You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 3 by Mona Zou and Version 2 by Mona Zou.
Peripheral arterial disease (PAD) is the third leading cause of atherosclerotic cardiovascular morbidity worldwide, with high prevalence and associated complications, and is often overlooked and undertreated. Research has shown that there is a profound lack of PAD-related knowledge and awareness; additionally, information sources are not often reliable and accessible.
- awareness
- patient education as topic
- knowledge
- peripheral artery disease
1. Introduction
Peripheral arterial disease (PAD)—a chronic arterial occlusive disease of the lower extremities—is a powerful predictor for all-cause, cardiovascular, and cerebrovascular morbidity and mortality, especially in older adults [1][2][3]. It is the third leading cause of atherosclerotic cardiovascular morbidity worldwide, affecting approximately 202 million people [1]. Despite the high prevalence and associated complications, PAD is often overlooked and undertreated [4]. Research has shown there is a profound lack of PAD-related knowledge and awareness in the general population [5][6][7], as well as healthcare providers [8][9][10] and those diagnosed with this condition [11]. Additionally, information sources for PAD are often not reliable and accessible [12][13].
Patient education is essential in the care of those living with cardiovascular diseases (CVD) [14][15], including PAD [3][16]. Patients require information about responding to symptoms, risk factors, and how to self-manage their disease to reduce this excess risk [14]. Indeed, patient education leads to not only increased knowledge but increased physical activity, improved nutrition, tobacco cessation, and medication adherence, as well as reductions in anxiety and depressive symptoms [14][15]. Delays in the presentation and appropriate management of the condition may lead to complications such as ischaemia, amputation, and death [4]. Research shows that educating and supporting patients with CVD leads to a better understanding of their central role in disease management, making informed decisions about their care, and engaging in heart-healthy behaviours [17]. Many strategies are used by healthcare providers to educate their patients, from discharge education [18] to structured programs following an event [19]. However, improvements in patients’ disease-related knowledge and awareness following educational interventions are not always achieved, which can compromise patients’ outcomes and the progression of their disease [20][21][22]. In this context, identifying patients’ needs and knowledge gaps is important to guide healthcare providers in supporting their patients’ learning journey.
