Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 3 by Lindsay Dong.
Urgent-start peritoneal dialysis (USPD) is defined as peritoneal dialysis initiated within 14 days of catheter insertion.
- urgent-start peritoneal dialysis
- peritoneal dialysis
- dialysis
- implementation
1. Introduction
Hemodialysis (HD) remains the most common form of renal replacement therapy in the United States, accounting for over 85% of incident dialysis in 2020 [1]. However, peritoneal dialysis (PD) is equally efficacious and allows patients to dialyze at home, leading to increased independence and quality of life for patients [2][3]. Furthermore, due to decreased healthcare costs and infrastructure, many countries are creating incentives to increase the percentage of patients on PD [4]. However, these incentives have not always been effective, and compared to locations such as Hong Kong, New Zealand, and Thailand, the United States lags far behind in PD utilization [5]. While dialysis ideally occurs after months to years of pre-dialysis care, up to 33% of patients receive little to no nephrology care before dialysis, and up to 60% of dialysis is initiated unplanned [6]. Peritoneal dialysis is a viable option for patients initiating dialysis in an unplanned manner, even prior to catheter site maturation. Typically, the catheter is placed and remains unused for at least 14 days. When initiated prior to 14 days after catheter implantation, it is termed urgent-start peritoneal dialysis (USPD). Furthermore, the majority of patients who begin dialysis while in the hospital continue the same modality as outpatients [7]. Given that a high percentage of patients initiate dialysis unplanned and many patients continue the same modality in the hospital, expanding the use of USPD may increase the use in the outpatient setting, especially among those who originally elected for PD. In an effort to maintain PD as an option for patients in the outpatient setting, USPD has been studied to determine its efficacy, especially in comparison to planned PD and urgent-start hemodialysis (USHD).
2. Clinical Considerations in Urgent-Start Peritoneal Dialysis
2.1. Patient Selection Criteria for USPD
Prior to initiating USPD, the patient must first go through a thorough evaluation. The initial evaluation can be performed by a nurse, social-worker, nurse care manager, nephrology fellow, or attending nephrologist using a standardized questionnaire [8]. There are few absolute contraindications to PD, especially if PD is to be started immediately in the inpatient setting. Broadly, PD requires a peritoneal cavity free of significant scarring or adhesions, a clean environment where exchanges can occur, and the mental/physical ability to perform PD [9]. Although some urgent-start PD may begin in the hospital, it is often initiated in outpatients, and therefore, social factors must also be considered. Due to the risk of infection, a clean environment in a stable home is required [9]. Given the increased patient responsibility in PD, including performing self-exchanges, the patient must have a high degree of motivation for PD and health literacy. When this is not met, or the patient has cognitive impairment, a caregiver or family member must meet these qualifications. Among the most important aspects of patient selection criteria is patient preference. While education in the inpatient setting may be time consuming and logistically difficult, it facilitates shared decision making and is vital to patient selection in USPD [10]. Most patients who initiate dialysis as inpatients will continue the same modality as outpatients [7]. Therefore, some patients who originally elected for outpatient PD but received USHD as inpatients may continue without their preferred modality. This process is described in Figure 1.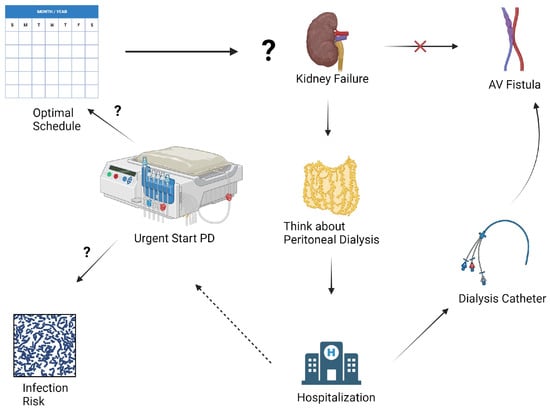
Figure 1. Rethinking Dialysis in the Urgent-Start Patient: Many patients elect for peritoneal dialysis in the outpatient setting but begin in an unplanned manner, often eventually receiving hemodialysis instead. Urgent-start peritoneal dialysis remains an understudied option to allow some of these patients to receive peritoneal dialysis in the outpatient setting. However, many clinical questions remain unanswered, including timing of initiation, terminology, and complications rates, such as infection and mechanical complications. Figure created with BioRender.com.
