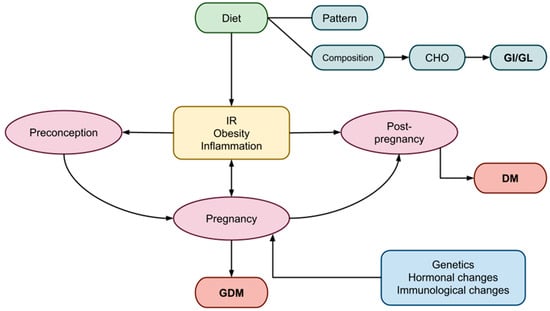
Gestational diabetes mellitus (GDM) is a common metabolic disorder that often develops during pregnancy, characterized by glucose intolerance and insulin resistance (IR). To ensure the well-being of both the mother and the fetus, the body undergoes multiple metabolic and immunological changes that result in peripheral IR and, under certain hereditary or acquired abnormalities, GDM in predisposed women. The adverse short- and long-term effects of GDM impact both the mother and the fetus. Nutrition seems to play an important role to prevent GDM or improve its evolution. An emphasis has been given to the proportion of carbohydrates (CHO) relative to protein and lipids, as well as dietary patterns, in GDM. The effects of CHO on postprandial glucose concentrations are reflected in the glycemic index (GI) and glycemic load (GL). Diets rich in GI and GL may induce or exacerbate IR, whereas diets low in GI and GL appear to enhance insulin sensitivity and improve glycemic control. These positive outcomes may be attributed to direct interactions with insulin and glucose homeostasis or indirect effects through improved body composition and weight management.
- gestational diabetes mellitus
- diet
- nutrition
- carbohydrates
- insulin resistance
- glycemic load
- glycemic index
- obesity
- pregnancy
1. Introduction
32. Pregnancy
3.1. Gestational IR
2.1. Gestational IR
Insulin resistance is commonly observed during pregnancy, although the processes underlying its pathogenesis are complex and not yet fully understood [46][20]. In a typical pregnancy, maternal tissues gradually become more insensitive to insulin, resulting in a 50–60% decrease in insulin sensitivity as gestation progresses [47,48][21][22]. During the second half of pregnancy, when IR is at its peak, GDM is believed to develop when β-cells fail to adapt to the increasing demand for insulin [47][21]. Both women with and without GDM experience similar increases in insulin production during pregnancy; however, women with GDM start at a lower level. Consequently, the β-cell abnormality in GDM is considered more of a chronic condition than a development during pregnancy. Overt T2DM may develop postpartum as a result of this β-cell malfunction in GDM [49][23]. Prior to and independently of changes in insulin sensitivity, the insulin secretory response significantly increases in the early stages of pregnancy. This metabolic adaptation may be mediated by circulating hormones, with placental hormones and/or cytokines likely responsible for these changes in maternal physiology [50][24]. Mostly women with preexisting IR and predisposing risk factors develop GDM. These risk factors include PCOS, low- or high-birth-weight fetuses, a family history of T2DM or GDM, multiparity, advanced maternal age, and a prior GDM diagnosis [51][25]. However, women with no preexisting IR may also develop GDM because they have defective β-cell function due to genetic or idiopathic reasons. IR in early pregnancy and a positive glucose challenge test in later pregnancy, irrespective of BMI, were also found to be associated with visceral adipose tissue depth evaluated by ultrasound that exceeded the top quartile in early pregnancy [52][26].32.1.1. Gestational Weight Status
Maternal weight is a crucial factor that significantly influences pregnancy progression, in conjunction with maternal age. Extensive studies have examined weight, calculating BMI in early pregnancy and the percentage of weight gained during pregnancy. Being overweight and obese are established contributors to GDM. A high antenatal BMI and excessive weight gain during pregnancy are recognized risk factors for various complications, including postpartum weight retention, GDM in subsequent pregnancies, future obesity, T2DM, and long-term CVD [53,54][27][28]. Additionally, these factors contribute to obstetrical complications such as pre-eclampsia, eclampsia, macrosomia, hemorrhage, and cesarean delivery [55][29]. Regarding maternal body fat levels, a significant correlation with maternal leptin levels during pregnancy has been observed. Leptin, a hormone produced by adipose tissue, has various metabolic effects, including decreased insulin sensitivity in non-pregnant individuals [58][30]. Mothers with elevated body fat levels are also more likely to give birth to newborns who have a higher likelihood of being obese in adulthood [59][31]. Visceral adipose tissue (VAT) in the abdomen is associated with metabolic syndrome, IR, and an elevated risk of CVD in the future [60,61][32][33]. The detection of IR and glucose dysregulation in mid-pregnancy is correlated with an increased depth of VAT in the first trimester of pregnancy [25,37][34][35].32.1.2. Effects of Diet on Gestational IR