2. Measurement of Disease-Related Knowledge and Awareness in PAD Patients
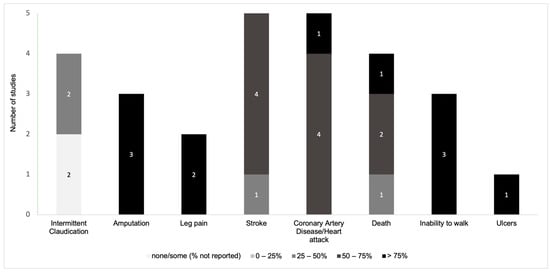
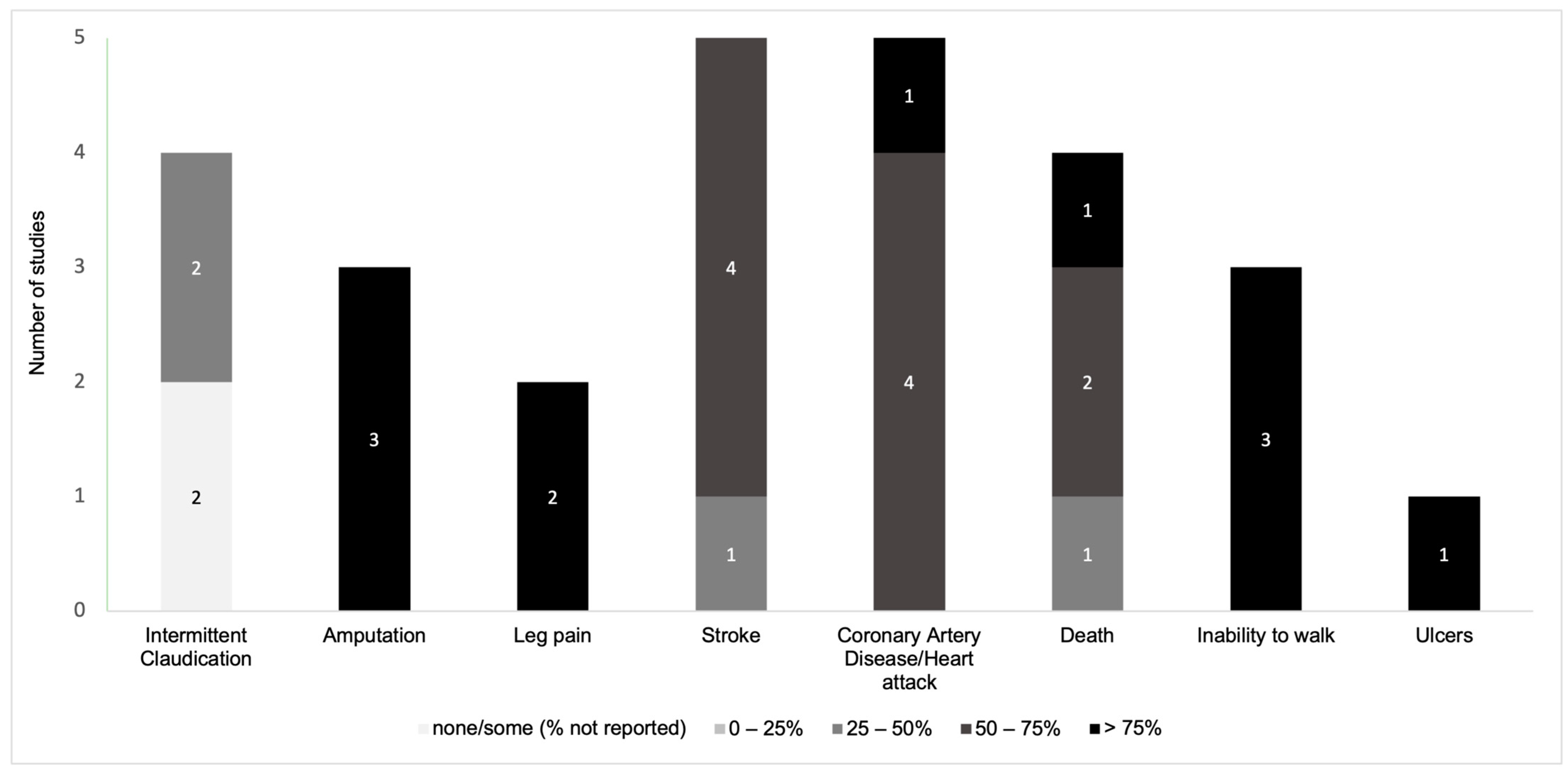
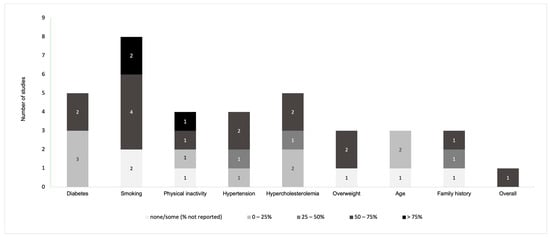
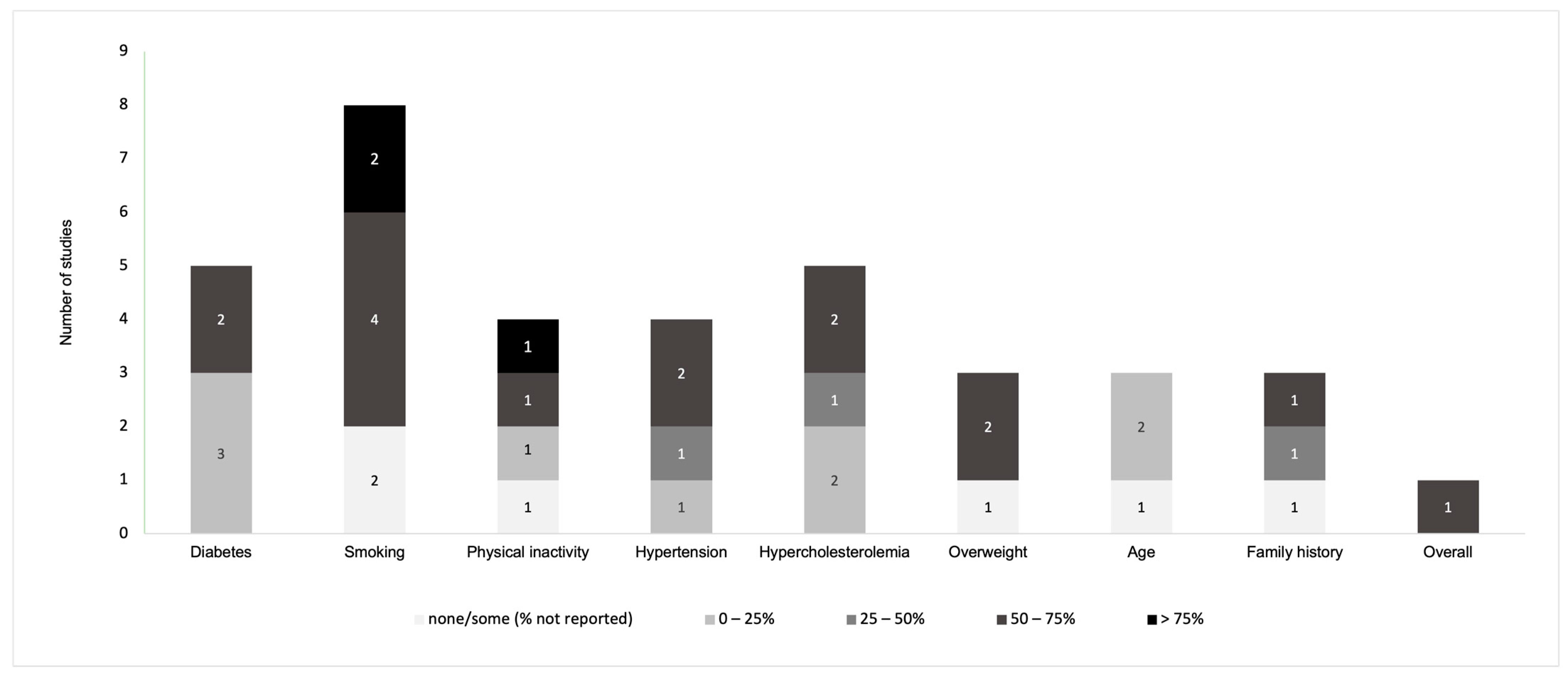
Overall, disease-related knowledge and awareness in PAD patients were measured with regard to signs/symptoms and complications in twelve instruments (Figure 1) [11][21][22][23][24][25][26][27][28][29][30][31], risk factors in nine instruments (Figure 2) [11][21][22][23][24][27][29][31][32], pathophysiology in eight instruments (Figure 3) [11][23][24][25][27][28][29][31], and management and pharmacological therapy in six instruments (Figure 4) [24][27][29][30][31][33]. One of the studies presented general knowledge without describing specific areas [34]. None of the identified instruments included questions from all these knowledge areas.Figure 1. Distribution of the knowledge and awareness about signs/symptoms of PAD evaluated in studies.
Figure 2. Distribution of the knowledge and awareness about risk factors of PAD evaluated in studies.
