A holistic view should be taken towards patient’s treatment, care and counselling in order to provide patient-centric, ethically and legally informed care for pregnant cancer patients. It is essential to consider individual circumstances of each pregnant cancer patient where each patient is seen as a person embedded in the realities of their lives and the changes that a cancer diagnosis brings to themselves and their pregnancy care.
- cancer during pregnancy
- ethics
- guidelines
- patient centricity
- patient engagement
- checklist
- ethical models
- ethics checklist
1. Introduction
| Type of Malignancy | Modes of Treatment | Considerations for Pregnant Patients | Considerations for the Foetus |
|---|---|---|---|
| Breast cancer [19][20][19,20] | Surgery (safe throughout pregnancy), radiotherapy (contraindicated in pregnancy), chemotherapy (second and third trimester), hormonal/endocrine therapy (contraindicated), immunotherapy (contraindicated, PD-1/PD-L1 pathway could result in immune response against the foetus), targeted therapy (contraindicated with exception of trastuzumab, which may be used in the first trimester under close monitoring). | Physiological breast changes should be considered, delaying reconstruction surgery after delivery. Higher risk of pregnancy complication cannot be excluded. |
Increased risks of stillbirths, small gestational weight, preterm delivery, neonatal mortality. No significant impairment after exposure to chemotherapy. Prematurity correlated with worse cognitive outcome irrespective of cancer treatment. |
| Thyroid cancer [21][22][21,22] | Surgery (second trimester or after delivery), endocrine therapy (LT4 therapy should start immediately after surgery), radioactive iodine (contraindicated in pregnancy and breastfeeding), immunotherapy with tyrosine kinase inhibitors (TKIs) is not well studied. | Calcium and vitamin D supplementation, hypothyroidism should be avoided by correct supplementation of thyroxine. No evidence to support pregnancy termination. |
Thyroid hormone deficiency can cause severe neurological disorders. |
| Cervical cancer [7][23][7[24],23,24] | Hysterectomy (in advanced cases, can be combined with a caesarean delivery or performed post-partum, otherwise not compatible with pregnancy), cold knife conization (risk of premature birth), radical trachelectomy/cervicectomy (risk of premature birth), chemotherapy (second and third trimester), radiotherapy (contraindicated). | Caesarean section is preferred delivery method, especially in advanced cases. Fertility preservation in advanced cases might not be possible. Chemotherapy is not recommended beyond 35 weeks of gestation to allow maternal and foetal bone marrow recovery before delivery. |
Chemotherapy can affect foetal eyes, genitals, hematopoietic system, nervous system, foetal growth. Single cases of bilateral hearing loss and rhabdomyosarcoma have been reported. |