Diet, encompassing total calorie consumption, dietary plans, food processing, and preparation, as well as exposure to endocrine-disrupting chemicals [64[36][37],65], appears to exert a significant impact on the onset or exacerbation of IR, particularly in cases where IR already exists, such as in obesity or PCOS [66][38]. A high-fat, Western-style diet characterized by a high caloric intake is a major risk factor for developing IR, prediabetes, T2DM, and obesity [69][39]. A diet rich in fats or sugars may also significantly alter the diversity of intestinal microbial flora. However, most diet-related alterations to the gut microbiota appear to be reversible with appropriate dietary modifications [70][40]. The diet recommended for expectant women with GDM should aim to promote healthy maternal weight gain while minimizing postprandial glucose spikes and fostering fetal development. Various dietary recommendations for GDM have been compared in numerous studies, including energy-restricted versus unrestricted diets; low-CHO, -GI, and -GL diets versus high-CHO, -GI, and -GL diets; diets rich in monounsaturated fats versus high-CHO diets [71][41]; and conventional diets versus fiber-enriched diets.32.1.3. Effects of CHO and GI/GL Estimates on Gestational IR
Women with gestational GDM should exercise extra caution regarding both the quantity and type of CHOs they consume. All pregnant women require a minimum of 175 g of dietary CHOs, 71 g of protein, and 28 g of fiber daily, as CHOs serve as a vital energy source for both the mother and the fetus [75][42]. The nutrition plan should highlight monounsaturated and polyunsaturated fats while limiting saturated fats and avoiding trans fats [21][19]. A low-CHO diet is typically recommended for women with GDM, despite inconsistent findings in several studies [76][43]. Especially for women with T1DM, optimal metabolic regulation and more successful pregnancies seem to be achieved through CHO counting [77][44]. A moderately low-CHO diet comprising 40% of the recommended daily calories improves glycemic management in women with T2DM but does not demonstrate beneficial effects on pregnancy outcomes [78][45]. While a low-CHO diet improves short-term glycemic control in women with GDM, no impact on insulin requirements (in women receiving insulin treatment) or the success of pregnancies has been observed [50,79][24][46]. However, caution is advised when combining a low-CHO dietary pattern with a high consumption of animal-based protein and fat, as it appears to be associated with a higher risk of GDM and T2DM later in life [44,79][46][47]. A high GL diet has been associated with an increased risk of GDM in women, particularly when compared to those with the lowest tertile of dietary GL [81][48]. Younger gestational ages, higher CHO proportions, and lower fiber intake were strongly linked to high-GL diets [19][17]. Diets with a low GI and GL, such as the DASH diet and the Mediterranean diet, have demonstrated positive effects on various biochemical and health parameters [67,72,83][49][50][51]. Regarding obstetric and fetal outcomes in GDM patients, lower-GI diets have demonstrated potential benefits, although the findings are still debatable [81][48]. Notably, lower insulin utilization was observed in individuals adhering to a low-GI diet, characterized by the consumption of high-quality, complex CHOs [18,84,85][16][52][53]. Examining the impact on offspring, low-GI diets were associated with a decreased incidence of large-for-gestational-age (LGA) babies [85][53], as well as influences on birth length and early childhood arterial wall thickness [89][54]. The Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), insulin, and leptin levels in children were also significantly were also significantly and positively correlatedwith dietary GI during pregnancy [90][55]. Contrary to these findings, several studies suggested that GI and GL indices were not significantly associated with GDM risk [26,91][56][57]. In patients with T2DM, Ojo et al. reported no notable differences in total cholesterol, HDL cholesterol, or LDL cholesterol [82][58]. Additionally, no distinctions were found in lipids [18[16][34],25], fructosamine, glycosylated hemoglobin [18[16][34],25], overall glycemic control, or pregnancy outcomes in women with GDM.3.2. Inflammation in Gestation
2.2. Inflammation in Gestation
