You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Jessie Wu and Version 1 by Marijana Vičić.
Lichen planus is a chronic disease affecting the skin, appendages, and mucous membranes. A cutaneous lichen planus is a rare disease occurring in less than 1% of the general population, while oral illness is up to five times more prevalent; still, both forms equally impair the patient’s quality of life.
- antibodies
- dendritic cells
- etiology
- lichen planus
1. Introduction
Lichen planus (LP) is a chronic, immune-mediated, mucocutaneous inflammatory disorder [1]. The classic disease is defined by the so-called “rule six P”, which summarizes the skin lesions’ characteristics, i.e., planar, purple, polygonal, pruritic, papule and plaque [2]. Cutaneous LP is a rare dermatosis whose prevalence ranges from 0.22 to 1% and involves equally people of both sexes and different races. Instead, the more frequent oral disease occurs in 2 to 5% of the general population and is twice as common in women [3,4,5,6][3][4][5][6]. Although LP primarily includes the skin and oral mucosa, other mucous membranes and skin appendages, such as nails and hair, can also be damaged [5]. LP usually appears in middle-aged adults from 30 to 60 years of age and rarely affects other age groups [4]. Although the cutaneous disease has numerous clinical variants, its typical form is the classic LP, presenting with small, sharply demarcated, flattened and polygonally shaped erythematous-livid papules, which may coalesce as the disease progresses [4]. A prominent feature of LP is epidermal hypergranulosis, manifested as whitish reticulate structures or Wickham’s striae on the lesions’ surface [2]. A classic LP usually presents as localized form, with skin changes confined to the extremities, especially the wrists, ankles, dorsal surfaces of the hands and feet, and the lumbar region [2], or less commonly as a generalized condition, involving the entire body, including the oral and anogenital mucosa [4]. Despite the impressive clinical presentation, the latter has a good prognosis, marked by a spontaneous withdrawal within two years of onset [2]. Skin LP is generally followed by severe pruritus, whose intensity corresponds to the affected surface but lacks visible scratches or secondary infections [5].2. Etiology of LP
2. Etiology of Lichen Planus