| Other gynaecological cancers (vulvar, vaginal, endometrial, ovarian cancer, ovarian masses with low malignant potential) [7] | Laparoscopic surgery (feasible throughout pregnancy, not longer than 90–120 min), surgery (decided upon individual cases), chemotherapy (second and third trimester), radiotherapy (contraindicated), systemic therapies not well studied. | Caesarean section is a preferred delivery method, especially in advanced cases. In cases of advanced epithelial ovarian cancer, pregnancy termination should be considered in the first half of pregnancy. Chemotherapy is not recommended beyond 35 weeks of gestation to allow maternal and foetal bone marrow recovery before delivery. |
If possible, delivery should not be induced before 37 weeks to allow foetal maturity. Breastfeeding should be avoided with ongoing chemotherapeutic, endocrine and targeted treatment. |
| Lymphomas (Hodgkin lymphoma and non-Hodgkin lymphoma) [25][26][25,26] | Chemotherapy (second and third trimester), radiotherapy (conflicting data), immunotherapy (limited data) | Deferring therapy until after delivery does not always affect maternal outcomes and can be considered. Pregnancy termination can be considered in the first trimester. Patients receiving antenatal therapy have more obstetric complications (preterm contractions and preterm rupture of membranes). |
No gross foetal malformations or anomalies have been reported. Low gestational age and admissions to NICU did not differ between neonates exposed and not exposed to chemotherapy. Those exposed to chemotherapy had lower birth weight. |
| Melanoma [27][28][27,28] | Excisions (throughout pregnancy—safe and necessary), targeted therapies (BRAF inhibitors) and checkpoint inhibitors (anti-PD1 and anti-CTLA4) may be teratogenic. | Relationship between pregnancy and melanoma should not be ruled out. Some reports suggest poorer prognosis for pregnant patients, but evidence is inconclusive. | No evidence that melanoma diagnosis will have adverse effected on the foetus. Melanoma accounts for 30% of metastatic spread to the placenta. This does not mean that the foetus will be affected. |
| Brain tumours [29][30][29,30] | Surgery, chemotherapy, radiotherapy—only limited data available due to rarity of the condition. | Delivery recommended after 34 weeks of gestation to allow foetal maturity. Caesarean delivery recommended. |
No known foetal complications. Steroids for foetal lung maturation might be needed if early delivery is needed due to deteriorating maternal condition. |
| Lung cancer [31][32][31,32] | Chemotherapy (second and third trimester), targeted therapies—only limited data available due to rarity of the condition | Increased risk of lung infections. Case reports suggest that lung cancer is diagnosed at advanced stages in pregnancy and prognosis is poor. | No adverse outcomes data reported. Due to advanced stage of maternal cancer, there might be a metastatic spread to the placenta. This does not mean that the foetus will be affected. |
2. Ethical Models Applicable to Cancer Care during Pregnancy
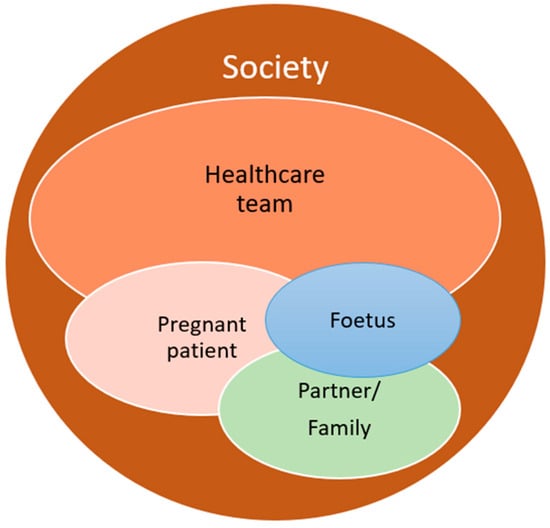
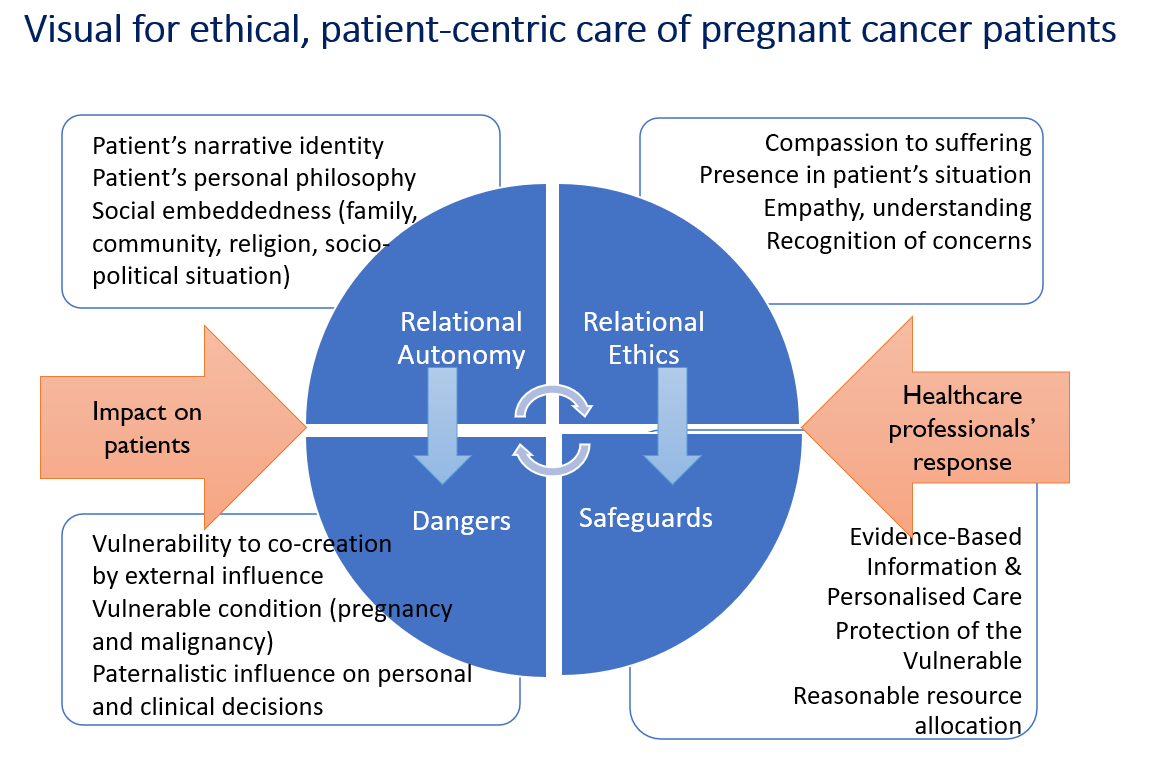
