Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 1 by Marcus Antônio Rossi Feliciano.
Contrast-enhanced ultrasonography is based on the intravenous injection of contrast media constituted by microbubbles. This imaging modality provides information on the tissue perfusion and allows the investigation of macro- and micro-circulation. Studies on different organs and tissues were performed in dogs and cats and revealed a tendency of malignant tumors to present faster transit of the contrast media (time to wash in, peak and wash out). These advanced techniques associated with other imaging modalities can be used as screening tests and can potentially represent an alternative to the invasive sampling methods required for cytological and histopathological analysis.
- elastography
- contrast-enhanced ultrasound
- neoplasia
- metastasis
- feline
- canine
1. Introduction to Elastography
Elastography is a relatively new ultrasonographic technology, created in the 1990s [1], that is noninvasive and used to measure the stiffness or elasticity of tissues [2]. There are two main forms of elastography used as diagnostic methods, static elastography, and dynamic elastography [2]. The authors described static elastography or the strain-wave modality as involving manual pressure from the transducer on the area under study, compressing the tissue to measure the relative tissue displacement. In this technique, the echoes are acquired before and after slight compression of the tissue using the sonographic probe. After compression, a sample of linear echoes are obtained. The data are, therefore, compared with cross-correlation techniques [3].
Dynamic elastography encompasses shear-wave elastography techniques. Sonoelastography (Fibroscan®, EchoSens, Paris, France) involves low-frequency vibration (20 Hz to 1000 Hz) externally applied to produce internal vibrations in the tissue under study. It allows quantifying the propagation and speed of the shear waves (expressed in kilopascals—kPa). This technique consists of exciting a tissue using harmonic vibration, producing low-frequency and high-amplitude waves. The low frequencies reduce the attenuation, allow deeper penetration, and avoid damages to the neighboring tissues [3]. Shear-wave speed is directly related to tissue stiffness. Therefore, the stiffer the tissue, the faster the shear-wave propagation (higher kPa) [4].
Shear-wave elastography evaluates tissue displacement from a force caused by a focused, high-intensity sound beam that produces shear waves [2]. These waves laterally pass through the tissue at a speed between 1 to 10 m/s and are rapidly attenuated by organic tissues. This method has lower inter-observer variability compared to manual compression elastography [1] and can be performed using commercially available equipment other than Fibroscan®, such as Acoustic Radiation Force Impulse (ARFI) (Siemens, Munich, Germany) or SuperSonic Shear-wave Imaging (SuperSonic Imaging, Aix-en-Provence, France) [5].
Several studies have used elastography for assessing hepatic fibrosis in humans as a preliminary assessment before tissue biopsies or for predicting and detecting malignancy [5[5][6],7], as well as for assessing acute and chronic kidney diseases [8][7]. In veterinary medicine, recent studies have explored elastography for evaluating the prostate [9[8][9][10],10,11], liver [12][11], and kidneys in dogs and cats [2[2][8],9], as well as for assessing hepatic fibrosis [13][12], lymph nodes [2[2][13][14][15][16][17][18][19][20][21],14,15,16,17,18,19,20,21,22], and mammary neoplasms [1,4,23,24,25][1][4][22][23][24]. Elastography has been shown to be a promising diagnostic method in the evaluation and prediction of neoplasm malignancy, mainly due to its safety and low invasiveness [1].
2. Applicability of Elastography
2.1. Mammary Glands
Mammary neoplasia is highly prevalent in dogs and can cause severe consequences to the animals [26][25]. For this reason, its diagnosis and treatment must be very aggressive and effective. Mammary neoplasia presents several molecular and clinicopathological similarities with mammary tumors in women [27][26]. A study of elastography for canine mammary tumors was able to differentiate benign nodules (such as mammary hyperplasia, adenoma, fibroadenoma and mixed benign tumors) and malignant tumors (such as tubular carcinoma, complex tubular papilliferous carcinoma, mixed carcinoma, simple solid carcinoma, and complex carcinoma) [1]. This study reported that malignant mammary nodules were more rigid and, therefore, presented a higher mean shear-wave velocity (3.33 m/s) when compared to benign nodules (1.28 m/s). ARFI elastography and other imaging modalities were used to investigate 300 mammary masses in dogs [23][22]. The authors reported that a shear-wave velocity higher than 2.57 m/s presented a sensitivity of 94.7%, a specificity of 97.2%, and high accuracy for the detection of malignancy. The researchers explained that malignant mammary tumors presented high stiffness and high shear-wave velocity. They said that this event can be explained by the stromal reaction induced by the carcinoma and is associated with increased collagen fibers in the mammary tissue.2.2. Lymph Nodes
