During the COVID-19 pandemic, an increase in the incidence of overweight and obesity in children was observed. It appears that unhealthy food choices, an unbalanced diet, and a sedentary lifestyle, as well as experiencing stress related to the pandemic, may be contributing to this disturbing trend. Chronic stress is a significant factor contributing to eating disorders and obesity in youngsters, involving medical, molecular, and psychological elements. Individuals under chronic stress often focus on appearance and weight, leading to negative body image and disrupted relationships with food, resulting in unhealthy eating behaviors. Chronic stress also impacts hormonal balance, reducing the satiety hormone leptin and elevating the appetite-stimulating hormone ghrelin, fostering increased hunger and uncontrolled snacking. Two systems, the hypothalamic–pituitary–adrenal axis and the sympathetic system with the adrenal medulla, are activated in response to stress, causing impaired secretion of noradrenaline and cortisol. Stress-related obesity mechanisms encompass oxidative stress, neuroinflammation, insulin resistance, and neurohormonal and neurotransmission disorders. Stress induces insulin resistance, elevating obesity risk by disrupting blood sugar regulation and fat storage. Stress also affects the gut microbiome, potentially influencing chronic inflammation and metabolic processes linked to obesity.
- chronic stress
- COVID-19 pandemic
- overweight
- obesity
- children
- adolescents
- eating behaviors
1. Mental Health, Pandemic Environment, and Eating Disorders
| Psychological and Pedagogical Interventions Used in Eating Disorder Treatment | |||
|---|---|---|---|
| Anorexia Nervosa | Bulimia Nervosa | Binge Eating Disorder | References |
|
|
|
[64,65,66,67,68,69][41][42][43][44][45][46] |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|||
|
|||
|
|||
|
|||
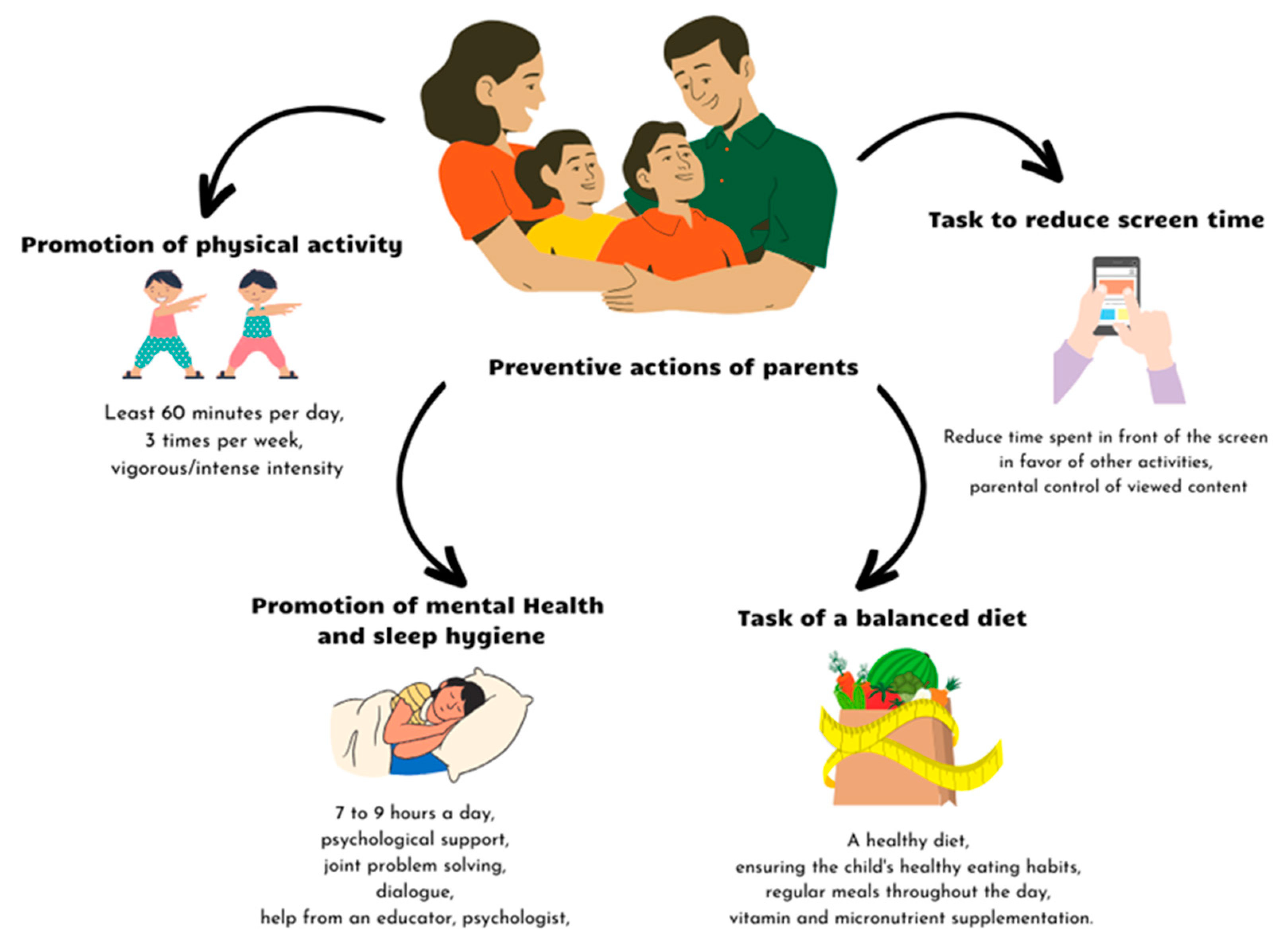
2. Prevention of Eating Disorders
References