Low-grade inflammation induced by cytokines is a typical feature of pregnancy, playing a vital role in the finely controlled inflammatory response crucial for the development of placentation from implantation to labor [94][59]. Maternal obesity and GDM are strong risk factors for persistent low-grade inflammation. Proinflammatory cytokines have been consistently linked to inflammation induced by obesity, showing higher levels in affected individuals [90][55]. In pregnancies affected by obesity, the placenta may undergo changes in shape and function as an adaptive response, acting as both a target and a source of inflammatory cytokines [94][59]. Adipose tissue also produces several inflammatory factors that regulate hunger and fat synthesis. These pro-inflammatory mediators play a role in the development of IR, overt diabetes mellitus, and other complications related to obesity [95,96,97,98][60][61][62][63]. Regardless of maternal BMI, specific inflammatory markers have been found elevated during pregnancy in women with a history of GDM and those who later develop GDM. Circulating tumor necrosis factor-alpha (TNF-α), as a biomarker of inflammation, decreases in early pregnancy, accompanied by an increase in insulin sensitivity [40][64]. In a study by Challier et al., obese women exhibited a 2–3-fold increase in placental macrophages along with elevated mRNA expressions of interleukin-1 (IL-1), TNF-α, and interleukin-6 (IL-6) [73][65]. While lean, overweight, and obese women show similar patterns of cytokine changes, those with a higher BMI tend to exhibit an increase in specific inflammatory markers (CRP and IL-6), although not consistently across all markers [94][59]. Serum C-reactive protein (CRP) levels during the late second and early third trimesters are associated with GDM and weight gain, whereas elevated highly sensitive CRP levels in GDM patients may indicate an increased risk of later developing T2DM [99][66]。43. Postpartum Period and Long-Term Management
Following delivery, women with GDM who were not previously diagnosed as diabetic (with any type of DM, including T1DM, T2DM, MODY, and LADA) should discontinue any treatment if needed. The recommended timeframe for glycemic reassessment is six to thirteen weeks post-delivery [101][67], to decide if initiation of drug treatment is indicated. This is particularly advised if future pregnancies are planned. Healthcare providers should educate patients about the long-term risks of both T2DM and GDM during the postpartum period. Both the American Diabetes Association (ADA) [102][68] and the National Institute for Health and Care Excellence (NICE) [103][69] recommend lifelong, annual glucose level evaluations. Various risk factors, such as family history, a history of GDM in previous pregnancies, and the need for insulin or oral glucose-lowering medications during pregnancy, influence the frequency of T2DM occurrence [101][67]. Lifestyle modifications play a crucial role, especially for morbidly obese women with IR, prior GDM, or prediabetes. A diet rich in protein and regular exercise are strongly recommended, as they have proven to be more successful in reducing IR and improving glycemic variability [106][70]. Diets such as the Mediterranean and DASH diets, low in complex CHOs and GI/GL, particularly when combined with plant-based proteins and fats [44[47][71],45], are employed to reduce the likelihood of GDM in future pregnancies and the risk of developing T2DM.54. Conclusions
The use of GI and GL estimates in the management of GDM has gained attention, recognizing the substantial impact of diet on glycemic control and pregnancy outcomes for GDM patients. Research indicates that low-CHO diets, particularly in the short term, have proven beneficial for patients with T2DM. Considering that women with GDM typically have diabetes for short durations (less than six months), low-CHO/low-GI diets may also be advantageous for them. A low-GI diet, in contrast to one with a higher CHO content, has been associated with improved glycemic control, reduced insulin requirements, lower cholesterol levels, decreased inflammation markers, and enhanced obstetric outcomes. However, the data remain contradictory, with several studies reporting no significant associations. The limited number of studies examining the impact of GI and GL on GDM, the absence of a consensus on what constitutes a preferred GL/GI diet, and ethical constraints preventing the study of effects on infants and newborns except through observational studies hinder our ability to fully assess these diets’ effects. Until larger-scale intervention trials are conducted, a low-GI diet should not replace the current pregnancy diets recommended by health organizations. Achieving a general consensus on what constitutes a low-GI/-GL diet is essential to enhance clinical practice with specific dietary recommendations for GDM patients.References
- Modzelewski, R.; Stefanowicz-Rutkowska, M.M.; Matuszewski, W.; Bandurska-Stankiewicz, E.M. Gestational Diabetes Mellitus—Recent Literature Review. J. Clin. Med. 2022, 11, 5736.