Lymph node evaluation is paramount to staging oncological patients since the presence of metastatic lymph nodes indicates negative prognostics. The sentinel lymph node is the first draining lymph node, and its location can optimize the success of tissue sampling for histopathology or cytology [28][27]. The diagnosis of lymphadenopathies is routinely performed with fine needle aspiration cytology. Some limitations of this method include the (frequent) insufficient amount of tumoral cells obtained in the samples and the high possibility of sample contamination, producing false negative results. B-mode ultrasonography is the first-choice imaging modality used to screen for lymph node metastasis. However, as with cytology, the ultrasound has some limitations due to the overlap of findings between benign inflammatory and neoplastic etiologies [14][13]. ARFI elastography was reported to be more sensitive and specific than the short/long axis ratio (evaluated with B-mode ultrasound) for the detection of axillary and inguinal metastatic lymph nodes in bitches with mammary neoplasia. The metastatic lymph nodes of bitches with mammary tumors were more rigid than reactive or normal lymph nodes [15][14], with an accuracy higher than 95% for the detection of malignant lymphoid tissues.2.3. Spleen
Splenic tumors are quite common in small animal clinics, especially in dogs. Approximately 58% of tumors larger than 1 cm in their largest axis are considered malignant, with hemangiosarcoma being the most frequent [35][28]. However, size, shape, and other characteristics from the B-mode ultrasound examination do not safely allow the differentiation between malignant and benign tumors, as benign and malignant neoplasms often share very similar echotexture and echogenicity patterns [36][29]. Strain elastography was used to differentiate malignant and benign hypoechoic splenic lesions smaller than 4 cm in width based on the elasticity index and stiffness value. Malignant lesions presented elasticity rates equal to or greater than 1.5 and stiffness values higher than 70% [37][30]. T2.4. Cutaneous Nodules
The cutaneous tissues, like other tissues and organs previously described, benefit from the association between different imaging modalities, such as B-mode, power Doppler and elastography, that contribute to increasing the specificity of the evaluations [38][31]. Strain elastography was able to differentiate some cutaneous nodules, such as mastocytoma and benign follicular tumors. They presented the highest elasticity scores among the neoplastic nodules. Calcified and nonvascularized nodules presented higher elasticity scores, and there was a negative correlation between the longitudinal diameter of the cutaneous nodules and qualitative elastographic parameters [39][32]. ARFI elastography associated malignant cutaneous and subcutaneous lesions with nondeformable tissues and shear-wave velocities > 3.52 m/s [38][31]. Similarly, another study compared lipomas and malignant cutaneous tumors and attributed the higher stiffness score to malignant lesions [40][33].2.5. Liver
B-mode ultrasonography is the first-choice method for hepatic evaluation in dogs and cats due to its advantages of being a noninvasive, quick and low-cost technique with high sensitivity for the detection of nodular or cystic lesions [12][11]. Hepatic lesions were submitted to a qualitative evaluation using an elastogram, where regions in blue represented rigid tissues, green spots were intermediate, and regions in red corresponded to soft tissues. Malignant hepatic lesions were presented in blue, indicating rigid tissues. In addition, the average intensity of colors in the elastogram was higher in cases of malignant tumors [41][34]. Elastography can present some limitations for hepatic evaluation, as higher frequency transducers are not able to promote adequate tissue deformation in deeper hepatic regions. Evaluations of deeper lesions or those in deep-chested or large-breed dogs are limited [41][34].2.6. Prostate and Testes
Ultrasound in its various modalities (such as B-mode and Doppler, for example) has limitations in differentiating prostatic and testicular lesions by producing nonspecific information about these lesions [9][8]. Therefore, elastography appears to be a promising method, providing additional information for distinguishing different types of lesions in the prostate and testicles of dogs and cats or allowing the delineation of the lesion area for puncture and material collection. Studies involving elastographic evaluations of prostatic and testicular conditions in domestic cats are scarce. Descriptions of normal elastographic parameters of the prostate and testicles of cats can also contribute to the differentiation of benign and malignant tumors, as malignant tumors are typically characterized as rigid and with high shear-wave velocities [42][35].3. Introduction to Contrast-Enhanced Ultrasonography (CEUS)
