Dietary supplements are widely utilized by cancer patients as part of a complementary and integrative approach to their healthcare. However, a significant portion of patients refrain from discussing their supplement use with their physicians, often due to the perceived indifference or negativity of their healthcare providers. This communication gap exposes patients to unreliable information sources and potential risks associated with uninformed supplementation. As the healthcare landscape evolves, there is an increasing recognition of the pivotal role that physicians play in guiding patients’ healthcare decisions. A patient-centered perspective prioritizes the provision of evidence-based information tailored to the individual’s needs. It advocates for open discussions about potential risks and fosters shared decision making, respecting patient autonomy. Additionally, this approach involves offering alternative options, documenting patient preferences, and ensuring ongoing support while coordinating with the healthcare team.
- complementary medicine
- alternative medicine
- integrative medicine
- cancer care
- oncology
- nutritional supplements
1. Introduction
2. Motivations for Supplement Use
Understanding the motivations that drive patients to adopt dietary supplements (DSs) is pivotal, especially in the context of cancer care. These motivations provide valuable insights into why patients choose to integrate DSs into their journey with cancer. One of the primary motivations for using DSs among cancer patients is the management of treatment side effects [5,6,18,19,20,21,22,23,24][5][6][7][8][9][10][11][12][13]. These side effects encompass issues like nausea, fatigue, and digestive challenges often associated with treatments such as chemotherapy, radiation, and immunotherapy. Additionally, patients dealing with anxiety tend to rely more on DSs, seeking psychological support and a sense of empowerment to take charge of their healthcare decisions [20][9]. For many, the objective of DS use is to enhance their quality of life rather than aiming solely for a cure [5,6,18,19,20][5][6][7][8][9]. Furthermore, cancer patients frequently turn to DSs with the aim of boosting their immune systems [5,6,18,19,20][5][6][7][8][9]. A robust immune response is crucial, helping patients fend off infections, recover from treatments, and maintain their overall health. Many view DSs, particularly those rich in vitamins, minerals, and antioxidants, as allies in fortifying their immune defenses. Moreover, the fear of cancer recurrence is a prevalent concern among survivors [5,6,19,20][5][6][8][9]. To allay this anxiety, some individuals resort to DSs, believing in their anti-cancer properties, which they perceive as a protective shield against disease recurrence, and which offer a sense of security and control. The pursuit of control and empowerment stands as a significant driver of DS usage [5,6,19,20][5][6][8][9]. A cancer diagnosis can often leave patients feeling adrift in a sea of uncertainty. DSs serve as a means of active participation in healthcare decisions, providing patients with a sense of control and autonomy over their health. Improving the overall quality of life remains a central objective in using supplements [5,6,19,20][5][6][8][9]. Patients seek enhancements not only of their physical well-being, but also of their emotional and mental health. The holistic approach offered by supplement use, addressing the body, mind, and spirit, presents an attractive option for enhancing overall well-being. Cultural factors and deeply ingrained beliefs significantly influence DS use [22,23,24][11][12][13]. Cultural practices and traditions often encourage specific supplement usage for health and healing, which patients tend to respect and follow. Additionally, the allure of a natural and holistic approach to health often steers patients toward DSs. Faced with a life-altering diagnosis, patients view supplement use as an act of self-care, a form of self-advocacy that allows them to take charge of their health and play an active role in their treatment journey.3. Challenges in Physician–Patient Communication