2.2. Timing of Initiation and Current Data Limitations
Conventional-start PD is defined as dialysis beginning 14 days or more after placement of a PD catheter. Given that a high percentage of patients require dialysis unplanned, the term “urgent start peritoneal dialysis” is applied to dialysis that begins prior to 14 days. However, recent literature has called for further dividing of USPD terminology, as some patients initiate PD within 24 h, while others begin after 13 days. Given the patients who require dialysis within 24 h are quite different from those who begin after 13 days, and there may be large differences in catheter site maturation, new definitions have been proposed. In 2018, Blake et al. proposed the terms “urgent start” for those who began within 72 h, and “early start” for those who began within 14 days [11]. Since publication, there has been an increase in literature that specifically separates these groups.2.3. Catheter Insertion Techniques
Multiple techniques are available to insert catheters for PD. These techniques can be performed both in inpatient and outpatient settings, and depending on the technique, can be implanted by different specialties. Techniques include open surgical, laparoscopic, interventional radiology-guided insertion, or percutaneously by nephrology. Among nonsurgical techniques, both fluoroscopy and ultrasound have demonstrated effectiveness [12]. Most commonly, a PD catheter is placed and secured using a double purse string technique.2.4. Peritoneal Dialysis Prescription and Modality Choices
When determining an initial PD prescription, there are various forms of PD a provider may choose. Given the concern for increased complications in USPD compared to conventional PD, investigators are interested in whether a certain prescription may decrease complications. Options include automated peritoneal dialysis (APD) and continuous ambulatory peritoneal dialysis (CAPD). Typically, patients receiving USPD will receive incremental PD (IPD) in which their prescription considers residual kidney function. One study of patients undergoing USPD compared APD and intermittent peritoneal dialysis (IPD) and showed that serum potassium and phosphorus were lower in the APD group, suggesting electrolyte clearance may be superior in APD [13].3. Outcomes and Efficacy of Urgent-Start Peritoneal Dialysis
3.1. Mechanical Complications and Technique Failure
Given most PD outcome data include patients who initiated PD after 14 days, clinical outcomes among those undergoing USPD are less well-defined. Mechanical complications such as catheter leaks and migrations are common in USPD. Rates of catheter leak at 30 days vary widely from 2.6% to 12% [14][15][16], and migration rates ranged from 2% to 12% at 30 days [14][15][16]. Overall catheter complications were also highly variable, with one study of 2059 patients reporting a 7.6% rate over a mean 36.5-month follow-up [17], compared to another study that showed a rate of 33.3% at 90 days [18]. Additionally, there is interest in determining if outcomes differ between conventional-start PD and USPD, and recent literature has investigated this relationship. The primary fear among patients who undergo USPD is increased mechanical complications, such as catheter dysfunction, and leakage, due to an immature site. Assuming the accuracy of this proposed mechanism, patients beginning with 72 h may have more mechanical complications than patients beginning with 14 days.3.2. Infectious Complications
Peritonitis is a common complication of PD [3]. There is interest in determining the approximate rate of peritonitis in USPD and whether it is different to conventional-start PD. Reported peritonitis rates at 30 days in USPD range from 0% to 8.6% [14][15][16][19]. Catheter site infection rates also vary widely from 0% to 12% [15][16][17]. One study of 310 diabetic patients found a 0.3% rate, while another smaller study of 26 patients found 12%, likely reflecting sample size differences. Additionally, one study found overall infectious complications to be 17% [20]. Although the crude rates were inconsistent, none of the studies demonstrated a statistically significant difference in peritonitis rates at 30 days when compared to conventional PD [14][15][16][21][22].3.3. Survival Rates and Patient Outcomes in USPD Compared to Other Modalities
Studies have compared outcomes between USPD and USHD to guide modality selection. USHD has a significantly higher 30-day bacteremia rate (13.4–21%) than USPD (3.0–3.1%) [23][24]. One such study reported a higher mortality rate due to infection, although the trend was not significant (p = 0.11) [23]. A Cochrane review also found more bacteremia with USHD versus USPD [25]. While the available evidence suggests USHD has a higher rate of bacteremia, overall complications may also be higher. Overall dialysis complications in USPD at 30 days were reported as 4.5–5.7% in USPD, compared to 10.7–24% in USHD [24][26][27].3.4. Impact of USPD on Healthcare Utilization
The use of peritoneal dialysis is increasing in developing countries, partially due to potentially lower costs and infrastructure needs compared to hemodialysis. However, the impact of complications on costs in urgent-start PD is unclear. One study analyzed costs in the first 90 days for USPD versus USHD. Mean costs were lower with USPD (USD 16,398) versus USHD (USD 19,352), primarily due to lower access-related costs (USD 2492 for USPD versus USD 5227 for USHD) [28]. The higher USHD costs reflect initial catheter placement and subsequent permanent access creation. Patients starting with USHD then transitioning to PD had similar costs to USHD alone (USD 19,400) [28].4. Barriers and Strategies to Optimize Urgent-Start Peritoneal Dialysis