Contrast-enhanced ultrasonography (CEUS) was introduced with more confidence and security in medicine in the 90s to evaluate cardiac perfusion [44][36]. Currently, this imaging modality is being widely used in medicine and veterinary medicine to evaluate renal tissue perfusion and hepatic, reproductive, and neoplastic tissues, for example [44,45,46,47,48,49][36][37][38][39][40][41]. This imaging modality is based on the use of an intravenous injection of contrast media composed of microbubbles [50][42]. The same authors stated that more recent products available commercially act exclusively in the intravascular region and are composed of a lipoprotein capsule containing microbubbles of a gas with a high molecular weight and low solubility in water. The researchers emphasized that these characteristics grant higher stability and longer time in circulation. One of the main advantages of CEUS is the possibility of real time studies when compared to other contrast-enhanced exams such as magnetic resonance imaging (MRI) and computed tomography (CT), where evaluation occurs after the injection of the contrast medium [47][39] and the evaluation of nonsedated dogs when compared to CT and MRI [46][38]. CEUS is a quali-quantitative evaluation based on the study of the enhancement of patterns and the measurement of perfusion parameters, such as mean transit time (time from contrast injection until its complete clearance) [49][41].4. Applicability of CEUS
4.1. Male Reproductive Tract
There are several studies describing the use of contrast-enhanced ultrasound to evaluate the male reproductive tract in dogs. A study described the ultrasonographic aspect of different testicular tumors with CEUS [45][37]. These authors observed that testes with interstitial cell tumors presented inhomogeneous enhancement patterns with focal hyperechoic lesions in many of the cases. The same study reported that testes with seminoma presented homogeneous hyperechoic sign, persistent intra-tumoral vessels and iso- or hypoechoic parenchyma. Other findings described Sertoli tumors as inhomogeneous, with focal hyperechoic homogeneous or heterogeneous lesions, and a hyperechoic peripheral rim. In general, this study stated that inhomogeneous testes with hyperechoic lesions were associated with malignancy, with 87% sensitivity and a 100% positive predictive value.4.2. Mammary Glands
Physiological alterations in the perfusion, size and the ultrasonographic aspect of mammary glands during the estrous cycle were investigated in bitches and represent the basis for the detection of mammary gland pathologies [50][42]. According to this study, during diestrus, all mammary glands increased in thickness and were presented as heterogeneous (B-mode ultrasonography), with a heterogeneous enhancement pattern (CEUS). The authors pointed out that abdominal cranial mammary glands presented an increase in the average transit time between estrus and late diestrus and a decrease between the end of diestrus and anestrus. Another finding was that inguinal mammary glands presented higher times to peak during anestrus when compared to estrus.4.3. Kidneys and Urinary Bladder
Kidneys present a three-phased contrast enhancement consisting of an early arterial phase—in which there is rapid contrast enhancement due to the arterial blood supply—followed by a cortical phase marked by intense and uniform enhancement of the renal parenchyma, and a medullary phase, when the pyramids gradually uptake contrast until they are isochoic with the cortex [51,55][43][44]. Different types of renal tumors presented specific characteristics when evaluated with CEUS [56][45]. These authors reported that renal carcinomas presented large tortuous arteries with early contrast enhancement when compared to a normal renal parenchyma. Comparatively, in the same study, histiocytic sarcomas and lymphomas were less vascularized, with smaller arteries and early wash out during the corticomedullary phase. In the corticomedullary phase (late), renal carcinomas presented homo- or heterogeneous, iso- or hypoechoic enhancement patterns, with progressive wash out. Metastasis of hemangiosarcoma presented no contrast enhancement in any phase (neither arterial nor corticomedullary). In addition to some particularities of each tumor type, there were some overlapping findings among malignant and benign tumors [56][45].4.4. Lymph Nodes
Peripheral lymph nodes were evaluated with CEUS and power Doppler. CEUS was able to detect twice as many blood vessels as the power Doppler investigation. Lymphomatous nodes presented hilar vessel displacement, neovascularization, and loss of the hyperechoic rim. The majority of the lymph nodes presented moderate to good perfusion with a homogeneous perfusion pattern [59][46].4.5. Spleen
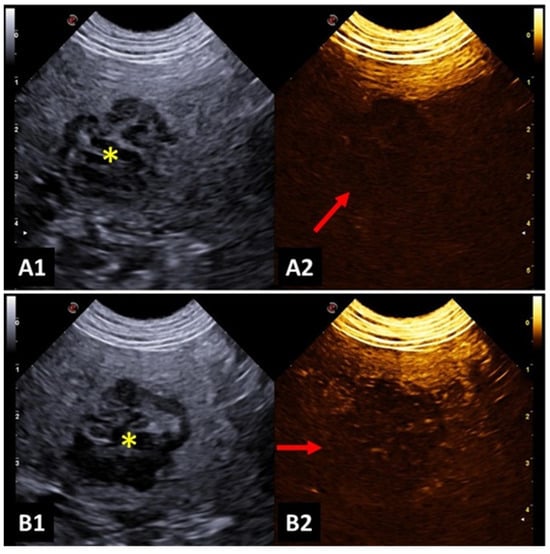
A study investigated focal splenic lesions with CEUS and reported that a hypoechoic lesion during wash out, which is associated with tortuous vessels, was suggestive of malignancy (Figure 31). Meanwhile, benign lesions presented a perfusion pattern similar to the adjacent splenic parenchyma. The same study found that hemangiosarcoma was presented as a large mass, with no perfusion in any phase, surrounded by a hypervascular splenic parenchyma. Lymphosarcoma presented faster time to peak and early wash out, with a honeycomb enhancement pattern during wash out [60][47].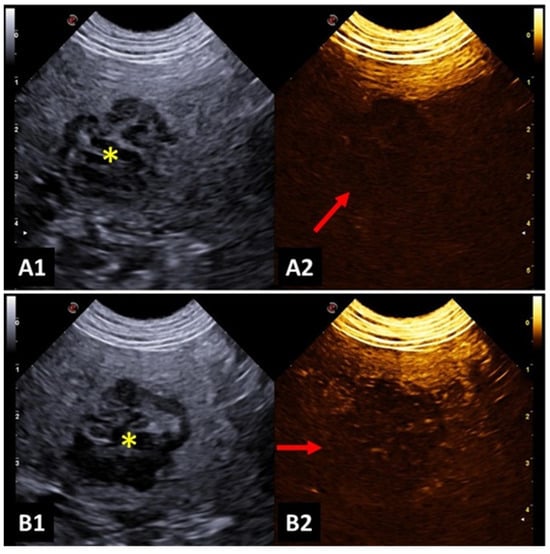
Figure 31. Image of malignant splenic lesion in a dog: (A1,B1) B-mode image of the splenic lesion with mixed and heterogeneous echogenicity; (A2) Contrast-enhanced ultrasonography (CEUS) image before contrast filling; (B2) hypointense splenic lesion during contrast wash out, indicating characteristics of malignancy. Yellow asterisk indicates lesions.