- Branson, V.; Dry, M.J.; Palmer, E.; Turnbull, D. The Adolescent Distress-Eustress Scale: Development and Validation. Sage Open 2019, 9, 2158244019865802.
- Branson, V.; Turnbull, D.; Dry, M.J.; Palmer, E. How Do Young People Experience Stress? A Qualitative Examination of the Indicators of Distress and Eustress in Adolescence. Int. J. Stress. Manag. 2019, 26, 321–329.
- Branson, V.; Palmer, E.; Dry, M.J.; Turnbull, D. A Holistic Understanding of the Effect of Stress on Adolescent Well-Being: A Conditional Process Analysis. Stress. Health 2019, 35, 626–641.
- Qian, L.; McWeeny, R.; Shinkaruk, C.; Baxter, A.; Cao, B.; Greenshaw, A.; Silverstone, P.; Pazderka, H.; Wei, Y. Child and Youth Mental Health and Wellbeing before and after Returning to In-Person Learning in Secondary Schools in the Context of COVID-19. Front. Public. Health 2023, 11, 1212297.
- Dalton, L.; Rapa, E.; Stein, A. Protecting the Psychological Health of Children through Effective Communication about COVID-19. Lancet Child. Adolesc. Health 2020, 4, 346–347.
- Liu, J.J.; Bao, Y.; Huang, X.; Shi, J.; Lu, L. Mental Health Considerations for Children Quarantined Because of COVID-19. Lancet Child. Adolesc. Health 2020, 4, 347–349.
- Imran, N.; Aamer, I.; Sharif, M.I.; Bodla, Z.H.; Naveed, S. Psychological Burden of Quarantine in Children and Adolescents: A Rapid Systematic Review and Proposed Solutions. Pak. J. Med. Sci. 2020, 36, 1106–1116.
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2021, 50, 44.
- Otto, A.K.; Jary, J.M.; Sturza, J.; Miller, C.A.; Prohaska, N.; Bravender, T.; Van Huysse, J. Medical Admissions among Adolescents with Eating Disorders during the COVID-19 Pandemic. Pediatrics 2021, 148, e2021052201.
- Devoe, D.J.; Han, A.; Anderson, A.; Katzman, D.K.; Patten, S.B.; Soumbasis, A.; Flanagan, J.; Paslakis, G.; Vyver, E.; Marcoux, G.; et al. The Impact of the COVID-19 Pandemic on Eating Disorders: A Systematic Review. Int. J. Eat. Disord. 2023, 56, 5–25.