The cause of LP has not been fully determined; however, genetic and environmental factors are thought to play a significant role in the onset of the disease (Figure 1).
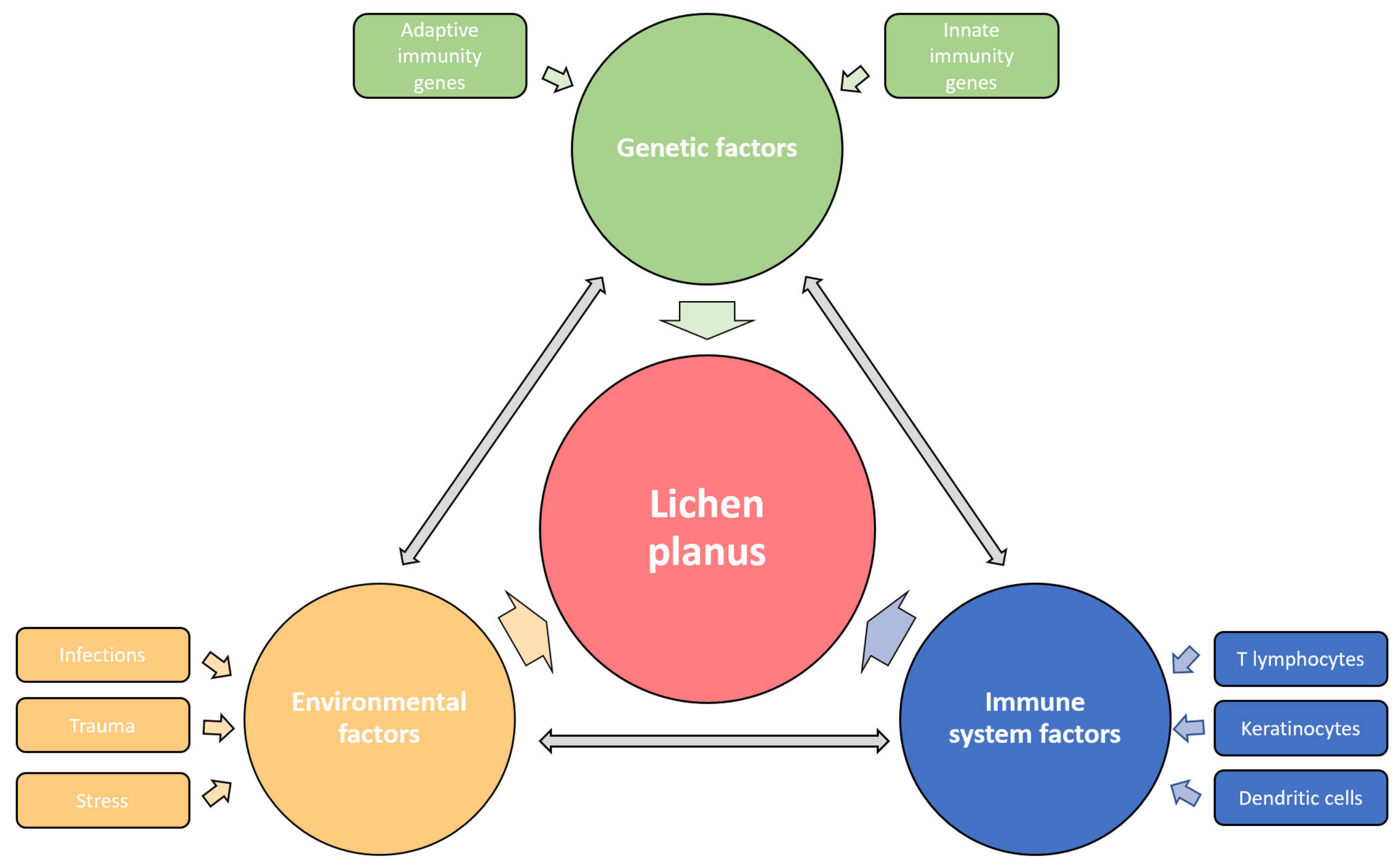
Figure 1. Etiological factors involved in the pathogenesis of LP. The disease affects the carrier of predisposing genes, in whom the various environmental factors trigger the immune response disorder resulting in specific LP phenotypes. The influences of genetic, environmental, and immune factors in LP development are dependent and mutually interconnected.
2.1. Genetic Factors
Genetic predisposition to disease was first suspected after noticing the LP presence in identical twins and 10% of the patients’ first relatives [2]. This observation confirmed the existence of a familial LP form, which constitutes up to 10% of all LP cases and is characterized by earlier onset, commoner relapses, treatment resistance, and oral mucosa involvement [24][7]. Still, genetic proneness has been observed in sporadic cases of LP. Furthermore, HLA-based susceptibility association studies identified a heterogeneous group of risk genotypes, some of which are primarily related to the familial form of the disease, such as HLA-A3, -Aw19, -B7, -B18 and -Cw8, the others such as HLA-DR1, -DRB1, -DQ1 and -Bw35 stand out in sporadic cases of cutaneous LP, while HLA-B8, -B51, -Bw57, -Bw61, are mostly expressed in oral OLPlichen planus (OLP) [2]. More detailed data on LP genetics were provided by a phenome-wide association study (PheWAS) revealing six single nucleotide polymorphisms (SNP), among which rs794275 was identified as the most significant, and HLA-DQB1 * 05:01 as the highly associated with LP [25][8]. Additionally, one genome-wide association study (GWAS) identified two more SNPs relevant for LP, i.e., rs884000 in the NRP2 and rs538399 in the IGFBP4 locus [26][9]. The conducted analyses discovered that the abovementioned polymorphisms principally affect genes with immune functions, such as Th1 response signaling molecules, i.e., TNF-α and IFN-γ, but also IL-4, IL-6, IL-10 and IL-12, IL-18, genes of oxidative stress, synthesis of thyroid hormones, prostaglandin E2, prothrombin, and NF-κB, which may impact the inflammatory mediators’ activity and cause disturbed signaling [1]. Genetic liability determines the reactivity of the patient’s skin and mucous membranes to other etiological factors.