4.6. Gastrointestinal Tract
Gastric neoplasia in dogs can be characterized using B-mode ultrasonography as severe gastric wall thickening (exceeding 1.2 cm), marked loss of the wall layering, and involvement of adjacent structures (i.e., regional lymphadenomegaly and steatites) [62][48]. Other authors mentioned that focal gastric wall thickness with loss of the normal wall layering may suggest gastric neoplasms [63][49]. Those features (to a much lesser extent) can be observed in cases of inflammatory conditions, with the exception of the involvement of lymph nodes and steatites [62][48].
There may be some differences in the symmetry of the wall thickening or the echogenicity of the gastric wall among gastric adenocarcinoma and lymphoma but, in general, B-mode ultrasonography findings may be nonspecific to distinguish different gastric tumors [64][50]. For that reason, contrast-enhanced ultrasonography is a promising modality that can help fill this gap, providing additional information to differentiate gastric neoplasms.
Malignant gastric tumors presented faster wash in compared to gastritis. B-mode ultrasound and CEUS were able to distinguish between malignant and benign gastric disorders, but the differentiation among several tumor histotypes still relies upon cytological or histopathological exams [62][48].
4.7. Liver and Biliary System
In the canine liver, a study of hepatocellular carcinoma evaluated with CEUS described some variation in the tumoral presentation (i.e., contrast enhancement) according to the level of cellular differentiation. The size of the tumor had little influence on the pattern of enhancement, either during wash in or wash out [67][51]. There can be three different enhancement phases distinguished in the liver. The arterial phase starts after contrast injection and provides information on the arterial blood supply of a given lesion. The portal venous phase presents diffuse and maximal contrast enhancement of the hepatic parenchyma, and the late phase marks the decrease of the contrast enhancement until the complete clearance of the contrast from circulation [68][52]. Different types of hepatic tumors can present variable contrast-enhancement patterns. For that reason, cytology and histopathology are important to confirm the diagnosis. Most sarcomas presented no enhancement during wash in. Metastasis presented hyper-enhancement during wash in, with hypo-enhancement during wash out [69][53]. This indicates a lower portal supply or lower blood volume of these metastatic lesions when compared to the liver parenchyma [70][54]. A well-differentiated hepatocellular carcinoma was characterized with homogeneous hyper-enhancement during the arterial phase and homogeneous wash out [67][51].4.8. Adrenal Glands
Contrast-enhanced ultrasound studies evaluated adrenal gland neoplasia and established parameters for the differentiation of adenoma, adenocarcinoma, and pheochromocytoma [75,76,77,78][55][56][57][58]. Malignant adrenal gland tumors presented heterogeneous contrast-enhancement patterns. Carcinoma and pheochromocytoma presented lower regional blood volumes when compared to adenoma. Adenocarcinoma presented tortuous feeding vessels during the arterial and venous phases [75][55]. The mean transit time (for contrast) was significantly lower for malignant neoplasia than for adenomas [75][55]. Pheochromocytoma presented a faster time to peak and a shorter mean transit time than adenoma and adenocarcinoma and bigger upslope and downslope than adenocarcinoma [76][56].4.9. Pancreas
Contrast-enhanced ultrasound was used to investigate canine pancreatic neoplasia. This imaging modality allowed the differentiation of adenocarcinomas, insulinomas, and benign nodules. Adenocarcinomas presented hypoechoic contrast enhancement [79,80][59][60] and hypoperfusion [80][60], whereas insulinomas were presented as solid lesions, with a homogeneous and hyperechoic contrast enhancement [80][60] and uniform hyperperfusion [80][60]. Comparatively, nodular hyperplasia was isoattenuating to the surrounding pancreatic parenchyma, whereas cystic formations presented no contrast enhancement [80][60].5. Conclusions
Elastography and contrast-enhanced ultrasonography provide important data on the differentiation of benign and malignant tumors in dogs and cats. These noninvasive imaging modalities are safe and can be easily performed on nonsedated animals, constituting interesting techniques for the investigation of neoplasia and metastasis in different tissues and organs. Their efficiency can be increased by the association with other imaging modalities such as B-mode or Doppler ultrasonography. Cytology and histopathology are the gold-standard methods to classify benign and malignant nodules and masses and determine the cellular type of a given neoplasm. However, they require invasive methods of tissue sampling, such as fine-needle aspiration or biopsy. In this way, elastography and CEUS, as well as other imaging modalities, can be used as screening tests, and can potentially represent an alternative to those invasive sampling methods.References
- Feliciano, M.A.R.; Maronezi, M.C.; Pavan, L.; Castanheira, T.L.; Simões, A.P.; Carvalho, C.; Canola, J.C.; Vicente, W.R. ARFI elastography as a complementary diagnostic method for mammary neoplasia in female dogs—Preliminary results. J. Small Anim. Pract. 2014, 55, 504–508.