There are many ethical guidance models that can be applied to cancer care during pregnancy. However, none of them appear to adequately address all ethical issues arising in these circumstances. Four biomedical ethics principles developed by Beauchamp and Childress [42] and the European principles in bioethics and biolaw [43][44][43,44] were used as a starting point (Table 2). Since caring for pregnant cancer patients also requires consideration of the patient’s relationships—including the patient’s perceived relationship with the foetus, partner, other children (if present), parents, relatives, friends and wider community, as well as ethno-socio-cultural and political environment [34]—elements of ethics of care [45][46][45,46], relational ethics [47][48][47,48] and medical maternalism [49][50][49,50] were also considered. These relational, patient-focused approaches were used as adjuncts to specify the principles-based guidance and to illustrate how the proposed theoretical framework (Figure 12) and subsequent ethics checklist (Table 3) can work in already existing healthcare structures by supplementing rather than challenging already established patient care processes and services.| Ethical Models Used to Develop the Guidance | Model Description and Specification | Key References | |
|---|---|---|---|
| Principle-based approaches | Four principles for biomedical ethics (Georgetown principles) by Beauchamp and Childress | Respect to patient’s autonomy, including relational aspectsRespect to patient’s autonomy, including relational aspects Nonmaleficence: avoiding harm before doing good Nonmaleficence: avoiding harm before doing good Beneficence: maximising the benefit for the pregnant patient and developing foetus Justice: considering a big picture and a broader contextBeneficence: maximising the benefit for the pregnant patient and developing foetus Justice: considering a big picture and a broader context |
[42] |
| European principles of bioethics and biolaw presented by Rendtorff | Autonomy: individual freedom to make choices Dignity: moral responsibility to human life Integrity: right to bodily integrity, right to refuse treatment Vulnerability (respect to vulnerability): recognising human vulnerabilities, protecting vulnerable groups |
[43][44][43,44] | |
| Relational, patient-focused approaches | Relational ethics | Trusted relationship building with the patient Patient-centric approach to patient care Interdependency and freedom Emotions and reason |
2.2. Relational, Patient-Focused Approaches
Shared decision making and care of pregnant cancer patients can be a very intense, emotional and psychologically demanding task for the healthcare team. It might challenge clinical teams’ attitudes towards the patient, their circumstances and even relationship with the patient. Indeed, the pregnant cancer patient’s relationship with the clinical team is of pivotal importance, requiring recognition of the patient’s unique situation; understanding of their individual circumstances; and empathy with their clinical, moral and practical concerns. Relational ethics can support clinicians with a patient-centred approach to patients by guiding the relationships toward empathy, attempting to understand patients’ emotions and reasoning [47]. The ethics of care further specify that compassion, presence, empathy and recognition of a patient as a fellow