2.2. Environmental Factors
Since the clinical course of the classic cutaneous LP is mainly marked by the acute beginning of one episode of the disease and its self-limiting nature, the microorganisms were often suspected as an LP causative agent. The association of LP with hepatitis C virus (HCV), which is up to thirteen times more common in LP patients, is best studied and verified by the results of several reports and meta-analyses conducted during the last decades [27,28,29,30,31][10][11][12][13][14]. A positive correlation between LP and HCV was observed among the populations of the Mediterranean, Germany, Japan, and the USA [32][15]. Although the exact role of HCV in LP development has still not been explained, viral components probably lead to host immune response dysregulation, as terminally differentiated and virus-specific CD8+ T lymphocytes have been found in the LP lesions [32,33][15][16]. Di Stasio et al. reported the improvement of OLP after direct-acting antiviral therapy, supporting the possible pathogenetic role of HCV infection in LP [33][16]. The increased prevalence and pathogenetic association of human papillomavirus (HPV) with OLP lesions have been proved [34][17], while the other possible causes include human herpesvirus 7 (HHV-7), found in infiltrating plasmacytoid dendritic cells in lesional skin biopsies [35[18][19][20],36,37], hepatitis B virus (HBV) [38[21][22],39], varicella-zoster virus (VZV) [40][23], and Epstein–Barr virus (EBV) [41][24]. In some cases, LP appeared or worsened following vaccination against hepatitis A and B [42,43[25][26][27],44], influenza [45][28], rabies [46][29], tetanus-diphtheria-pertussis [47][30] or SARS-CoV-2 in recent times [48,49,50][31][32][33]. Despite opposing views, Helicobacter pylori could contribute to LP etiopathogenesis, as it is associated with the altered function of salivary microbiome enhancing inflammation, while its eradication alleviates disease symptoms [51,52,53][34][35][36]. New data indicate that microbial infection could also play a role in OLP etiopathogenesis since it has been shown that a large number of bacteria and T lymphocytes were present in the affected tissue [54][37]. Novel fungi-based pathogenesis of OLP considers the role of Candida and Malassezia mycotypes in instigating the LP antigen expression and consequential Th17 lymphocytes’ reaction [55][38]. Furthermore, significant bacterial, fungal, and viral dysbiosis was detected in the saliva of these patients, with higher levels of Solobacterium, Fusobacterium, Porphyromonas, Prevotella, Candida, Aspergillus, Alternarium, tick-borne encephalitis virus, brochotrix bacteriophage virus and bacillus virus SPO1 and lower levels of Streptococci, Actinobacteria and Firmicutes compared to healthy controls [54,56][37][39]. Since the oral cavity is the initial part of the digestive system and forms part of the gut–skin axis, disturbances of the oral and salivary microbiome composition can directly trigger the patient’s immune system dysregulation, causing OLP [54,56][37][39].
However, in addition to microbial factors, it has been shown that OLP can be caused by contact allergens, primarily dental filling metals, such as mercury and gold [57,58[40][41][42],59], while its occurrence is associated with areca nut and betel quid chewing in the Far East as well [60,61][43][44]. Chemicals such as para-phenylenediamine, dimethyl fumarate and methacrylic acid esters can cause LP-like contact dermatitis [2,62][2][45]. Various drugs, especially those from the group of antihypertensives (beta-blockers and diuretics), antimalarials, antibiotics, antidiabetics, phosphodiesterase (PD)-1 inhibitors, and biologicals such as anti-TNF-α and dupilumab, can induce lichenoid reactions [63,64,65,66,67,68,69][46][47][48][49][50][51][52]. Lichen skin changes can occur due to radiation field exposure and radiotherapy [70][53]. Likewise, LP can be caused by mechanical injuries, such as surgical procedures or tattooing, which is confirmed by the appearance of the Köebner phenomenon in the linear form of the disease [71,72][54][55]. It has been proven that severe psychological stress can cause LP in hitherto healthy individuals, and anxiety and depression have the same effect on the onset or worsening of an existing illness [73,74,75][56][57][58].
References
- Boch, K.; Langan, E.A.; Kridin, K.; Zillikens, D.; Ludwig, R.J.; Bieber, K. Lichen Planus. Front. Med. 2021, 8, 737813.
- Tziotzios, C.; Lee, J.Y.W.; Brier, T.; Saito, R.; Hsu, C.K.; Bhargava, K.; Stefanato, C.M.; Fenton, D.A.; McGrath, J.A. Lichen planus and lichenoid dermatoses: Clinical overview and molecular basis. J. Am. Acad. Dermatol. 2018, 79, 789–804.
- Alrashdan, M.S.; Cirillo, N.; McCullough, M. Oral lichen planus: A literature review and update. Arch. Dermatol. Res. 2016, 308, 539–551.
- Solimani, F.; Forchhammer, S.; Schloegl, A.; Ghoreschi, K.; Meier, K. Lichen planus-a clinical guide. J. Dtsch. Dermatol. Ges. 2021, 19, 864–882.
- Ujiie, H.; Rosmarin, D.; Schon, M.P.; Stander, S.; Boch, K.; Metz, M.; Maurer, M.; Thaci, D.; Schmidt, E.; Cole, C.; et al. Unmet Medical Needs in Chronic, Non-communicable Inflammatory Skin Diseases. Front. Med. 2022, 9, 875492.