- Appleby, R.B.; Vaden, S.L.; Monteith, G.; Seiler, G.S. Shear wave elastography evaluation of cats with chronic kidney disease. Vet. Radiol. Ultrasound 2023, 64, 330–336.
- Maronezi, M.C.; Feliciano, M.A.R.; Vicente, W.R.R. Elastografia e Ultrassonografia contrastada. In Ultrassonografia em Cães e Gatos, 1st ed.; Feliciano, M.A.R., Assis, A.R., Vicente, W.R.R., Eds.; MedVet: São Paulo, Brazil, 2019; pp. 33–56.
- Massimini, M.; Della Salda, L.; Di Francesco, L.; Contri, A. Strain and Shear-Wave Elastography and Their Relationship to Histopathological Features of Canine Mammary Nodular Lesions. Vet. Sci. 2022, 9, 506.
- Sporea, I.; Bota, S.; Jurchis, A.; Sirli, R.; Gradinaru-Tascau, O.; Popescu, A.; Ratiu, I.; Szilaski, M. Acoustic Radiation force impulse and supersonic shear imaging versus transient elastography for liver fibrosis assessment. Ultrasound Med. Biol. 2013, 39, 1933–1941.
- Boozari, B.; Potthoff, A.; Mederacke, I.; Hahn, A.; Reising, A.; Rifai, K.; Wedemeyer, H.; Bahr, M.; Kubicka, S.; Manns, M.; et al. Evaluation of sound speed for detection of liver fibrosis. Prospective comparison with transient elastography and histology. J. Ultrasound Med. 2010, 29, 1581–1588.
- Menzilcioglu, M.S.; Duymus, M.; Citil, S.; Avcu, S.; Gungor, G.; Sahin, T.; Boysan, S.N.; Altunoren, O.; Sarica, A. Strain wave elastography for evaluation of renal parenchyma in chronic kidney disease. Br. J. Radiol. 2015, 88, 20140714.
- Domoslawska, A.; Zdunczyk, S.; Jurczak, A.; Janowski, T. Elastography as a diagnostic tool in the prostate tumour detection in Labrador retriever. Andrologia 2018, 50, e13139.
- Cintra, C.A.; Feliciano, M.A.R.; Santos, V.J.C.; Maronezi, M.C.; Cruz, I.K.; Gasser, B.; Silva, P.; Crivellenti, L.Z.; Uscategui, R.A.R. Applicability of ARFI elastography on the evaluation of canine prostatic alterations detected by B-mode and Doppler ultrasonography. Arq. Bras. Med. Veterinária Zootec. 2020, 72, 2135–2140.
- Feliciano, M.A.R.; Maronezi, M.C.; Simões, A.P.R.; Uscategui, R.R.; Maciel, G.S.; Carvalho, C.F.; Canola, J.C.; Vicente, W.R.R. Acoustic radiation force impulse elastography of prostate and testes of healthy dogs: Preliminary results. J. Small Anim. Pract. 2015, 56, 320–324.
- Assawarachan, S.N.; Chuchalermporn, P.; Maneesaay, P.; Thengchaisri, N. Evaluation of hepatobiliary ultrasound scores in healthy dogs and dogs with liver diseases. Vet. World 2019, 12, 1266–1272.
- Tamura, M.; Ohta, H.; Shimbo, G.; Osuga, T.; Sasaki, N.; Morishita, K.; Kagawa, Y.; Takiguchi, M. Usefulness of noninvasive shear wave elastography for the assessment of hepatic fibrosis in dogs with hepatic disease. J. Vet. Intern. Med. 2019, 33, 2067–2074.
- Favril, S.; Stock, E.; Broeckx, B.J.G.; Devriendt, N.; de Rooster, H.; Vanderperren, K. Shear wave elastography of lymph nodes in dogs with head and neck cancer: A pilot study. Vet. Comp. Oncol. 2022, 20, 521–528.
