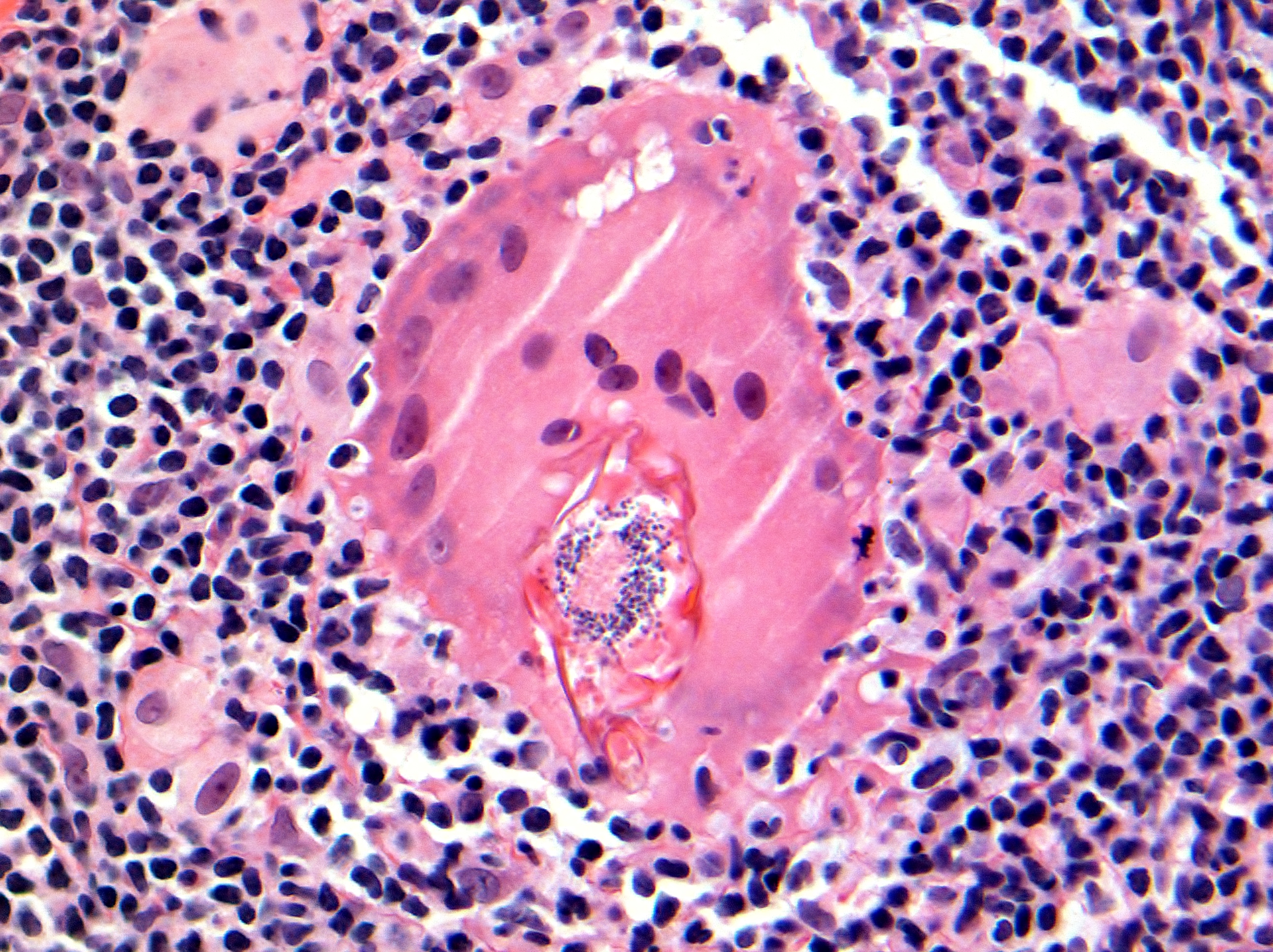
Figure 2. Multinucleated giant histiocyte containing Demodex mite (Hematoxylin and Eosin, original magnification x400).
Figuresfigures above (Hematoxylin and Eosin, original magnification 1 andx400) 2 show a parasitized multinucleated giant histiocyte in perifollicular reticular dermis ccontaining a Demodex mite. The biopsy is from a nasal skin lesion in a patient with rosacea. Following damage to the hair follicle, the mite has entered the dermis, causing a granulomatous reaction around it.
5. Summary:
In sum, Demodex proliferation in human skin could be a consequence rather than the cause, a pathogen causing the disease, or an aggravating factor that exacerbates the disease. The debate regarding the pathogenic role of Demodex in rosacea will continue. However, when an organism can enter the dermis and cause a significant inflammatory reaction around itself, the hypothesis that it is just an ‘innocent bystander’ appears unlikely. At least in some cases of rosacea, this mite does appear to act as an aggravating or triggering factor to complicate pre-existing disease.
References
- Rusiecka-Ziolkowska, J.; Nokiel, M.; Fleischer, M. Demodex: an old pathogen or a new one? . Aylesworth R, Vance JC. Demodex folliculorum and Demodex brevis in cutaneous biopsies.. J Am Acadv C Dermatolin Exp Med. . 1982014, 23, 295-298., 7(5), 583-589.
- Aylesworth, R.; Vance J.C. Demodex folliculorum and Demodex brevis in cutaneous biopsies. Erbagei Z, Ozgoztasi O. The significance of Demodex folliculorum density in rosacea.. Int J Am Acad Dermatol. 19982, , 37, 583-589.(6), 421-425.
- Erbagei, Z.; Ozgoztasi, O. The significance of Demodex folliculorum density in rosacea. IRoihu T, Kariniemi AL. Demodex mites in acne rosacea.. J Cutant J DermatPathol. 1998, 37, 421-425., 25(10), 550-552.
- Roihu, T.; Kariniemi, A.L. Demodex mites in acne rosacea. Akilov OE, Mumcuoglu KY. Immune response in demodicosis.. J CEutan Pathr Acad Dermatol Venereol. 1998, 25, 550-552.. 2004, 18(4), 440-444.
- Aktaş Karabay, E.; Aksu Çerman, A. Demodex folliculorum infestations in common facial dermatoses: acne vulgaris, rosacea, seborrheic dermatitis. Ecker RI, Winkelmann RK. Demodex granuloma.. An Brasch Dermatol. 2020, 9. 1979, 115, 187-193.(3), 343-344.
- Chang, Y.S.; Huang, Y.C. Role of Demodex mite infestation in rosacea: A systematic review and meta-analysis. Karincaoglu Y, Bayram N, Aycan O, Esrefoglu M. The clinical importance of demodex folliculorum presenting with nonspecific facial signs and symptoms.. J Am Acad Dermatol. 20017, 77, 441-447.4, 31, 618-626.
- Akilov, O.E.; Mumcuoglu, K.Y. Immune response in demodicosis. J Eur Acad Dermatol Venereol . 2004, 18, 440-444.
- Ecker, R.I.; Winkelmann, R.K. Demodex granuloma. Arch Dermatol. 1979, 115, 343-344.
- Karincaoglu, Y.; Bayram, N.; Aycan, O.; Esrefoglu, M. The clinical importance of demodex folliculorum presenting with nonspecific facial signs and symptoms. J Dermatol. 2004, 31, 618-626.
- Schaller, M; Pietschke, K. Successful therapy of ocular rosacea with topical ivermectin. Br J Dermatol . 2018, 179, 520-521.