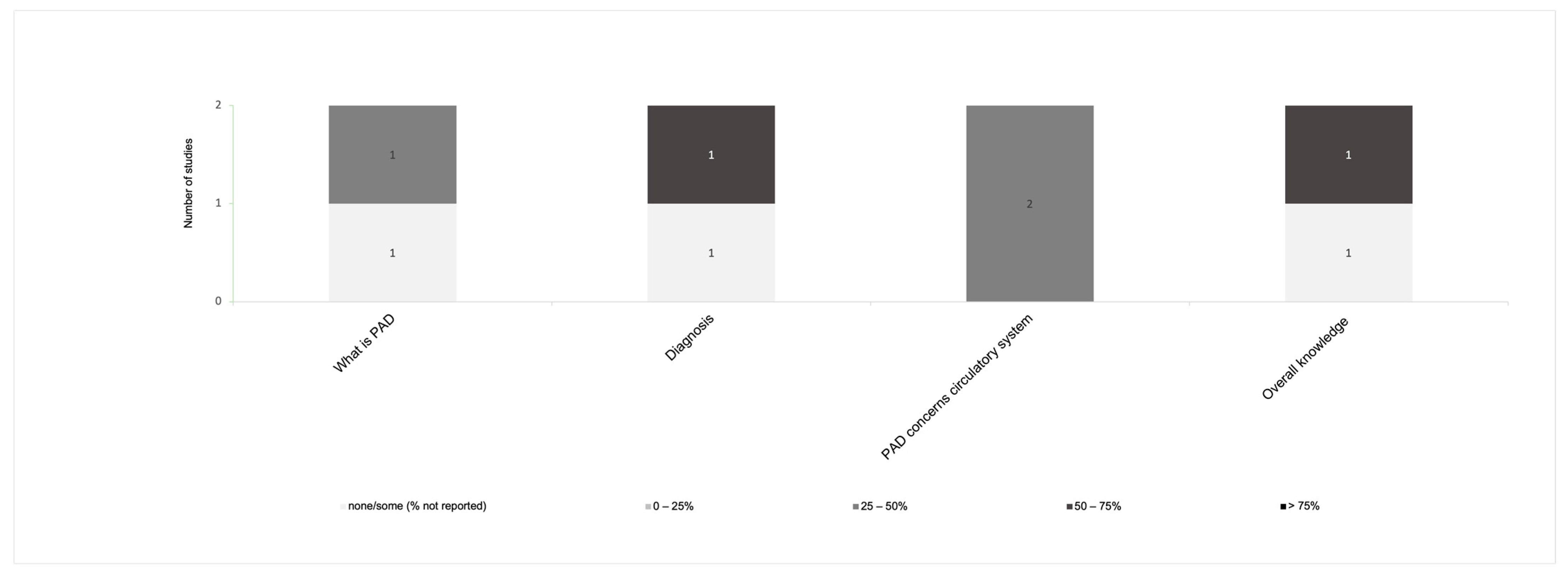
Figure 3. Distribution of the knowledge and awareness about the pathophysiology of PAD evaluated in studies.
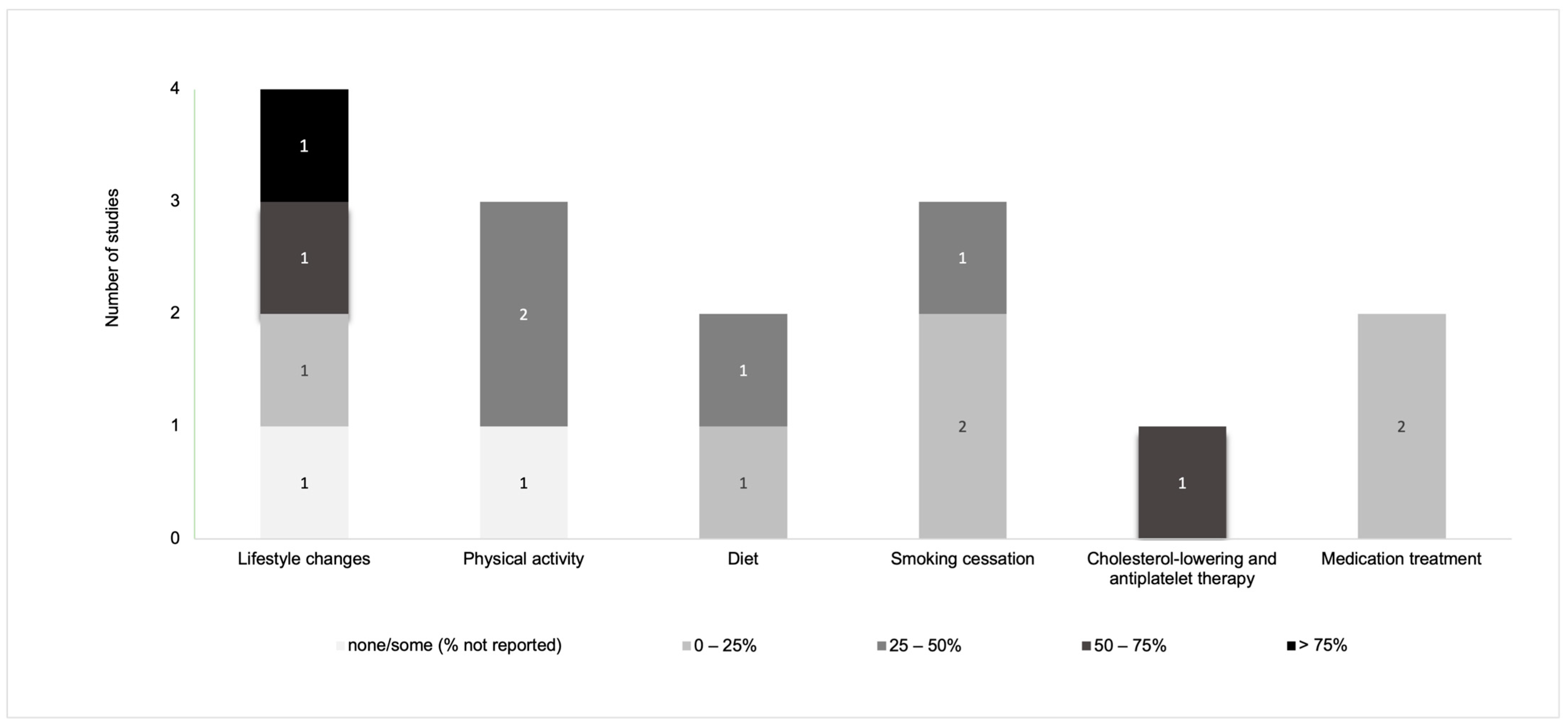
Figure 4. Distribution of the knowledge of, and awareness about, management and pharmacological therapy of PAD evaluated in studies.

Figure 5. Word cloud of most common terms included in the knowledge/awareness questions.
References
- Fowkes, F.G.R.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.A.; Williams, L.J.; Mensah, G.A.; et al. Comparison of Global Estimates of Prevalence and Risk Factors for Peripheral Artery Disease in 2000 and 2010: A Systematic Review and Analysis. Lancet 2013, 382, 1329–1340.
- National Clinical Guideline Centre. Lower Limb Peripheral Arterial Disease: Diagnosis and Management; NICE Clinical Guidelines; National Clinical Guideline Centre: London, UK, 2012.