- Silva, P.; Uscategui, R.A.R.; Maronezi, M.C.; Gasser, B.; Pavan, L.; Gatto, I.R.H.; Almeida, V.T.; Vicente, W.R.R.; Feliciano, M.A.R. Ultrasonography for lymph nodes metastasis identification in bitches with mammary neoplasms. Sci. Rep. 2018, 8, 17708.
- Azizi, G.; Keller, J.M.; Mayo, M.L.; Piper, K.; Puett, D.; Earp, K.M.; Malchoff, C.D. Shear Wave Elastography and Cervical Lymph Nodes: Predicting Malignancy. Ultrasound Med. Biol. 2016, 42, 1273–1281.
- Chen, B.B.; Li, J.; Xiao, W.W.; Zhao, C.; Lu, T.X.; Han, F. The value of shear wave elastography in predicting undiagnosed small cervical lymph node metastasis in nasopharyngeal carcinoma: A preliminary study. Eur. J. Radiol. 2018, 103, 19–24.
- Seiler, G.S.; Griffith, E. Comparisons between elastographic stiffness scores for benign versus malignant lymph nodes in dogs and cats. Vet. Radiol. Ultrasound 2018, 59, 79–88.
- Choi, M.; Yoon, J.; Choi, M. Semi-quantitative strain elastography may facilitate pre-surgical prediction of mandibular lymph nodes malignancy in dogs. J. Vet. Sci. 2019, 20, e62.
- Choi, M.; Yoon, J.; Choi, M. Contrast-enhanced ultrasound sonography combined with strain elastography to evaluate mandibular lymph nodes in clinically healthy dogs and those with head and neck tumors. Vet. J. 2020, 257, 105447.
- Belotta, A.F.; Gomes, M.C.; Rocha, N.S.; Melchert, A.; Giuffrida, R.; Silva, J.P.; Mamprim, M.J. Sonography and sonoelastography in the detection of malignancy in superficial lymph nodes of dogs. J. Vet. Intern. Med. 2019, 33, 1403–1413.
- Febo, E.; Del Signore, F.; Bernabo, N.; Paolini, A.; Simeoni, F.; De Bonis, A.; Rosto, M.; Canal, S.; Vignoli, M. Ultrasonography and Sonoelastography Characteristics of Benign vs. Malignant Mesenteric Lymph Nodes in Cats: An Update. Animals 2023, 13, 2664.
- Feliciano, M.A.R.; Uscategui, R.A.R.; Maronezi, M.C.; Simões, A.P.R.; Silva, P.; Gasser, B.; Pavan, L.; Carvalho, C.F.; Canola, J.C.; Vicente, W.R.R. Ultrasonography methods for predicting malignancy in canine mammary tumors. PLoS ONE 2017, 12, e0178143.
- Glinska-Suchocka, K.; Jankowski, M.; Kubiak, K.; Spuzak, J.; Dzimira, S.; Nicpon, J. Application of shear wave elastography in the diagnosis of mammary gland neoplasm in dogs. Pol. J. Vet. Sci. 2013, 16, 477–482.
- Feliciano, M.A.R.; Maronezi, M.C.; Brito, M.B.S.; Simões, A.P.R.; Maciel, G.S.; Castanheira, T.L.L.; Garrudo, E.; Uscategui, R.R.; Miceli, N.G.; Vicente, W.R.R. Doppler and Elastography as complementary diagnostic methods for mammary neoplasms in female cats. Arq. Bras. Med. Vet. Zootec. 2015, 67, 935–939.
- Collivignarelli, F.; Tamburro, R.; Aste, G.; Falerrno, I.; Del Signore, F.; Simeoni, F.; Patsikas, M.; Gianfelici, J.; Terragni, R.; Attorri, V.; et al. Lymphatic drainage mapping with indirect lymphography for canine mammary tumors. Animals 2021, 11, 1115.
- Holen, I.; Speirs, V.; Morrissey, B.; Blyth, K. In vivo models in breast cancer research: Progress, challenges and future directions. Dis. Models Mech. 2017, 10, 359–371.
- Liptak, J.M.; Boston, S.E. Nonselective lymph node dissection and sentinel lymph node mapping and biopsy. Vet. Clin. Anim. 2019, 49, 793–807.
- Sherwood, J.M.; Haynes, A.M.; Klocke, E.; Higginbotham, M.L.; Thomson, E.M.; Weng, H.Y.; Millard, H.A.T. Occurrence and clinicopathologic features of splenic neoplasia based on body weight: 325 dogs (2003–2013). J. Am. Anim. Hosp. Assoc. 2016, 52, 220–226.