- Chu, A.H.Y.; Godfrey, K.M. Gestational Diabetes Mellitus and Developmental Programming. Ann. Nutr. Metab. 2020, 76, 4–15.
- Plows, J.; Stanley, J.; Baker, P.; Reynolds, C.; Vickers, M. The Pathophysiology of Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 3342.
- Ladyman, S.R.; Brooks, V.L. Central Actions of Insulin during Pregnancy and Lactation. J. Neuroendocrinol. 2021, 33, e12946.
- Butte, N.F. Carbohydrate and Lipid Metabolism in Pregnancy: Normal Compared with Gestational Diabetes Mellitus. Am. J. Clin. Nutr. 2000, 71, 1256S–1261S.
- Duggleby, S.L.; Jackson, A.A. Protein, Amino Acid and Nitrogen Metabolism during Pregnancy: How Might the Mother Meet the Needs of Her Fetus? Curr. Opin. Clin. Nutr. Metab. Care 2002, 5, 503–509.
- Soma-Pillay, P.; Nelson-Piercy, C.; Tolppanen, H.; Mebazaa, A. Physiological Changes in Pregnancy. Cardiovasc. J. Afr. 2016, 27, 89–94.
- Rassie, K.L.; Giri, R.; Melder, A.; Joham, A.; Mousa, A.; Teede, H.J. Lactogenic Hormones in Relation to Maternal Metabolic Health in Pregnancy and Postpartum: Protocol for a Systematic Review. BMJ Open 2022, 12, e055257.
- Yahaya, T.O.; Salisu, T.; Abdulrahman, Y.B.; Umar, A.K. Update on the Genetic and Epigenetic Etiology of Gestational Diabetes Mellitus: A Review. Egypt. J. Med. Hum. Genet. 2020, 21, 13.
- Kuang, Y.-S.; Lu, J.-H.; Li, S.-H.; Li, J.-H.; Yuan, M.-Y.; He, J.-R.; Chen, N.-N.; Xiao, W.-Q.; Shen, S.-Y.; Qiu, L.; et al. Connections between the Human Gut Microbiome and Gestational Diabetes Mellitus. Gigascience 2017, 6, gix058.
- Ormazabal, V.; Nair, S.; Carrión, F.; Mcintyre, H.D.; Salomon, C. The Link between Gestational Diabetes and Cardiovascular Diseases: Potential Role of Extracellular Vesicles. Cardiovasc. Diabetol. 2022, 21, 174.
- Nguyen-Ngo, C.; Jayabalan, N.; Salomon, C.; Lappas, M. Molecular Pathways Disrupted by Gestational Diabetes Mellitus. J. Mol. Endocrinol. 2019, 63, R51–R72.
- Abu Samra, N.; Jelinek, H.F.; Alsafar, H.; Asghar, F.; Seoud, M.; Hussein, S.M.; Mubarak, H.M.; Anwar, S.; Memon, M.; Afify, N.; et al. Genomics and Epigenomics of Gestational Diabetes Mellitus: Understanding the Molecular Pathways of the Disease Pathogenesis. Int. J. Mol. Sci. 2022, 23, 3514.
- Dias, S.; Pheiffer, C.; Abrahams, Y.; Rheeder, P.; Adam, S. Molecular Biomarkers for Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2018, 19, 2926.
- Dłuski, D.F.; Wolińska, E.; Skrzypczak, M. Epigenetic Changes in Gestational Diabetes Mellitus. Int. J. Mol. Sci. 2021, 22, 7649.