- Paiva, E.D.; da Silva, L.R.; Machado, M.E.D.; de Aguiar, R.C.B.; da Silva Garcia, K.R.; Acioly, P.G.M. Child Behavior during the Social Distancing in the COVID-19 Pandemic. Rev. Bras. Enferm. 2021, 74, e20200762.
- Jiao, W.Y.; Wang, L.N.; Liu, J.; Fang, S.F.; Jiao, F.Y.; Pettoello-Mantovani, M.; Somekh, E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020, 221, 264.
- Lavigne-Cerván, R.; Costa-López, B.; Juárez-Ruiz de Mier, R.; Real-Fernández, M.; Sánchez-Muñoz de León, M.; Navarro-Soria, I. Consequences of COVID-19 Confinement on Anxiety, Sleep and Executive Functions of Children and Adolescents in Spain. Front. Psychol. 2021, 12, 565516.
- Parent/Caregiver Guide to Helping Families Cope with the Coronavirus Disease 2019 | The National Child Traumatic Stress Network. Available online: https://www.nctsn.org/resources/parent-caregiver-guide-to-helping-families-cope-with-the-coronavirus-disease-2019 (accessed on 31 October 2023).
- Chawla, N.; Tom, A.; Sen, M.S.; Sagar, R. Psychological Impact of COVID-19 on Children and Adolescents: A Systematic Review. Indian J. Psychol. Med. 2021, 43, 294–299.
- Courtney, D.; Watson, P.; Battaglia, M.; Mulsant, B.H.; Szatmari, P. COVID-19 Impacts on Child and Youth Anxiety and Depression: Challenges and Opportunities. Can. J. Psychiatry 2020, 65, 688–691.
- Grover, S.; Venkatesh Raju, V.; Sharma, A.; Shah, R.S. Depression in Children and Adolescents: A Review of Indian Studies. Indian J. Psychol. Med. 2019, 41, 216–227.
- Rice, F.; Riglin, L.; Lomax, T.; Souter, E.; Potter, R.; Smith, D.J.; Thapar, A.K.; Thapar, A. Adolescent and Adult Differences in Major Depression Symptom Profiles. J. Affect. Disord. 2019, 243, 175–181.
- Lindberg, L.; Hagman, E.; Danielsson, P.; Marcus, C.; Persson, M. Anxiety and Depression in Children and Adolescents with Obesity: A Nationwide Study in Sweden. BMC Med. 2020, 18, 1–9.
- Mahmood, L.; Flores-Barrantes, P.; Moreno, L.A.; Manios, Y.; Gonzalez-Gil, E.M. The Influence of Parental Dietary Behaviors and Practices on Children’s Eating Habits. Nutrients 2021, 13, 1138.
- Moitra, P.; Madan, J. Impact of Screen Time during COVID-19 on Eating Habits, Physical Activity, Sleep, and Depression Symptoms: A Cross-Sectional Study in Indian Adolescents. PLoS ONE 2022, 17, e0264951.
- Kamaleddine, A.N.; Antar, H.A.; Ali, B.T.A.; Hammoudi, S.F.; Lee, J.; Lee, T.; Bhang, S.Y.; Chung, S.; Salameh, P. Effect of Screen Time on Physical and Mental Health and Eating Habits During COVID-19 Lockdown in Lebanon. Psychiatry Investig. 2022, 19, 220.
- Hill, D.C.; Moss, R.H.; Sykes-Muskett, B.; Conner, M.; O’Connor, D.B. Stress and Eating Behaviors in Children and Adolescents: Systematic Review and Meta-Analysis. Appetite 2018, 123, 14–22.
- Teixeira, M.T.; Vitorino, R.S.; da Silva, J.H.; Raposo, L.M.; Aquino, L.A.D.; Ribas, S.A. Eating Habits of Children and Adolescents during the COVID-19 Pandemic: The Impact of Social Isolation. J. Human. Nutr. Diet. 2021, 34, 670–678.
- Yu, Z.; Muehleman, V. Eating Disorders and Metabolic Diseases. Int. J. Environ. Res. Public Health 2023, 20, 2446.