Effective communication between physicians and patients with cancer regarding the use of DSs is a multifaceted process fraught with several challenges. These challenges can significantly affect the patient–provider relationship, the quality of care, and patient outcomes [19][8]. One fundamental challenge is the limited knowledge many physicians have about DSs. Medical education primarily focuses on conventional treatments and pharmaceuticals, leaving healthcare providers ill-equipped to discuss DSs with their patients. This knowledge gap results in a lack of guidance on this topic. A survey of US oncologists revealed that not even half discussed DS use with their patients [23][12]. On the patient side, there is often a reluctance to disclose supplement use to their physicians [21][10]. This reluctance can stem from a variety of factors, including a fear of judgment or disapproval, concerns about the physician’s lack of knowledge about supplements, a perception that conventional medicine providers do not want them to use alternative therapies, or sometimes even a fear that their physician will discontinue the conventional cancer therapies [18,19,20][7][8][9]. The absence of robust scientific evidence about DS use poses a substantial challenge. Supplements often lack the same level of rigorous research and safety data required of pharmaceutical drugs. The lack of clinical trials and comprehensive evidence make it difficult for physicians to provide evidence-based recommendations or to make informed decisions about supplement use. Both patients and physicians may feel uncertain about the effectiveness and safety of specific supplements [5,6,18,19,20][5][6][7][8][9]. Time constraints in clinical settings can be a practical challenge. Physicians often have limited time during patient appointments. Discussing DSs can be time consuming, involving a detailed review of the patient’s supplement regimen, potential interactions with prescribed medications, and patient education. These time constraints may hinder comprehensive discussions, leaving patients feeling unheard and misunderstood. In some healthcare systems, physicians may not receive reimbursement for discussing DSs or providing integrative care. This financial disincentive can lead to a lack of motivation to engage in in-depth conversations about supplements with patients, creating a disconnect between patient needs and healthcare provider priorities [19][8]. Differences in beliefs between patients and physicians can be a significant obstacle to effective communication. While patients may see supplements as a way to complement their conventional treatments and improve their well-being, physicians who do not share this perspective may struggle to effectively communicate or support these choices. Physicians must also manage patient expectations. Patients may have high hopes for DSs, anticipating significant benefits. Balancing these expectations with realistic, evidence-based information about the potential benefits and limitations of supplements can be a delicate task [5,6,19][5][6][8]. Trust is built on the belief that physicians have their patients’ best interests at heart, and when patients feel their choices are not acknowledged or respected, trust begins to wane [19][8].4. Developing an Approach to Address Cancer Patients’ Requests to Incorporate Dietary Supplements
A prominent comprehensive cancer center in the United States recently introduced another innovative care model that involves the use of a dedicated pharmacist to offer guidance to patients on the use of DSs [26][14]. In this program, integrative medicine providers who are engaged in counseling patients to address unmet symptom needs prescribe DSs when deemed appropriate, considering the clinical context, patient preferences, and available research evidence, using the clinical pharmacist as an additional professional who helps with providing this advice [26][14]. When a patient requests the addition of DSs to their cancer care, healthcare providers must dedicate sufficient time to address the patient’s needs thoroughly. To provide an informed response, providers should use reliable sources, such as About Herbs from Memorial Sloan Kettering Cancer Center [27][15] or the Natural Medicine Database [28][16], to evaluate the safety and efficacy of the supplement in question, the potential side effects, drug–herb–nutrient interactions, and product quality. The findings from such searches can be divided into three categories based on the risk and benefit value (Figure 1):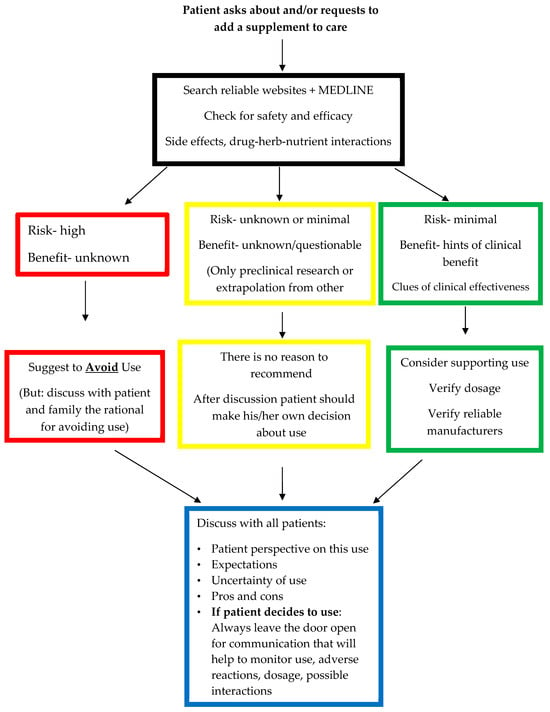
-
High risk and low or unknown benefit;
-
Questionable risk and low or unknown benefit;
-
Minimal risk and clinical clues regarding its benefit.