- Maronezi, M.C.; Carneiro, R.K.; da Cruz, I.C.K.; de Oliveira, A.P.L.; De Nardi, A.B.; Pavan, L.; Del’Aguila-Silva, P.; Uscategui, R.A.R.; Feliciano, M.A.R. Accuracy of B-mode ultrasound and ARFI elastography in predicting malignancy of canine splenic lesions. Sci. Rep. 2022, 12, 4252.
- Barella, G.; Lodi, M.; Faverzani, S. Role of strain elastography in differentiating malignant hypoechoic splenic lesions in dogs: Preliminary results. Bulg. J. Vet. Med. 2017, 20, 255–263.
- Cruz, I.C.K.; Carneiro, R.K.; de Nardi, A.B.; Uscategui, R.A.R.; Bortoluzzi, E.M.; Feliciano, M.A.R. Malignancy prediction of cutaneous and subcutaneous neoplasms in canines using B-mode ultrasonography, Doppler, and ARFI elastography. BMC Vet. Res. 2022, 18, 10.
- Brizzi, G.; Crepaldi, P.; Roccabianca, P.; Morabito, S.; Zini, E.; Auriemma, E.; Zanna, G. Strain elastography for the assessment of skin nodules in dogs. Vet. Dermatol. 2021, 32, 272-e75.
- Longo, M.; Bavcar, S.; Handel, I.; Smith, S.; Liuti, T. Real-time elastosonography of lipomatous vs. malignant subcutaneous neoplasms in dogs: Preliminary results. Vet. Radiol. Ultrasound 2018, 59, 198–202.
- Huaijantug, S.; Yatmark, P.; Phophug, P.; Worapakdee, M.; Phutrakul, A.; Julapanthong, P.; Chuaychoo, K. Quantitative ultrasound elastography and serum ferritin level in dogs with liver tumors. J. Adv. Vet. Anim. Res. 2020, 7, 575–584.
- Brito, M.B.S.; Feliciano, M.A.R.; Coutinho, L.N.; Simões, A.P.R.; Maronezi, M.C.; Garcia, P.H.S.; Uscategui, R.R.; de Almeida, V.T.; Crivelaro, R.M.; Vicente, W.R.R. ARFI Elastography of healthy adult felines testes. Acta Sci. Vet. 2015, 43, 1303–1307.
- Patton, H.M.; Johnson, B.F.; Smorodinsky, E.; Sirlin, C.B. Imaging and Noninvasive Diagnosis of Liver Disease: Computerized Tomography, Ultrasound, Magnetic Resonance Imaging, and Emerging Techniques. In Zakim and Boyer’s Hepatology; Elsevier: Amsterdam, The Netherlands, 2012; pp. 216–254.
- Volta, A.; Manfredi, S.; Vignoli, M.; Russo, M.; England, G.C.; Rossi, F.; Bigliardi, E.; Di Ianni, F.; Parmigiani, E.; Bresciani, C.; et al. Use of contrast-enhanced ultrasonography in chronic pathologic canine testes. Reprod. Domest. Anim. 2014, 49, 202–209.
- Quartuccio, M.; Mangano, C.; Macri, F.; Rizzo, M.; Di Pietro, S.; Pugliese, M.; Mazzullo, G.; Cristarella, S.; De Majo, M. Contrast-enhanced ultrasound evaluation of testicular interstitial cell tumors in conscious non-sedated dogs. Vet. Med. 2018, 63, 125–130.
- Hillaert, A.; Stock, E.; Duchateau, L.; de Rooster, H.; Devriendt, N.; Vanderperren, K. B-Mode and Contrast-Enhanced Ultrasonography Aspects of Benign and Malignant Superficial Neoplasms in Dogs: A Preliminary Study. Animals 2022, 12, 2765.
- Orlandi, R.; Vallesi, E.; Boiti, C.; Polisca, A.; Bargellini, P.; Troisi, A. Characterization of Testicular Tumor Lesions in Dogs by Different Ultrasound Techniques. Animals 2022, 12, 210.
- Sinagra, L.; Orlandi, R.; Caspanello, T.; Troisi, A.; Iannelli, N.M.; Vallesi, E.; Pettina, G.; Bargellini, P.; de Majo, M.; Boiti, C.; et al. Contrast-Enhanced Ultrasonography (CEUS) in Imaging of the Reproductive System in Dogs: A Literature Review. Animals 2023, 13, 1615.
- Vanderperren, K.; Saunders, J.H.; Van der Vekens, E.; Wydooghe, E.; de Rooster, H.; Duchateau, L.; Stock, E. B-mode and contrast-enhanced ultrasonography of the mammary gland during the estrous cycle of dogs. Anim. Reprod. Sci. 2018, 199, 15–23.
- Choi, S.Y.; Jeong, W.C.; Lee, Y.W.; Choi, H.J. Contrast enhanced ultrasonography of kidney in conscious and anesthetized beagle dogs. J. Vet. Med. Sci. 2016, 78, 239–244.
- Prakash, A.; Tan, G.J.S.; Wansaicheong, G.K.L. Contrast enhanced ultrasound of kidneys. Pictorial essay. Med. Ultrason. 2011, 13, 150–156.