- Markovic, T.P.; Muirhead, R.; Overs, S.; Ross, G.P.; Louie, J.C.Y.; Kizirian, N.; Denyer, G.; Petocz, P.; Hyett, J.; Brand-Miller, J.C. Randomized Controlled Trial Investigating the Effects of a Low–Glycemic Index Diet on Pregnancy Outcomes in Women at High Risk of Gestational Diabetes Mellitus: The GI Baby 3 Study. Diabetes Care 2016, 39, 31–38.
- Tieu, J.; Shepherd, E.; Middleton, P.; Crowther, C.A. Dietary Advice Interventions in Pregnancy for Preventing Gestational Diabetes Mellitus. Cochrane Database Syst. Rev. 2017, 1, CD006674.
- Damm, P.; Houshmand-Oeregaard, A.; Kelstrup, L.; Lauenborg, J.; Mathiesen, E.R.; Clausen, T.D. Gestational Diabetes Mellitus and Long-Term Consequences for Mother and Offspring: A View from Denmark. Diabetologia 2016, 59, 1396–1399.
- Elsayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes—2023. Diabetes Care 2023, 46, S254–S266.
- Hodson, K.; Dalla Man, C.; Smith, F.; Thelwall, P.; Cobelli, C.; Robson, S.; Taylor, R. Mechanism of Insulin Resistance in Normal Pregnancy. Horm. Metab. Res. 2013, 45, 567–571.
- Kampmann, U.; Knorr, S.; Fuglsang, J.; Ovesen, P. Determinants of Maternal Insulin Resistance during Pregnancy: An Updated Overview. J. Diabetes Res. 2019, 2019, 5320156.
- Catalano, P.M. Trying to Understand Gestational Diabetes. Diabet. Med. 2014, 31, 273–281.
- Jang, E.-H.; Kwon, H.-S. β-Cell Dysfunction and Insulin Resistance in Gestational Glucose Intolerance. Korean J. Intern. Med. 2013, 28, 294.
- Moreno-Castilla, C.; Hernandez, M.; Bergua, M.; Alvarez, M.C.; Arce, M.A.; Rodriguez, K.; Martinez-Alonso, M.; Iglesias, M.; Mateu, M.; Santos, M.D.; et al. Low-Carbohydrate Diet for the Treatment of Gestational Diabetes Mellitus. Diabetes Care 2013, 36, 2233–2238.
- Zhu, Y.; Zhang, C. Prevalence of Gestational Diabetes and Risk of Progression to Type 2 Diabetes: A Global Perspective. Curr. Diab. Rep. 2016, 16, 7.
- Walsh, J.M.; Mahony, R.M.; Culliton, M.; Foley, M.E.; McAuliffe, F.M. Impact of a Low Glycemic Index Diet in Pregnancy on Markers of Maternal and Fetal Metabolism and Inflammation. Reprod. Sci. 2014, 21, 1378–1381.
- Tang, J.; Chen, R.; Yu, Y.; Bao, W.; Tiemeier, H.; Rodney, A.; Zhu, X.; Li, M.; Huang, D.; Zhao, Q. Associations of Pre-Pregnancy Impaired Fasting Glucose and Body Mass Index among Pregnant Women without Pre-Existing Diabetes with Offspring Being Large for Gestational Age and Preterm Birth: A Cohort Study in China. BMJ Open Diabetes Res. Care 2021, 9, e001641.
- Shinar, S.; Berger, H.; De Souza, L.R.; Ray, J.G. Difference in Visceral Adipose Tissue in Pregnancy and Postpartum and Related Changes in Maternal Insulin Resistance. J. Ultrasound Med. 2019, 38, 667–673.
- Gallagher, K.; Migliaccio, L.; Rogers, R.G.; Leeman, L.; Hervey, E.; Qualls, C. Impact of Nulliparous Women’s Body Mass Index or Excessive Weight Gain in Pregnancy on Genital Tract Trauma at Birth. J. Midwifery Womens. Health 2014, 59, 54–59.
- Walsh, J.M.; Byrne, J.; Mahony, R.M.; Foley, M.E.; McAuliffe, F.M. Leptin, Fetal Growth and Insulin Resistance in Non-Diabetic Pregnancies. Early Hum. Dev. 2014, 90, 271–274.