4.1. Multidisciplinary Approach and Team Collaboration
Implementing USPD presents logistical challenges including coordination across multiple specialties and ensuring adequate staff familiarity with the modality. A summary of barriers is presented in Figure 2. A standardized evaluation helps identify appropriate candidates, considering social support, medical history, and functional status [8]. Extensive patient education is required as PD relies heavily on patient involvement, presenting workflow challenges when initiating PD urgently in the inpatient setting. Nurses, physicians, dieticians, psychologists, and administrators play a critical role in a successful PD program. Adequate nurse staffing ratios are crucial, since nurses complete many USPD tasks and may lack familiarity compared to conventional PD initiation [8]. Involving nurses in USPD protocol development can optimize success [8]. Post-initiation, vigilant nursing care may reduce complications through early issue recognition and intervention. Timely catheter placement also remains a barrier, as operators are often less comfortable with PD versus HD catheters [29], and catheters must be placed as soon as possible to initiate USPD. Operating room implantation, while facilitating adhesiolysis, presents logistical hurdles. Percutaneous insertion by interventional radiology or nephrology allows for urgent bedside placement in uncomplicated cases [30].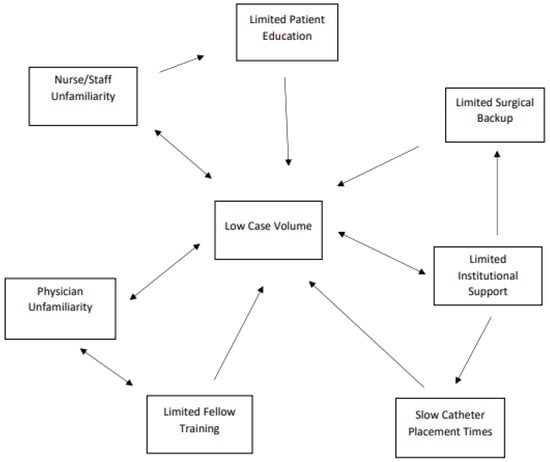
Figure 2. Summary of interconnected barriers to urgent-start peritoneal dialysis implementation.
4.2. Education and Training Programs for Healthcare Professionals
Hemodialysis is a far more prevalent modality than PD in most countries [1]. Due to a lack of exposure, many nephrologists and nephrology trainees do not feel comfortable prescribing PD. This concept is amplified with USPD. One study demonstrated that most fellows felt “moderately comfortable” with PD, and only 3% had ever initiated someone on USPD [31]. Furthermore, only 11% had ever observed a PD catheter insertion, and 3.8% felt competent placing a PD catheter [31]. In candidate patients, it is important to offer USPD as an option, and therefore, we must increase fellow comfortability. This may be through a variety of methods, including awareness, didactics, and hands-on practice. Even among comfortable providers, USPD use is limited by logistical barriers, including urgent placement of PD catheters [29]. While it has been previously stated that nephrology fellows have limited experience placing PD catheters, general surgery fellows feel similarly [29]. The most commonly cited reason for the inadequate training of PD catheters by general surgery trainees was inadequate referrals [29].4.3. Patient Education
Patient education is critical for informed dialysis modality selection and to ensure alignment with patient goals and values. Given that up to 60% of patients crash onto dialysis [6], many must make this life-altering decision in a short timeframe. To effectively inform patients of options, strong educational interventions are required.4.4. Clinical Pathways and Protocols for USPD Initiation and Follow-Up
Due to the significant collaboration and resulting challenges of initiating a USPD program, there is interest in the specific protocols used. Multiple centers have reported on their individual protocols and experiences, providing examples for other centers to potentially implement. Javaid et al. provide excellent examples of their initial experience and sustained success with USPD implementation [30][32]. This center performed a root cause analysis which identified three main barriers to USPD implementation: variation in PD patient selection criteria, unavailability of catheter placement, and lack of a coordinated program. The key to addressing these challenges was hiring a dedicated PD coordinator and ensuring staffing of nephrologists able to place PD catheters [30]. Adequate other staffing was identified, and a dedicated PD initiation clinic was created with nephrologists interested in PD and the PD coordinator to handle logistics. An outpatient center was formed to administer low-volume, supine PD for the first two weeks.4.5. Evidence Gaps and Areas for Future Research
As previously stated, a lack of clear terminology has plagued the field of USPD. Because quite different patient populations are all termed “urgent start peritoneal dialysis”, there is difficulty in comparing groups. The inability to adequately compare groups has led to low confidence data, hindering the advancement of USPD as a technique.5. Conclusions
In summary, USPD is a viable modality for patients who require initiation within 14 days. Given the potential patient and societal benefits of PD, increasing its use in the urgent setting may allow more patients to utilize the modality for maintenance. High rates of unplanned dialysis and continued use of the in-hospital form of dialysis in the outpatient setting suggest that increasing USPD may increase outpatient PD.References
- United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2022.