- Haers, H.; Vignoli, M.; Paes, G.; Rossi, F.; Taeymans, O.; Daminet, S.; Saunders, J.H. Contrast harmonic ultrasonographic appearance of focal space-occupying renal lesions. Vet. Radiol. Ultrasound 2010, 51, 516–522.
- Salwei, R.M.; O’Brien, R.T.; Matheson, J.S. Characterization of lymphomatous lymph nodes in dogs using contrast harmonic and Power Doppler ultrasound. Vet. Radiol. Ultrasound 2005, 46, 411–416.
- Rossi, F.; Leone, V.F.; Vignoli, M.; Laddaga, E.; Terragni, R. Use of contrast-enhanced ultrasound for characterization of focal splenic lesions. Vet. Radiol. Ultrasound 2008, 49, 154–164.
- Simeoni, F.; Del Signore, F.; Aste, G.; Bargellini, P.; Rubini, G.; Terragni, R.; Tamburro, R.; Falerno, I.; de Pasquale, F.; Russo, M.; et al. B-Mode and Contrast Enhanced Ultrasonography Features of Gastric Inflammatory and Neoplastic Diseases in Dogs. Animals 2021, 11, 670.
- Seiler, G.; Maï, W. The Stomach. In Bsava Manual of Canine and Feline Abdominal Imaging; O’Brien, R., Barr, F., Eds.; British Small Animal Veterinary Association: Gloucester, UK, 2009; pp. 87–109.
- Simeoni, F.; Del Signore, F.; Terragni, R.; Tamburro, R.; Aste, G.; Vignoli, M. Diagnostic imaging of Gastrointestinal Tumors in Dogs and Cats: A Review. Am. J. Anim. Vet. Sci. 2020, 15, 89–101.
- Banzato, T.; Rubini, G.; Orlandi, R.; Bargellini, P.; Bonsembiante, F.; Zotti, A. Contrast-enhanced ultrasound features of hepatocellular carcinoma in dogs. Vet. Rec. 2020, 186, 187.
- Chammas, M.C.; Bordini, A.L. Contrast-enhanced ultrasonography for the evaluation of malignant focal liver lesions. Ultrasonography 2022, 41, 4–24.
- Burti, S.; Zotti, A.; Rubini, G.; Orlandi, R.; Bargellini, P.; Bonsembiante, F.; Banzato, T. Contrast-enhanced ultrasound features of malignant focal hepatic masses in dogs. Sci. Rep. 2020, 10, 6076.
- Cantisani, V.; Grazhdani, H.; Fioravanti, C.; Rosignuolo, M.; Calliada, F.; Messineo, D.; Bernieri, M.G.; Redler, A.; Catalano, C.; D’Ambrosio, F. Liver metastases: Contrast-enhanced ultrasound compared with computed tomography and magnetic resonance. World J. Gastroenterol. 2014, 20, 9998–10007.
- Pey, P.; Rossi, F.; Vignoli, M.; Duchateau, L.; Marescaux, L.; Saunders, J.H. Use of contrast-enhanced ultrasonography to characterize adrenal gland tumors in dogs. Am. J. Vet. Res. 2014, 75, 886–892.
- Nagumo, T.; Ishigaki, K.; Yoshida, O.; Iizuka, K.; Tamura, K.; Sakurai, N.; Terai, K.; Seki, M.; Edamura, K.; Asano, K. Utility of contrast-enhanced ultrasound in differential diagnosis of adrenal tumors in dogs. J. Vet. Med. Sci. 2020, 82, 1594–1601.
- Bargellini, P.; Orlandi, R.; Dentini, A.; Paloni, C.; Rubioni, G.; Fonti, P.; Diana, A.; Peterson, M.E.; Boiti, C. Use of contrast-enhanced ultrasound in the diagnosis of adrenal tumors in dogs. J. Am. Anim. Hosp. Assoc. 2016, 52, 132–143.
- Burti, S.; Zotti, A.; Rubini, G.; Orlandi, R.; Bargellini, P.; Bonsembiante, F.; Contiero, B.; Bendazzoli, M.; Banzato, T. Contrast-enhanced ultrasound features of adrenal lesions in dogs. Vet. Rec. 2023, 193, e2949.
- Burti, S.; Zotti, A.; Rubini, G.; Orlandi, R.; Bargellini, P.; Bonsembiante, F.; Contiero, B.; Banzato, T. Contrast-enhanced ultrasound features of focal pancreatic lesions in dogs. Vet. Rec. 2022, 191, e2080.
- Vanderperren, K.; Haers, H.; Van der Vekens, E.; Stock, E.; Paepe, D.; Daminet, S.; Saunders, J.H. Description of the use of contrast-enhanced ultrasonography in four dogs with pancreatic tumors. J. Small Anim. Pract. 2014, 55, 164–169.
More