- Powe, C.E.; Huston Presley, L.P.; Locascio, J.J.; Catalano, P.M. Augmented Insulin Secretory Response in Early Pregnancy. Diabetologia 2019, 62, 1445–1452.
- Peppa, M.; Koliaki, C.; Papaefstathiou, A.; Garoflos, E.; Katsilambros, N.; Raptis, S.A.; Hadjidakis, D.I.; Dimitriadis, G.D. Body Composition Determinants of Metabolic Phenotypes of Obesity in Nonobese and Obese Postmenopausal Women. Obesity 2013, 21, 1807–1814.
- Peppa, M.; Koliaki, C.; Hadjidakis, D.I.; Garoflos, E.; Papaefstathiou, A.; Katsilambros, N.; Raptis, S.A.; Dimitriadis, G.D. Regional Fat Distribution and Cardiometabolic Risk in Healthy Postmenopausal Women. Eur. J. Intern. Med. 2013, 24, 824–831.
- Kizirian, N.V.; Goletzke, J.; Brodie, S.; Atkinson, F.S.; Markovic, T.P.; Ross, G.P.; Buyken, A.; Brand-Miller, J.P. Lower Glycemic Load Meals Reduce Diurnal Glycemic Oscillations in Women with Risk Factors for Gestational Diabetes. BMJ Open Diabetes Res. Care 2017, 5, e000351.
- Kunath, J.; Günther, J.; Rauh, K.; Hoffmann, J.; Stecher, L.; Rosenfeld, E.; Kick, L.; Ulm, K.; Hauner, H. Effects of a Lifestyle Intervention during Pregnancy to Prevent Excessive Gestational Weight Gain in Routine Care—The Cluster-Randomised GeliS Trial. BMC Med. 2019, 17, 5.
- Tang, Z.-R.; Xu, X.-L.; Deng, S.-L.; Lian, Z.-X.; Yu, K. Oestrogenic Endocrine Disruptors in the Placenta and the Fetus. Int. J. Mol. Sci. 2020, 21, 1519.
- Darbre, P.D. Endocrine Disruptors and Obesity. Curr. Obes. Rep. 2017, 6, 18–27.
- Louie, J.C.Y.; Brand-Miller, J.C.; Markovic, T.P.; Ross, G.P.; Moses, R.G. Glycemic Index and Pregnancy: A Systematic Literature Review. J. Nutr. Metab. 2010, 2010, 282464.
- Verboven, M.; Deluyker, D.; Ferferieva, V.; Lambrichts, I.; Hansen, D.; Eijnde, B.O.; Bito, V. Western Diet given to Healthy Rats Mimics the Human Phenotype of Diabetic Cardiomyopathy. J. Nutr. Biochem. 2018, 61, 140–146.
- He, L. Alterations of Gut Microbiota by Overnutrition Impact Gluconeogenic Gene Expression and Insulin Signaling. Int. J. Mol. Sci. 2021, 22, 2121.
- Osorio-Yáñez, C.; Gelaye, B.; Qiu, C.; Bao, W.; Cardenas, A.; Enquobahrie, D.A.; Williams, M.A. Maternal Intake of Fried Foods and Risk of Gestational Diabetes Mellitus. Ann. Epidemiol. 2017, 27, 384–390.e1.
- Mustad, V.A.; Huynh, D.T.T.; López-Pedrosa, J.M.; Campoy, C.; Rueda, R. The Role of Dietary Carbohydrates in Gestational Diabetes. Nutrients 2020, 12, 385.
- Schenk, S.; Andrey, M.; De Giorgi, S.; Le Dizes, O.; Puder, J.J. What Is the Place of a Low Carbohydrate or Low Glycemic Index Diet in Gestational Diabetes Treatment? Rev. Med. Suisse 2021, 17, 1083–1086.
- Holt, R.I.G.; DeVries, J.H.; Hess-Fischl, A.; Hirsch, I.B.; Kirkman, M.S.; Klupa, T.; Ludwig, B.; Nørgaard, K.; Pettus, J.; Renard, E.; et al. The Management of Type 1 Diabetes in Adults. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2021, 64, 2609–2652.