human being play a significant role in building trusted relationships between healthcare professionals and their patients [64], which is regarded with high importance in midwifery [46]. Medical maternalism is one more patient-focused approach emerging in contemporary bioethics [50]. It considers patients’ autonomy in a relational context and encourages patient support by the clinical team, where patients are provided correct, up-to-date and easy to understand information in order to guide them through the decision-making process with their best interests in mind. Caring for pregnant cancer patients can have further relational and care obligation complexities. Some healthcare professionals might feel an obligation to protect the developing foetus and might consider it a separate patient [65][66][65,66]. Such protection, however, can only be achieved if pregnant patients perceive foetal interests the same way as the clinical team does and are willing to collaborate with the clinicians. Some jurisdictions might have legal frameworks governing pregnancy care and restricting pregnancy termination. A recent example from the United States in the Dobbs vs. Jackson case shows that cancer treatment options might be restricted for pregnant patients [38][67][38,67], despite the historic trend denying foetuses a legal entity status until they are born [68]. Relational, patient-focused approaches to patient care can fall short of being universally applicable as they mostly describe the practice of providing care [69]. Such approaches are based on forming trusted relationships with the patient, but they do not offer a clear set of rules to follow which could be applied in different patient care scenarios. Furthermore, some suggest that care ethics and relational approaches to patient care are solely based on Western perceptions of patient care and lack cultural representativeness and inclusiveness [70].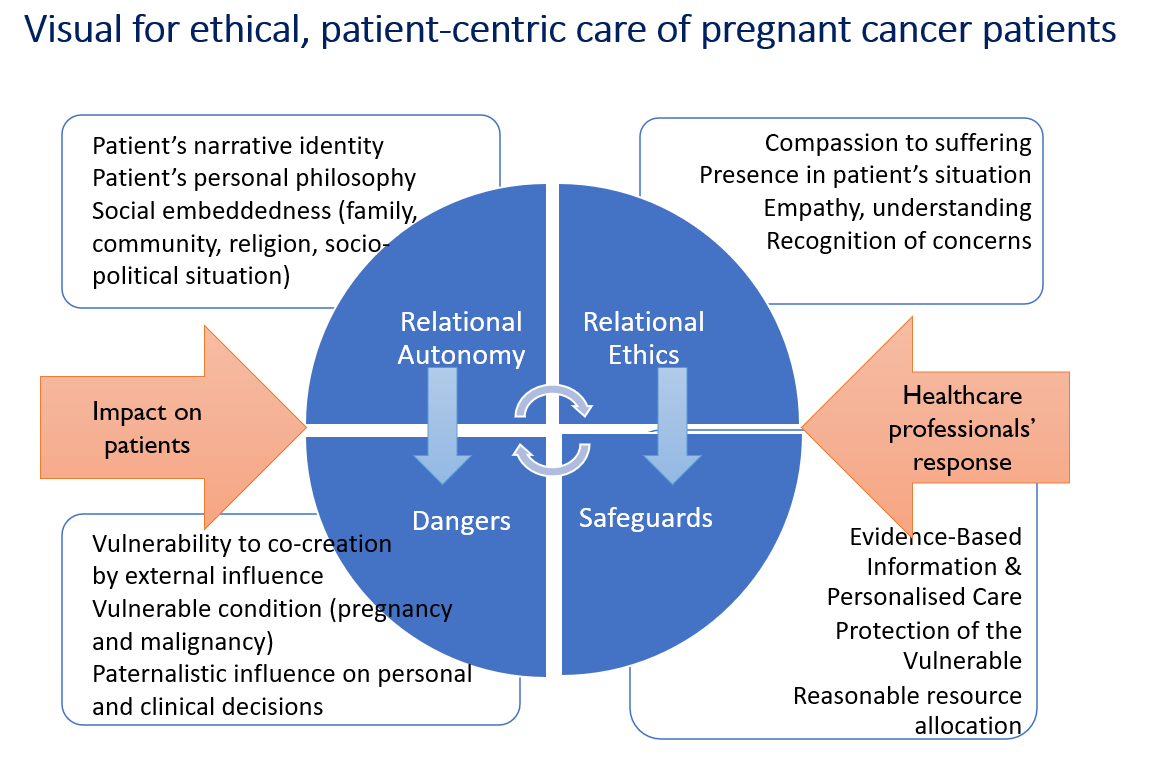
|
Ethics Checklist to Support Decision-Making Process in Treatment and Care of Pregnant Cancer Patients
|
Tick |
||
|
Perform an accurate clinical assessment to be able to discuss the disease prognosis, treatment intent (curative vs. palliative) and its impact on pregnancy.
|
|
||
|
Identify the patient’s social and relational circumstances (e.g., spouse/partner/significant other; children; other relevant relationships; literacy and information comprehension level; occupation/employment situation; housing arrangements; socio-economic status; religion/spiritual/philosophical beliefs and needs; family/relational dynamics; gender identification; social roles important to the patient; etc.)
|
|
||
|
Recognise the potential vulnerability of the pregnant cancer patient, take time to listen to patient’s concerns and fears, allow time to ask questions. Be informed about support services available for these patients.
|
|
||
|
Recognise the developing foetus as a vulnerable entity and in need of protection by its parents as much as healthcare professionals. Take into consideration the gestational age of the foetus and the local legal requirements around pregnancy termination for medical reasons.