4.1. High Risk and Low or Unknown Benefit
If the research findings indicate that the use of a particular DS raises significant safety concerns, such as the potential for side effects and interactions, while the benefits remain unclear and are primarily based on speculation rather than clinical research, it is advisable to discourage such use. In such cases, healthcare providers should engage in a discussion that acknowledges the risks involved and also documents these concerns.4.2. Questionable Risk and Low or Unknown Benefit
When the research findings reveal no known safety or interaction concerns based on clinical research, yet there is no concrete evidence of clinical benefits, patients should not be dissuaded from using a supplement. It is important to respect their choice, even if their motivations for using a supplement are not based on scientific evidence. In such situations, an open and honest discussion with patients about their motivations, as well as a detailed discussion of the advantages and disadvantages of supplement use, should take place. Given the absence of major safety concerns, the approach should be to empower patients to make their own informed decisions regarding the use of a supplement.4.3. Minimal Risk with Clinical Clues Regarding the Benefit
A discussion about DS use should take place with all patients who seek advice about DSs during and after their cancer care. Patient perspectives and expectations should be explored, and the inherent uncertainty in DS use should be discussed, including the pros and cons, for all three categories. It is crucial to emphasize that even if patients choose to go against their advice, healthcare providers should maintain an open channel of communication, coupled with empathy and compassion. This approach will help to maintain communication and the monitoring of DS use, adverse reactions, and potential interactions, which is essential for intervention or treatment adjustments. Another important aspect of approaching DS use among cancer patients is informing the oncologist regarding the recommendations and patients’ decisions. This information will help the oncologist to understand the rationale behind supplement use and to help monitor for adverse effects or interactions, in case they need to add new medications to the treatment plan for the cancer. The physician’s role does not conclude with the initial discussion. Ongoing support and monitoring are vital as patients integrate DSs into their care plan. Collaboration with other healthcare team members, such as oncologists and nurses, is essential to promote patient safety and well-being, by ensuring that DSs do not interfere with the conventional treatments. Remaining informed and updated is a commitment that physicians must uphold. The ever-evolving landscape of DSs and their role in cancer care demands a continuous dedication to learning. Ongoing education and staying informed about the emerging evidence are essential to providing patients with the most current and evidence-based information. The ultimate goal is to empower patients to make well-informed and empowered choices. By encouraging and supporting patients in their quest to make informed decisions, physicians can ensure that patients are well equipped to navigate the intricate path of dietary supplement use in the context of cancer care. This suggested approach addresses cancer patients’ requests to integrate DSs into their care with a clear patient–doctor communication process relating to safety and efficacy, in a patient-centered manner.5. Recommending Dietary Supplements as Food
Discussing nutrition with patients affected by cancer is one of the main issues discussed in the integrative oncology setting [29][17]. Nutrition and DSs, in many situations, are commonly discussed in the same encounter. Many DSs are derived from food, and although some DSs are combinations of multiple ingredients, not all are. Therefore, advising the patient to eat the whole food that the supplement is derived from is another strategy that might help meet the patient’s expectations. One example is the use of mushroom supplements for cancer. The data support an association between high dietary mushroom consumption and a lower risk of cancer [30][18]. Mushrooms are anti-inflammatory and immune-enhancing, and are often used in Asian countries during cancer treatment.6. Conclusions
In summary, effective communication between physicians and cancer patients regarding dietary supplement (DS) use stands as a cornerstone for establishing trust and ensuring optimal care provision. Acknowledging and actively addressing the inherent challenges to this communication process are pivotal for fortifying the patient–provider relationship, elevating care standards and, ultimately, leading to improved patient outcomes. To meet these challenges and to achieve enhanced patient-centered care, healthcare providers must adopt a paradigm shift, viewing patients as informed participants in their healthcare decisions. Physicians should evolve into expert guides and consultants, valuing and respecting patient autonomy and empowerment. Central to this recommended approach is the emphasis on open discussion, transparency, and the utmost regard for patient autonomy. By adhering to such principles, healthcare providers can effectively navigate the intricacies of discussing dietary supplement use in the realm of cancer care, prioritizing the safety and overall well-being of the patient. Furthermore, in implementing this approach, it is imperative to integrate reliable sources of information, engage in risk stratification, and offer specific recommendations tailored to the individual patient’s needs. Subsequent monitoring ensures continued support and guidance, further reinforcing patient safety and optimal health outcomes.References
- The Council for Responsible Nutrition, Press Release, 5 October 2023: Three Quarters of Americans Take Dietary Supplements. Available online: https://www.crnusa.org/newsroom/three-quarters-americans-take-dietary-supplements-most-users-agree-they-are-essential (accessed on 17 October 2023).
