Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Ralf Weiskirchen and Version 2 by Catherine Yang.
Obesity or excessive weight gain is identified as the most important and significant risk factor in the development and progression of type 2 diabetes mellitus (DM) in all age groups. It has reached pandemic dimensions, making the treatment of obesity crucial in the prevention and management of type 2 DM worldwide.
- obesity
- type 2 diabetes
- pathophysiology
- management
1. Introduction
The rapid development of global urbanization and modernization has lasting effects on lifestyle aspects such as unhealthy eating habits, lack of exercise, increased stress and environmental factors. These factors contribute to the alarming growth of obesity and type 2 DM worldwide. Obese individuals develop insulin resistance, which is characterized by impaired insulin action in the liver and reduced glucose uptake in fat and muscle [1]. While lifestyle changes and medications are recommended for prevention, they have not been successful in suppressing the increasing incidence conditions. Therefore, it is crucial to gain a deeper understanding of the molecular mechanisms linking obesity and type 2 DM in order to address this global healthcare challenge effectively.
The intricate connections and sharing of pathophysiological mechanisms between obesity and type 2 DM amplify the prevalence and incidence of insulin resistance, dyslipidemia, NAFLD and a constellation of metabolic abnormalities in obese individuals. Increased body mass index (BMI) and abdominal fat distribution linearly increases the risk of type 2 DM due to alterations in adipose tissue biology that links obesity with insulin resistance and beta cell dysfunction [1]. Abdominal obesity, commonly determined by waist-to-hip ratio, is an independent factor for the development of hypertension and elevated fasting glucose, even if the overweight individual with predominant abdominal fat does not meet the BMI criteria for obesity [2]. Multiple in vivo and clinical studies have demonstrated a cause-and-effect relationship between obesity and type 2 DM, unraveling their intimate connections. It is shocking to note that according to the WHO fact sheet, at least 41 million children under the age 5 are overweight or obese (BMI ≥ 35 kg/m2) as of 2016. If this trend continues, 60% of the world’s population will be obese or overweight by 2030 [3]. According to WHO, obesity accounts for 44% of diabetes and the incidence of obesity-related diabetes is expected to double to 300 million by 2025 [4].
It is interesting to note that during starvation, adipose tissue, which serves as a major fuel reserve, provides a critical energy source for survival. Additionally, adipose tissue modifies various physiological functions, including appetite, reproduction and insulin action, through the secretion of adipokines and exosomes [1]. In obese individuals, non-esterified fatty acids play a crucial role in the development of insulin resistance and beta cell dysfunction [1].
The close relationship between obesity and diabetes has led to the term “diabesity”, which highlights that the majority of individuals with diabetes are obese or overweight [5]. While type 2 DM is influenced by genetic predisposition and ethnicity which are non-modifiable risk factors, it can still be prevented or managed by addressing modifiable risk factors such as obesity. Despite recent advancement in management strategies, obesity and diabetes remain a significant interconnected public health challenge worldwide.
2. Obesity and Type 2 DM
Obesity is defined as the excessive accumulation of fat in various parts of the body or organs, known as ectopic fat or throughout the body. It is a chronic, progressive, relapsing condition with multiple factors that lead to adverse metabolic and psychosocial health consequences [6]. One of the main causes of obesity is an imbalance between the excess energy stored and the energy utilized by the body, which can disrupt nutrient signals and result in insufficient energy expenditure [6]. Assessing the risk factors for adiposity involves measuring height, weight, BMI, waist circumference and body fat percentage. The diagnosis of obesity relies on the BMI cut off and the relationship between body weight, fat distribution pattern and visceral fat [7]. BMI alone is no longer sufficient to evaluate obesity, as it is a diverse condition. Table 1 displays the classification of obesity based on BMI and waist circumference [7].Table 1.
Classification of obesity based on body mass index and waist circumferences.
| Condition | BMI (kg/m2) | Disease Risk Relative to Normal Weight and Waist Circumference Men ≤ 40 inches (≤102 cm) Women ≤ 35 inches (≤88 cm) |
|---|---|---|
| Normal | 18.5–24.9 | data |
| Overweight | 25.0–29.9 | Increased |
| Obese | 30.0–34.9 (class 1) | High |
| 35.0–39.9 (class 2) | Very high | |
| Extremely Obese | ≥40 | Extremely high |
Table 2.
Anthropometric assessment of body fat percentage as a measure of adiposity.
| Condition | Males | Females |
|---|---|---|
| Essential fat | <15% | <10% |
| Athletes | 15–19% | 10–14% |
| Fit | 20–24% | 15–19% |
| Acceptable | 25–29% | 20–24% |
| Pre-obesity | 30–34% | 25–29% |
| Obesity | >35% | >30% |
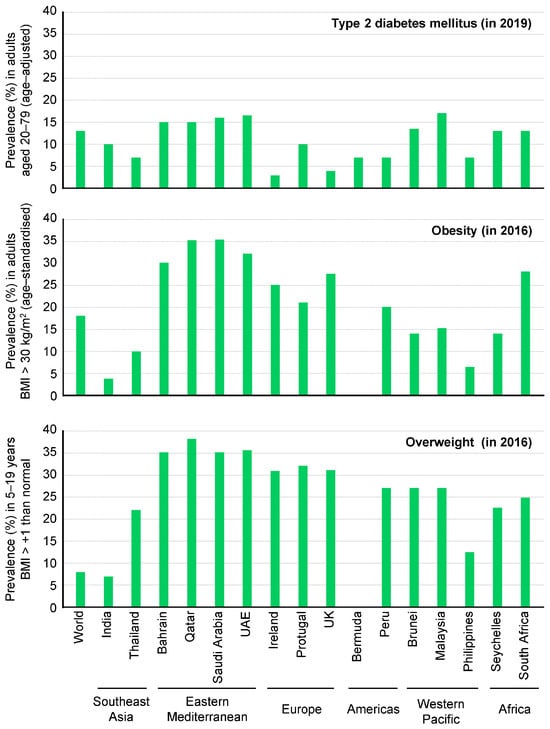
Figure 1. Prevalence of type 2 diabetes mellitus (in 2019), obesity (in 2016) and overweight (in 2016) in selected countries. This figure has been redrawn in a modified form from [19].
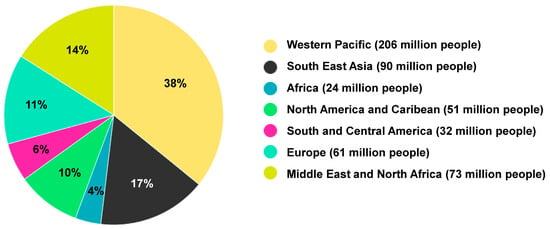
Figure 2. Prevalence of diabetes worldwide in 2021. A total of 573 million people suffered from diabetes in 2021. The figure has been redrawn and modified based on information from [26].