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: Executive Summary. Vasc. Med. 2017, 22, NP1–NP43.
- Cronin, C.T.; McCartan, D.P.; McMonagle, M.; Cross, K.S.; Dowdall, J.F. Peripheral Artery Disease: A Marked Lack of Awareness in Ireland. Eur. J. Vasc. Endovasc. Surg. 2015, 49, 556–562.
- Hirsch, A.T.; Murphy, T.P.; Lovell, M.B.; Twillman, G.; Treat-Jacobson, D.; Harwood, E.M.; Mohler, E.R.; Creager, M.A.; Hobson, R.W.; Robertson, R.M.; et al. Gaps in Public Knowledge of Peripheral Arterial Disease: The First National PAD Public Awareness Survey. Circulation 2007, 116, 2086–2094.
- Lovell, M.; Harris, K.; Forbes, T.; Twillman, G.; Abramson, B.; Criqui, M.H.; Schroeder, P.; Mohler, E.R.; Hirsch, A.T. Peripheral Arterial Disease: Lack of Awareness in Canada. Can. J. Cardiol. 2009, 25, 39–45.
- Weragoda, J.; Weerasinghe, M.C.; Seneviratne, R.; Wijeyaratne, S.M. Gaps in Awareness of Peripheral Arterial Disease in Sri Lanka: A Cross Sectional Study. BMC Public Health 2016, 6, 1073.