- Agostino, H.; Burstein, B.; Moubayed, D.; Taddeo, D.; Grady, R.; Vyver, E.; Dimitropoulos, G.; Dominic, A.; Coelho, J.S. Trends in the Incidence of New-Onset Anorexia Nervosa and Atypical Anorexia Nervosa Among Youth During the COVID-19 Pandemic in Canada. JAMA Netw. Open 2021, 4, 2137395.
- Giacomini, G.; Elhadidy, H.S.M.A.; Paladini, G.; Onorati, R.; Sciurpa, E.; Gianino, M.M.; Borraccino, A. Eating Disorders in Hospitalized School-Aged Children and Adolescents during the COVID-19 Pandemic: A Cross-Sectional Study of Discharge Records in Developmental Ages in Italy. Int. J. Environ. Res. Public Health 2022, 19, 12988.
- Mizumoto, Y.; Sasaki, Y.; Sunakawa, H.; Tanese, S.; Shinohara, R.; Kurokouchi, T.; Sugimoto, K.; Seto, M.; Ishida, M.; Itagaki, K.; et al. Current Situation and Clinical Burden of Pediatricians for Children with Eating Disorders during the COVID-19 Pandemic. Glob. Health Med. 2023, 5, 122.
- Asch, D.A.; Buresh, J.; Allison, K.C.; Islam, N.; Sheils, N.E.; Doshi, J.A.; Werner, R.M. Trends in US Patients Receiving Care for Eating Disorders and Other Common Behavioral Health Conditions Before and During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2134913.
- Stabouli, S.; Erdine, S.; Suurorg, L.; Jankauskienė, A.; Lurbe, E. Obesity and Eating Disorders in Children and Adolescents: The Bidirectional Link. Nutrients 2021, 13, 4321.
- Breton, E.; Fotso Soh, J.; Booij, L. Immunoinflammatory processes: Overlapping mechanisms between obesity and eating disorders? Neurosci. Biobehav. Rev. 2022, 138, 104688.
- Villarejo, C.; Fernández-Aranda, F.; Jiménez-Murcia, S.; Peñas-Lledó, E.; Granero, R.; Penelo, E.; Tinahones, F.J.; Sancho, C.; Vilarrasa, N.; Montserrat-Gil de Bernabé, M.; et al. Lifetime obesity in patients with eating disorders: Increasing prevalence, clinical and personality correlates. Eur. Eat. Disord. Rev. 2012, 20, 250–254.
- Flament, M.F.; Henderson, K.; Buchholz, A.; Obeid, N.; Nguyen, H.N.; Birmingham, M.; Goldfield, G. Weight Status and DSM-5 Diagnoses of Eating Disorders in Adolescents From the Community. J. Am. Acad. Child. Adolesc. Psychiatry 2015, 54, 403–411.e2.
- Jebeile, H.; Lister, N.B.; Baur, L.A.; Garnett, S.P.; Paxton, S.J. Eating disorder risk in adolescents with obesity. Obes. Rev. 2021, 22, e13173.
- Vitagliano, J.A.; Jhe, G.; Milliren, C.E.; Lin, J.A.; Spigel, R.; Freizinger, M.; Woods, E.R.; Forman, S.F.; Richmond, T.K. COVID-19 and Eating Disorder and Mental Health Concerns in Patients with Eating Disorders. J. Eat. Disord. 2021, 9, 1–8.
- Spettigue, W.; Obeid, N.; Erbach, M.; Feder, S.; Finner, N.; Harrison, M.E.; Isserlin, L.; Robinson, A.; Norris, M.L. The Impact of COVID-19 on Adolescents with Eating Disorders: A Cohort Study. J. Eat. Disord. 2021, 9, 1–8.
- Graell, M.; Morón-Nozaleda, M.G.; Camarneiro, R.; Villaseñor, Á.; Yáñez, S.; Muñoz, R.; Martínez-Núñez, B.; Miguélez-Fernández, C.; Muñoz, M.; Faya, M. Children and Adolescents with Eating Disorders during COVID-19 Confinement: Difficulties and Future Challenges. Eur. Eat. Disord. Rev. 2020, 28, 864–870.