- Chuasuwan, A.; Pooripussarakul, S.; Thakkinstian, A.; Ingsathit, A.; Pattanaprateep, O. Comparisons of quality of life between patients underwent peritoneal dialysis and hemodialysis: A systematic review and meta-analysis. Health Qual. Life Outcomes 2020, 18, 191.
- Vogt, B.; Painter, D.F.; Saad Berreta, R.; Lokhande, A.; Shah, A.D. Hospitalization in maintenance peritoneal dialysis: A review. Hosp. Pract. 2023, 51, 18–28.
- Liu, F.X.; Gao, X.; Inglese, G.; Chuengsaman, P.; Pecoits-Filho, R.; Yu, A. A Global Overview of the Impact of Peritoneal Dialysis First or Favored Policies: An Opinion. Perit. Dial. Int. 2015, 35, 406–420.
- Briggs, V.; Davies, S.; Wilkie, M. International Variations in Peritoneal Dialysis Utilization and Implications for Practice. Am. J. Kidney Dis. 2019, 74, 101–110.
- Radhakrishnan, J.; Remuzzi, G.; Saran, R.; Williams, D.E.; Rios-Burrows, N.; Powe, N.; CDC-CKD Surveillance for the CDC-CKD Surveillance Team; Brück, K.; Wanner, C.; Stel, V.S.; et al. Taming the chronic kidney disease epidemic: A global view of surveillance efforts. Kidney Int. 2014, 86, 246–250.
- Rajora, N.; Shastri, S.; Pirwani, G.; Saxena, R. How To Build a Successful Urgent-Start Peritoneal Dialysis Program. Kidney360 2020, 1, 1165–1177.
- Ghaffari, A.; Kumar, V.; Guest, S. Infrastructure requirements for an urgent-start peritoneal dialysis program. Perit. Dial. Int. 2013, 33, 611–617.
- Teitelbaum, I. Peritoneal Dialysis. N. Engl. J. Med. 2021, 385, 1786–1795.
- Rosner, M.H. Peritoneal Dialysis Should Be Considered the First Option for Patients Requiring Urgent Start Dialysis: COMMENTARY. Kidney360 2023, 4, 141–142.
- Blake, P.G.; Jain, A.K. Urgent Start Peritoneal Dialysis: Defining What It Is and Why It Matters. Clin. J. Am. Soc. Nephrol. CJASN 2018, 13, 1278–1279.
- Abdel-Aal, A.K.; Dybbro, P.; Hathaway, P.; Guest, S.; Neuwirth, M.; Krishnamurthy, V. Best practices consensus protocol for peritoneal dialysis catheter placement by interventional radiologists. Perit. Dial. Int. 2014, 34, 481–493.
- Wang, C.; Fu, X.; Yang, Y.; Deng, J.; Lu, J.; Peng, Y.; Liu, Y.; Zhang, H.-Q.; Deng, H.-M.; Liu, H.; et al. A Comparison between Intermittent Peritoneal Dialysis and Automatic Peritoneal Dialysis on Urgent Peritoneal Dialysis. Am. J. Nephrol. 2017, 45, 540–548.
- Scalamogna, A.; Nardelli, L.; Cicero, E.; Castellano, G. Analysis of mechanical complications in urgent-start peritoneal dialysis. J. Nephrol. 2022, 35, 1489–1496.
- See, E.J.; Cho, Y.; Hawley, C.M.; Jaffrey, L.R.; Johnson, D.W. Early and Late Patient Outcomes in Urgent-Start Peritoneal Dialysis. Perit. Dial. Int. 2017, 37, 414–419.
- Hu, X.; Yang, L.; Sun, Z.; Zhang, X.; Zhu, X.; Zhou, W.; Wen, X.; Liu, S.; Cui, W. Break-in Period ≤ 24 Hours as an Option for Urgent-start Peritoneal Dialysis in Patients with Diabetes. Frontiers in endocrinology. 2022, 13, 93657.
- Ye, H.; Yang, X.; Yi, C.; Guo, Q.; Li, Y.; Yang, Q.; Chen, W.; Mao, H.; Li, J.; Qiu, Y.; et al. Urgent-start peritoneal dialysis for patients with end stage renal disease: A 10-year retrospective study. BMC Nephrol. 2019, 20, 238.