- Bridgwood, B.M.; Nickinson, A.T.O.; Houghton, J.S.M.; Pepper, C.J.; Sayers, R.D. Knowledge of Peripheral Artery Disease: What Do the Public, Healthcare Practitioners, and Trainees Know? Vasc. Med. 2020, 25, 263–273.
- Schwarcz, A.I.; Quijano, A.; Olin, J.W.; Ostfeld, R.J. Internal Medicine Interns Have a Poor Knowledge of Peripheral Artery Disease. Angiology 2012, 63, 597–602.
- Correa-Vázquez, E.J.; de Jesús-Sosa, M.A.; Reyes-Claudio, K.M.; Chévere-Rivera, K. Cardiologist’s Knowledge of the Physiotherapy and the Challenges of Referring Patients with Peripheral Arterial Disease in Puerto Rico. Fisioterapia 2019, 41, 65–72.
- Byskosh, N.; Pamulapati, V.; Xu, S.; Vavra, A.K.; Hoel, A.W.; Tian, L.; McDermott, M.M.; Butt, Z.; Ho, K.J. Identifying Gaps in Disease Knowledge among Patients with Peripheral Artery Disease. J. Vasc. Surg. 2022, 75, 1358–1368.
- AlHamzah, M.; Eikelboom, R.; Hussain, M.A.; Syed, M.H.; Salata, K.; Wheatcroft, M.; Verma, S.; Al-Omran, M. Knowledge Gap of Peripheral Artery Disease Starts in Medical School. J. Vasc. Surg. 2019, 70, 241–245.
- AlHamzah, M.; Eikelboom, R.; Syed, M.; Salata, K.; Hussain, M.A.; Al-Omran, M. Physicians’ Peripheral Arterial Disease Knowledge Gap Starts in Medical School. J. Vasc. Surg. 2017, 63, e84.
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89.
- Balady, G.J.; Williams, M.A.; Ades, P.A.; Bittner, V.; Comoss, P.; Foody, J.M.; Franklin, B.; Sanderson, B.; Southard, D. Core Components of Cardiac Rehabilitation/Secondary Prevention Programs: 2007 Update: A Scientific Statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils O. Circulation 2007, 115, 2675–2682.
- Abramson, B.L.; Al-Omran, M.; Anand, S.S.; Albalawi, Z.; Coutinho, T.; de Mestral, C.; Dubois, L.; Gill, H.L.; Greco, E.; Guzman, R.; et al. Canadian Cardiovascular Society 2022 Guidelines for Peripheral Arterial Disease. Can. J. Cardiol. 2022, 38, 560–587.
- Bolt, L.J.J.; Jacobs, M.; Sigterman, T.A.; Krasznai, A.G.; Sikkink, C.; Schurink, G.W.H.; Bouwman, L.H. Assessment of Behavioral Determinants Influencing Success of Supervised Exercise Therapy in Patients with Intermittent Claudication: A Cross Sectional Survey. Physiol. Behav. 2020, 215, 112732.
- Veronovici, N.R.; Lasiuk, G.C.; Rempel, G.R.; Norris, C.M. Discharge Education to Promote Self-Management Following Cardiovascular Surgery: An Integrative Review. Eur. J. Cardiovasc. Nurs. 2014, 13, 22–31.
- Shi, W.; Ghisi, G.L.M.; Zhang, L.; Hyun, K.; Pakosh, M.; Gallagher, R. Systematic Review, Meta-Analysis and Meta-Regression to Determine the Effects of Patient Education on Health Behaviour Change in Adults Diagnosed with Coronary Heart Disease. J. Clin. Nurs. 2023, 32, 5300–5327.
- Krist, A.H.; Tong, S.T.; Aycock, R.A.; Longo, D.R. Engaging Patients in Decision-Making and Behavior Change to Promote Prevention. Stud. Health Technol. Inform. 2017, 240, 284–302.
- Lokin, J.L.C.; Hengeveld, P.J.; Conijn, A.P.; Nieuwkerk, P.T.; Koelemay, M.J.W. Disease Understanding in Patients with Intermittent Claudication: A Qualitative Study. J. Vasc. Nurs. 2015, 33, 112–118.