- Dietary Supplement Health and Education Act of 1994, Pub. L. No. 103–417, 103rd Congress (25 October 1994). Available online: https://ods.od.nih.gov/About/DSHEA_Wording.aspx (accessed on 1 November 2023).
- Sandler, S.; Halabi, S.; Kaplan, E.; Baron, J.; Paskett, E.; Petrelli, N. Use of vitamins, minerals, and nutritional supplements by participants in a chemoprevention trial. Cancer 2001, 91, 1040–1045.
- Paltiel, O.; Avitzour, M.; Peretz, T.; Cherny, N.; Kaduri, L.; Pfeffer, R.M.; Wagner, N.; Soskolne, V. Determinants of the use of complementary therapies by patients with cancer. J. Clin. Oncol. 2001, 19, 2439–2444.
- Frenkel, M.; Abrams, D.I.; Ladas, E.J.; Deng, G.; Hardy, M.; Capodice, J.L.; Winegardner, M.F.; Gubili, J.K.; Yeung, K.S.; Kussmann, H.; et al. Integrating dietary supplements into cancer care. Integr. Cancer. Ther. 2013, 12, 369–384.
- Ge, J.; Fishman, J.; Vapiwala, N.; Lim, S.Q.; Desai, K.; Xie, S.X.; Mao, J.J. Patient-physician communication about complementary and alternative medicine in a radiation oncology setting. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, e1–e6.
- Tasaki, K.; Maskarinec, G.; Shumay, D.M.; Tatsumura, Y.; Kakai, H. Communication between physicians and cancer patients about complementary and alternative medicine: Exploring patients’ perspectives. Psychooncology 2002, 11, 212–220.
- Frenkel, M.; Cohen, L. Effective communication about the use of complementary and integrative medicine in cancer care. J. Altern. Complement. Med. 2014, 20, 12–18.
- Lee, H.R.; Song, Y.M.; Jeon, K.H.; Cho, I.Y. The association between the use of dietary supplement and psychological status of cancer survivors in Korea: A cross-sectional study. Korean J. Fam. Med. 2021, 42, 317–326.
- Sanford, N.N.; Sher, D.J.; Ahn, C.; Aizer, A.A.; Mahal, B.A. Prevalence and nondisclosure of complementary and alternative medicine use in patients with cancer and cancer survivors in the United States. JAMA Oncol. 2019, 5, 735–737.
- Ben-Arye, E.; Samuels, N.; Daher, M.; Turker, I.; Nimri, O.; Rassouli, M.; Silbermann, M. Integrating Complementary and Traditional Practices in Middle-Eastern Supportive Cancer Care. J Natl Cancer Inst Monogr. 2017, 2017, lgx016.
- Jiang, C.; Larbi, O.; Feyes, D.; Wang, G.M.; Momotaz, H.; Li, M.; Daunov, K.; Daly, B.; Mazanec, S.; Rodgers-Melnick, S.; et al. A survey of cancer patients, caregivers, and providers regarding familiarity, importance, and utilization of supportive and integrative oncology services. Support. Care Cancer 2021, 29, 5777–5785.
- John, G.M.; Hershman, D.L.; Falci, L.; Shi, Z.; Tsai, W.Y.; Greenlee, H. Complementary and alternative medicine use among US cancer survivors. J. Cancer Surviv. 2016, 10, 850–864.
- Hou, Y.N.; Chimonas, S.; Gubili, J.; Deng, G.; Mao, J.J. Integrating herbal medicine into oncology care delivery: Development, implementation, and evaluation of a novel program. Support. Care Cancer 2023, 31, 128.
- About Herbs Website, Memorial Sloane Kettering Cancer Center. Available online: https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/herbs/search (accessed on 1 November 2023).
- Nat Med Database. Available online: https://naturalmedicines.therapeuticresearch.com/ (accessed on 1 November 2023).
- Frenkel, M.; Sapire, K.J.; Lacey, J.; Zollman, C.; Sierpina, V.S. “What Should I Eat?”—Addressing Questions and Challenges Related to Nutrition in the Integrative Oncology Setting. Curr. Oncol. Rep. 2022, 24, 1557–1567.
- Ba, D.M.; Ssentongo, P.; Beelman, R.B.; Muscat, J.; Gao, X.; Richie, J.P. Higher Mushroom Consumption Is Associated with Lower Risk of Cancer: A Systematic Review and Meta-Analysis of Observational Studies. Adv. Nutr. Int. Rev. J. 2021, 12, 1691–1704.