- Roskjær, A.B.; Andersen, J.R.; Ronneby, H.; Damm, P.; Mathiesen, E.R. Dietary Advices on Carbohydrate Intake for Pregnant Women with Type 1 Diabetes. J. Matern. Neonatal Med. 2015, 28, 229–233.
- Bao, W.; Li, S.; Chavarro, J.E.; Tobias, D.K.; Zhu, Y.; Hu, F.B.; Zhang, C. Low Carbohydrate–Diet Scores and Long-Term Risk of Type 2 Diabetes Among Women With a History of Gestational Diabetes Mellitus: A Prospective Cohort Study. Diabetes Care 2016, 39, 43–49.
- Bao, W.; Bowers, K.; Tobias, D.K.; Olsen, S.F.; Chavarro, J.; Vaag, A.; Kiely, M.; Zhang, C. Prepregnancy Low-Carbohydrate Dietary Pattern and Risk of Gestational Diabetes Mellitus: A Prospective Cohort Study. Am. J. Clin. Nutr. 2014, 99, 1378–1384.
- Zhang, X.; Gong, Y.; Della Corte, K.; Yu, D.; Xue, H.; Shan, S.; Tian, G.; Liang, Y.; Zhang, J.; He, F.; et al. Relevance of Dietary Glycemic Index, Glycemic Load and Fiber Intake before and during Pregnancy for the Risk of Gestational Diabetes Mellitus and Maternal Glucose Homeostasis. Clin. Nutr. 2021, 40, 2791–2799.
- Wang, J.-S.; Liu, W.-J.; Lee, C.-L. Associations of Adherence to the DASH Diet and the Mediterranean Diet With All-Cause Mortality in Subjects With Various Glucose Regulation States. Front. Nutr. 2022, 9, 828792.
- Gołąbek, K.; Regulska-Ilow, B. Dietary Support in Insulin Resistance: An Overview of Current Scientific Reports. Adv. Clin. Exp. Med. 2019, 28, 1577–1585.
- Critselis, E.; Kontogianni, M.D.; Georgousopoulou, E.; Chrysohoou, C.; Tousoulis, D.; Pitsavos, C.; Panagiotakos, D.B. Comparison of the Mediterranean Diet and the Dietary Approach Stop Hypertension in Reducing the Risk of 10-Year Fatal and Non-Fatal CVD Events in Healthy Adults: The ATTICA Study (2002–2012). Public Health Nutr. 2021, 24, 2746–2757.
- Mahajan, A.; Donovan, L.E.; Vallee, R.; Yamamoto, J.M. Evidenced-Based Nutrition for Gestational Diabetes Mellitus. Curr. Diab. Rep. 2019, 19, 94.
- Wei, J.; Heng, W.; Gao, J. Effects of Low Glycemic Index Diets on Gestational Diabetes Mellitus. Medicine 2016, 95, e3792.
- Skilton, M.R.; Siitonen, N.; Würtz, P.; Viikari, J.S.A.; Juonala, M.; Seppälä, I.; Laitinen, T.; Lehtimäki, T.; Taittonen, L.; Kähönen, M.; et al. High Birth Weight Is Associated With Obesity and Increased Carotid Wall Thickness in Young Adults. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1064–1068.
- Danielsen, I.; Granström, C.; Haldorsson, T.; Rytter, D.; Hammer Bech, B.; Henriksen, T.B.; Vaag, A.A.; Olsen, S.F. Dietary Glycemic Index during Pregnancy Is Associated with Biomarkers of the Metabolic Syndrome in Offspring at Age 20 Years. PLoS ONE 2013, 8, e64887.
- Hasbullah, F.Y.; Mohd Yusof, B.N.; Shariff, Z.M.; Rejali, Z.; Yong, H.Y.; Mitri, J. Factors Associated with Dietary Glycemic Index and Glycemic Load in Pregnant Women and Risk for Gestational Diabetes Mellitus. Int. J. Food Sci. Nutr. 2020, 71, 516–524.