- Wann-Hansson, C.; Wennick, A. How Do Patients with Peripheral Arterial Disease Communicate Their Knowledge about Their Illness and Treatments? A Qualitative Descriptive Study. BMC Nurs. 2016, 15, 29.
- Keelan, S.; Foley, N.; Healy, D.; Kheirelseid, E.; McHugh, S.; Moneley, D.; Naughton, P. Poor Patient Awareness of Peripheral Arterial Disease, It Is Time to Optimize the Clinical Visit. Surgeon 2021, 20, 157–163.
- Willigendael, E.M.; Teijink, J.A.W.; Bartelink, M.L.; Boiten, J.; Moll, F.L.; Büller, H.R.; Prins, M.H. Peripheral Arterial Disease: Public and Patient Awareness in the Netherlands. Eur. J. Vasc. Endovasc. Surg. 2004, 27, 622–628.
- Udelnow, A.; Hecht, V.; Buschmann, I.; Wilbrandt, C.; Barth, U.; Meyer, F.; Halloul, Z. Disease Knowledge and Patient Education Are Key Players for a Better Quality of Life in Vascular Surgery Patients. Eur. Surg. 2020, 53, 75–83.
- Builyte, I.U.; Baltrunas, T.; Butkute, E.; Srinanthalogen, R.; Skrebunas, A.; Urbonavicius, S.; Rucinskas, K. Peripheral Artery Disease Patients Are Poorly Aware of Their Disease. Scand. Cardiovasc. J. 2019, 53, 373–378.
- Martínez, L.G.; Gutiérrez, R.F.; Gallego, A.G.; García, A.P.; Vega, M.S.; Calvo, A.Z. Diseño, Validación y Aplicación Clínica de Un Cuestionario de Conocimiento (ConocEAP) de Los Pacientes Con Enfermedad Arterial Periférica. Angiología 2017, 69, 4–11.
- Vasaroangrong, T.; Thosingha, O.; Riegel, B.; Ruangsetakit, C.; Viwatwongkasem, C. Factors Influencing Prehospital Delay Time among Patients with Peripheral Arterial Occlusive Disease. Eur. J. Cardiovasc. Nurs. 2016, 15, 285–293.
- Owens, M.; Mohan, H.; Moloney, M.A.; Roche-Nagle, G.; Baker, J.; Sheehan, S.; Mehigan, D.; Barry, M. Patient Knowledge of Peripheral Vascular Disease in an Outpatient Setting: An Achilles Heel? Ir. Med. J. 2013, 106, 116–118.
- McDermott, M.M.; Mandapat, A.L.; Moates, A.; Albay, M.; Chiou, E.; Celic, L.; Greenland, P. Knowledge and Attitudes Regarding Cardiovascular Disease Risk and Prevention in Patients with Coronary or Peripheral Arterial Disease. Arch. Intern. Med. 2003, 163, 2157–2162.
- Gorely, T.; Crank, H.; Humphreys, L.; Nawaz, S.; Tew, G.A. “Standing Still in the Street”: Experiences, Knowledge and Beliefs of Patients with Intermittent Claudication—A Qualitative Study. J. Vasc. Nurs. 2015, 33, 4–9.
- Coughlin, P.A.; Gulati, V.; Mavor, A.I.D.; Gough, M.J.; Homer-Vanniasinkam, S. Risk Factor Awareness in Patients with Peripheral Arterial Disease. J. Cardiovasc. Surg. 2007, 48, 735.
- Provance, J.B.; Spertus, J.A.; Decker, C. Abstract 15970: Examining Patients’ Knowledge with Regards to Peripheral Artery Disease Treatments and Outcomes: Insights from the PORTRAIT Registry. Circulation 2018, 138, A15970.
- El Jang, D.; Jang, Y.S.; Oh, E.G.; Ko, Y.G. Factors Associated with Health-Related Quality of Life in Patients with Peripheral Arterial Disease. Korean J. Adult Nurs. 2018, 30, 266–276.
More