- Abrantes, A.R.M.; Gonçalves, H.; Ferrer, F.A.D.; Lobos, A.M.V. Urgent start peritoneal dialysis: Is there room for more? Nefrologia 2021, 41, 573–577.
- Pilatti, M.; Theodorovitz, V.C.; Hille, D.; Sevignani, G.; Ferreira, H.C.; Vieira, M.A.; Calice-Silva, V.; de França, P.H.C. Urgent vs. planned peritoneal dialysis initiation: Complications and outcomes in the first year of therapy. Braz. J. Nephrol. 2022, 44, 482–489.
- Bhalla, N.M.; Arora, N.; Darbinian, J.A.; Zheng, S. Urgent Start Peritoneal Dialysis: A Population-Based Cohort Study. Kidney Med. 2022, 4, 100414.
- Xie, J.; Wang, H.; Li, S.; Zuo, Y.; Wang, Y.; Zhang, Y.; Liang, T.; Li, J.; Wang, L.; Feng, Z.; et al. Low-Volume Tidal Peritoneal Dialysis Is a Preferable Mode in Patients Initiating Urgent-Start Automated Peritoneal Dialysis: A Randomized, Open-Label, Prospective Control Study. Ther. Apher. Dial. 2019, 23, 409–417.
- Wen, X.; Yang, L.; Sun, Z.; Zhang, X.; Zhu, X.; Zhou, W.; Hu, X.; Liu, S.; Luo, P.; Cui, W. Feasibility of a break-in period of less than 24 hours for urgent start peritoneal dialysis: A multicenter study. Ren. Fail. 2022, 44, 450–460.
- Koch, M.; Kohnle, M.; Trapp, R.; Haastert, B.; Rump, L.C.; Aker, S. Comparable outcome of acute unplanned peritoneal dialysis and haemodialysis. Nephrol. Dial. Transplant. 2012, 27, 375–380.
- Jin, H.; Fang, W.; Zhu, M.; Yu, Z.; Fang, Y.; Yan, H.; Zhang, M.; Wang, Q.; Che, X.; Xie, Y.; et al. Urgent-Start Peritoneal Dialysis and Hemodialysis in ESRD Patients: Complications and Outcomes. PLoS ONE 2016, 11, e0166181.
- Htay, H.; Johnson, D.W.; Craig, J.C.; Teixeira-Pinto, A.; Hawley, C.M.; Cho, Y. Urgent-start peritoneal dialysis versus haemodialysis for people with chronic kidney disease. Cochrane Database Syst. Rev. 2021, 2021, CD012899.
- Jin, H.; Ni, Z.; Mou, S.; Lu, R.; Fang, W.; Huang, J.; Hu, C.; Zhang, H.; Yan, H.; Li, Z.; et al. Feasibility of Urgent-Start Peritoneal Dialysis in Older Patients with End-Stage Renal Disease: A Single-Center Experience. Perit. Dial. Int. 2018, 38, 125–130.
- Zang, X.; Du, X.; Li, L.; Mei, C. Complications and outcomes of urgent-start peritoneal dialysis in elderly patients with end-stage renal disease in China: A retrospective cohort study. BMJ Open 2020, 10, e032849.
- Liu, F.X.; Ghaffari, A.; Dhatt, H.; Kumar, V.; Balsera, C.; Wallace, E.; Khairullah, Q.; Lesher, B.; Gao, X.; Henderson, H.; et al. Economic evaluation of urgent-start peritoneal dialysis versus urgent-start hemodialysis in the United States. Medicine 2014, 93, e293.
- Dean, D.; Cruz, D.N. We Use Permcaths Instead of Peritoneal Catheters for Acute Kidney Injury and Urgent-Start Dialysis. Semin. Dial. 2016, 29, 260–262.
- Javaid, M.M.; Khan, B.A.; Yeo, E.X.; Teo, B.W.; Subramanian, S. Sustained Increase in Peritoneal Dialysis Prevalence through a Structured PD Initiation Service. Perit. Dial. Int. 2018, 38, 374–376.
- Gupta, N.; Taber-Hight, E.B.; Miller, B.W. Perceptions of Home Dialysis Training and Experience Among US Nephrology Fellows. Am. J. Kidney Dis. 2021, 77, 713–718.e1.
- Javaid, M.M.; Lee, E.; Khan, B.A.; Subramanian, S. Description of an Urgent-Start Peritoneal Dialysis Program in Singapore. Perit. Dial. Int. 2017, 37, 500–502.
More