|
|
||
|
Confirm and document patients’ decision-making capacity:
|
|
||
|
If the patient is capable of consenting to medical treatment and interventions: |
If the patient is not capable of consenting to medical treatment and interventions (unconscious, lacks capacity to make decisions): |
|
|
|
Discuss with the patient their preferences regarding the medical decision-making process and communication with clinical team. |
Identify the surrogate decision maker, ask about their own wellbeing and support needs, share information about available support. |
|
|
|
Discuss with the patient their preferences, expectations and perceptions about their desired cancer treatment and pregnancy outcome in their individual situation and care priorities, existing and desired advance care directives. |
Discuss the perceived patient and their caregiver(s)’ preferences with the surrogate decision maker, establish the expectations and perceptions about the desirable disease treatment and pregnancy outcome and care priorities, known/existing advance care directives, including the views and wishes the patient is known to have had expressed in the past. |
|
|
|
Support the patient with drafting, completing or updating the advance care directives, clearly document the patient’s intent for which circumstances they are applicable. |
Identify other stakeholders, who might need to be involved in the medical decision-making process (e.g., partner, parents, etc.) in order to establish the best interest of the patient and developing foetus. |
|
|
|
Identify other stakeholders involved in the clinical decision-making process (e.g., partner, parents, etc.) whose involvement is important to the patient.
|
If the patient is conscious, involve them in the conversation about their treatment and care options, where possible and practical. |
|
|
|
Document all relevant information in the patient’s notes/electronic medical records.
|
Document all relevant information in the patient’s notes/electronic medical records. |
|
|
|
Upon confirming the decision-making capacity, share evidence-based information regarding treatment options and related clinical outcomes, expected short- and long-term toxicities for the patient and the developing foetus.
|
|
||
|
Inform the patient/surrogate decision maker about ongoing cancer during pregnancy research and available options for participation in clinical trials.
|
|
||
|
Involve a multidisciplinary team that includes different medical specialties with expertise in care of pregnant patients with cancer and other healthcare professionals, such as nurses, psychologists, social workers, hospital ethics committee/ethics advisory board, ethical and spiritual care providers, etc.
|
|
||
|
Obtain a written consent to treatment and/or care plan (if required by local regulations), allowing adequate time for decision making, following the discussion on available cancer and pregnancy management options.
|
|
||
|
Where written consent to treatment/care plan is not a routine or mandatory requirement, allow adequate time for decision making, following the discussion on available cancer and pregnancy management options and document it in the patient’s notes/electronic medical records.
|
|
||
|
Clearly document patient’s/surrogate decision maker’s decisions, concerns and explanation given on treatment and care in patient’s notes/electronic medical records.
|
|
||
|
Periodically review changes in patient’s treatment and care plan, updating consent documentation as per local legal requirements and professional guidance.
|
|
||
|
Seek consultation with other hospital/care facility teams (hospital ethics committee/ethics advisory board, social services, patient financial support, patient counselling, etc.) if available healthcare resources are not adequate for handling a particular patient’s case, if patient’s or surrogate decision maker’s treatment/care preferences are futile and might result in significant financial burden to the healthcare system or themselves.
|
|
||
|
Ensure that the patient/surrogate decision maker are aware of an option to request a second opinion from another doctor/multidisciplinary team without retaliation from the treating doctor/team or administration.
|
|
||
|
Should patient/surrogate decision makers refuse treatment or suggested care pathway, seek to understand the reasons behind it, be ready to answer questions and give time to consider the options without retaliation from the treating doctor/team or administration.
|
|
||
|
Identify existing and potential concerns within the clinical team based on legal considerations, political leaning, religious beliefs and personal preferences; seek reconciliation of such concerns in a structured manner (e.g., moral case deliberation, clinical ethics consultation, ethical counselling, etc.)
|
|
||
|
Acknowledge the rights and their legal/professional limits for clinical and supporting team members to exercise conscientious objections (e.g., administering treatment to a pregnant patient that can potentially harm the foetus, carrying out abortion/pregnancy termination procedures, proving post-abortion care to cancer patients, etc.), constructively engage concerned team members, seek council with the legal team, ethics consultation service, senior management, etc., to ensure that patient safety, continuity of treatment and care are not compromised due to moral objections leading to staff shortage.
|
|
||
| [ | 47 | ] | [48][47,48] |
| Care ethics (ethics of care) | Compassion to patient’s suffering Presence in patient’s unique situation, active listening Empathy to patient’s feelings and circumstances Recognition of a patient as fellow human being |
[45][46][45,46] | |
| Medical maternalism | Shared decision making Accessible evidence-based information Conversation and understanding of patient’s circumstances and best interest Patient guidance through clinical advice and reason |
[49][50][49,50] | |