- Aminianfar, A.; Soltani, S.; Hajianfar, H.; Azadbakht, L.; Shahshahan, Z.; Esmaillzadeh, A. The Association between Dietary Glycemic Index and Load and Risk of Gestational Diabetes Mellitus: A Prospective Study. Diabetes Res. Clin. Pract. 2020, 170, 108469.
- Ojo, O.; Ojo, O.O.; Wang, X.-H.; Adegboye, A.R.A. The Effects of a Low GI Diet on Cardiometabolic and Inflammatory Parameters in Patients with Type 2 and Gestational Diabetes: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Nutrients 2019, 11, 1584.
- Pantham, P.; Aye, I.L.M.H.; Powell, T.L. Inflammation in Maternal Obesity and Gestational Diabetes Mellitus. Placenta 2015, 36, 709–715.
- Szlapinski, S.K.; Hill, D.J. Metabolic Adaptations to Pregnancy in Healthy and Gestational Diabetic Pregnancies: The Pancreas—Placenta Axis. Curr. Vasc. Pharmacol. 2020, 19, 141–153.
- Trojnar, M.; Patro-Małysza, J.; Kimber-Trojnar, Ż.; Leszczyńska-Gorzelak, B.; Mosiewicz, J. Associations between Fatty Acid-Binding Protein 4–A Proinflammatory Adipokine and Insulin Resistance, Gestational and Type 2 Diabetes Mellitus. Cells 2019, 8, 227.
- Yang, H.; Youm, Y.-H.; Vandanmagsar, B.; Ravussin, A.; Gimble, J.M.; Greenway, F.; Stephens, J.M.; Mynatt, R.L.; Dixit, V.D. Obesity Increases the Production of Proinflammatory Mediators from Adipose Tissue T Cells and Compromises TCR Repertoire Diversity: Implications for Systemic Inflammation and Insulin Resistance. J. Immunol. 2010, 185, 1836–1845.
- Rehman, K.; Akash, M.S.H. Mechanisms of Inflammatory Responses and Development of Insulin Resistance: How Are They Interlinked? J. Biomed. Sci. 2016, 23, 87.
- Fernández-González, E.; Martínez-González, M.Á.; Bes-Rastrollo, M.; Suescun-Elizalde, D.; Basterra-Gortari, F.J.; Santiago, S.; Gea, A. Association between Pre-Conceptional Carbohydrate Quality Index and the Incidence of Gestational Diabetes: The SUN Cohort Study. Br. J. Nutr. 2023, 129, 704–714.
- Messika, A.; Toledano, Y.; Hadar, E.; Shmuel, E.; Tauman, R.; Shamir, R.; Froy, O. Relationship among Chrononutrition, Sleep, and Glycemic Control in Women with Gestational Diabetes Mellitus: A Randomized Controlled Trial. Am. J. Obstet. Gynecol. MFM 2022, 4, 100660.
- Kominiarek, M.A.; Rajan, P. Nutrition Recommendations in Pregnancy and Lactation. Med. Clin. N. Am. 2016, 100, 1199–1215.
- Egan, A.M.; Dunne, F.P. Optimal Management of Gestational Diabetes. Br. Med. Bull. 2019, 131, 97–108.
- Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S200–S210.
- NICE Guideline Diabetes in Pregnancy: Management from Preconception to the Postnatal. Available online: www.nice.org.uk/guidance/ng3 (accessed on 25 February 2023).
- Tettamanzi, F.; Bagnardi, V.; Louca, P.; Nogal, A.; Monti, G.S.; Mambrini, S.P.; Lucchetti, E.; Maestrini, S.; Mazza, S.; Rodriguez-Mateos, A.; et al. A High Protein Diet Is More Effective in Improving Insulin Resistance and Glycemic Variability Compared to a Mediterranean Diet—A Cross-Over Controlled Inpatient Dietary Study. Nutrients 2021, 13, 4380.
- Looman, M.; Schoenaker, D.A.J.M.; Soedamah-Muthu, S.S.; Geelen, A.; Feskens, E.J.M.; Mishra, G.D. Pre-Pregnancy Dietary Carbohydrate Quantity and Quality, and Risk of Developing Gestational Diabetes: The Australian Longitudinal Study on Women’s Health. Br. J. Nutr. 2018, 120, 435–444.