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The Impact of COVID-19 Epidemic on Eating Disorders: A Longitudinal Observation of Pre versus Post Psychopathological Features in a Sample of Patients with Eating Disorders and a Group of Healthy Controls. Int. J. Eat. Disord. 2020, 53, 1855–1862.
- Shum, M.; Moreno, C.; Kamody, R.; McCollum, S.; Shabanova, V.; Loyal, J. The Evolving Needs of Children Hospitalized for Eating Disorders During the COVID-19 Pandemic. Hosp. Pediatr. 2022, 12, 696–702.
- Toulany, A.; Kurdyak, P.; Guttmann, A.; Stukel, T.A.; Fu, L.; Strauss, R.; Fiksenbaum, L.; Saunders, N.R. Acute Care Visits for Eating Disorders Among Children and Adolescents After the Onset of the COVID-19 Pandemic. J. Adolesc. Health 2022, 70, 42–47.
- Davis, L.E.; Attia, E. Recent Advances in Therapies for Eating Disorders. F1000Research 2019, 8.
- Bohon, C. Binge Eating Disorder in Children and Adolescents. Child. Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 549.
- Hornberger, L.L.; Lane, M.A. Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics 2021, 147, e2020040279.
- Mairs, R.; Nicholls, D. Assessment and Treatment of Eating Disorders in Children and Adolescents. Arch. Dis. Child. 2016, 101, 1168–1175.
- Herpertz-Dahlmann, B.; Dahmen, B. Children in Need—Diagnostics, Epidemiology, Treatment and Outcome of Early Onset Anorexia Nervosa. Nutrients 2019, 11, 1932.
- Gorrell, S.; Le Grange, D. Update on Treatments for Adolescent Bulimia Nervosa. Child. Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 537.
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920.
- McCombie, C.; Austin, A.; Dalton, B.; Lawrence, V.; Schmidt, U. “Now It’s Just Old Habits and Misery”-Understanding the Impact of the COVID-19 Pandemic on People With Current or Life-Time Eating Disorders: A Qualitative Study. Front. Psychiatry 2020, 11, 589225.
- Maunder, K.; McNicholas, F. Exploring Carer Burden amongst Those Caring for a Child or Adolescent with an Eating Disorder during COVID-19. J. Eat. Disord. 2021, 9, 1–8.
- PiLaR Program—An Evaluation. HSE National Clinical Program of Eating Disorders National Clinical Programme for Eating Disorders. 2019. Available online: https://www.bodywhys.ie/wp-content/uploads/2019/02/PilarReport_web.pdf (accessed on 31 October 2023).
- Scapaticci, S.; Neri, C.R.; Marseglia, G.L.; Staiano, A.; Chiarelli, F.; Verduci, E. The Impact of the COVID-19 Pandemic on Lifestyle Behaviors in Children and Adolescents: An International Overview. Ital. J. Pediatr. 2022, 48, 1–17.
- Chua, J.Y.X.; Tam, W.; Shorey, S. Research Review: Effectiveness of Universal Eating Disorder Prevention Interventions in Improving Body Image among Children: A Systematic Review and Meta-Analysis. J. Child. Psychol. Psychiatry 2020, 61, 522–535.
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and Lockdown on Mental Health of Children and Adolescents: A Narrative Review with Recommendations. Psychiatry Res. 2020, 293, 113429.
- Parker, M.N.; Lavender, J.M.; Schvey, N.A.; Tanofsky-Kraff, M. Practical Considerations for Using the Eating Disorder Examination Interview with Adolescents. Adolesc. Health Med. Ther. 2023, 14, 63–85.
- O’Logbon, J.; Newlove-Delgado, T.; McManus, S.; Mathews, F.; Hill, S.; Sadler, K.; Ford, T. How Does the Increase in Eating Difficulties According to the Development and Well-Being Assessment Screening Items Relate to the Population Prevalence of Eating Disorders? An Analysis of the 2017 Mental Health in Children and Young People Survey. Int. J. Eat. Disord. 2022, 55, 1777–1787.