- Nosratzehi, T. Oral lichen planus: An overview of potential risk factors, biomarkers and treatments. Asian Pac. J. Cancer Prev. 2018, 19, 1161–1167.
- Brănişteanu, D.E.; Pintilie, A.; Andreş, L.E.; Dimitriu, A.; Oanţă, A.; Stoleriu, G.; Brănişteanu, D.C. Ethiopatogenic hypotheses in lichen planus.pdf. Rev. Med. Chir. Soc. Med. Nat. Iasi 2016, 120, 760–767.
- Liu, J.; Ye, Z.; Mayer, J.G.; Hoch, B.A.; Green, C.; Rolak, L.; Cold, C.; Khor, S.S.; Zheng, X.; Miyagawa, T.; et al. Phenome-wide association study maps new diseases to the human major histocompatibility complex region. J. Med. Genet. 2016, 53, 681–689.
- Nagao, Y.; Nishida, N.; Toyo-Oka, L.; Kawaguchi, A.; Amoroso, A.; Carrozzo, M.; Sata, M.; Mizokami, M.; Tokunaga, K.; Tanaka, Y. Genome-Wide Association Study Identifies Risk Variants for Lichen Planus in Patients with Hepatitis C Virus Infection. Clin. Gastroenterol. Hepatol. 2017, 15, 937–944.e5.
- Ma, S.H.; Tai, Y.H.; Dai, Y.X.; Chang, Y.T.; Chen, T.J.; Chen, M.H. Association between hepatitis C virus infection and subsequent chronic inflammatory skin disease. J. Dermatol. 2021, 48, 1884–1891.
- Alaizari, N.A.; Al-Maweri, S.A.; Al-Shamiri, H.M.; Tarakji, B.; Shugaa-Addin, B. Hepatitis C virus infections in oral lichen planus: A systematic review and meta-analysis. Aust. Dent. J. 2016, 61, 282–287.
- Petti, S.; Rabiei, M.; De Luca, M.; Scully, C. The magnitude of the association between hepatitis C virus infection and oral lichen planus: Meta-analysis and case control study. Odontology 2011, 99, 168–178.
- Lodi, G.; Pellicano, R.; Carrozzo, M. Hepatitis C virus infection and lichen planus: A systematic review with meta-analysis. Oral Dis. 2010, 16, 601–612.
- Pitak-Arnnop, P.; Subbalekha, K.; Sirintawat, N.; Tangmanee, C.; Auychai, P.; Muangchan, C.; Sukphopetch, P.; Meningaud, J.P.; Neff, A. Are oral lichen planus patients at high risk of hepatitis C? A case-control study. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e37–e42.
- Georgescu, S.R.; Tampa, M.; Mitran, M.I.; Mitran, C.I.; Sarbu, M.I.; Nicolae, I.; Matei, C.; Caruntu, C.; Neagu, M.; Popa, M.I. Potential pathogenic mechanisms involved in the association between lichen planus and hepatitis C virus infection. Exp. Ther. Med. 2019, 17, 1045–1051.
- Di Stasio, D.; Lucchese, A.; Romano, A.; Adinolfi, L.E.; Serpico, R.; Marrone, A. The clinical impact of direct-acting antiviral treatment on patients affected by hepatitis C virus-related oral lichen planus: A cohort study. Clin. Oral Investig. 2022, 26, 5409–5417.
- Della Vella, F.; Lauritano, D.; Pannone, G.; Del Prete, R.; Di Stasio, D.; Contaldo, M.; Petruzzi, M. Prevalence of HPV in patients affected by oral Lichen planus: A prospective study using two different chair-side sampling methods. J. Oral Pathol. Med. 2021, 50, 716–722.
- Nahidi, Y.; Tayyebi Meibodi, N.; Ghazvini, K.; Esmaily, H.; Esmaeelzadeh, M. Association of classic lichen planus with human herpesvirus-7 infection. Int. J. Dermatol. 2017, 56, 49–53.
- De Vries, H.J.; van Marle, J.; Teunissen, M.B.; Picavet, D.; Zorgdrager, F.; Bos, J.D.; Weel, J.; Cornelissen, M. Lichen planus is associated with human herpesvirus type 7 replication and infiltration of plasmacytoid dendritic cells. Br. J. Dermatol. 2006, 154, 361–364.
- De Vries, H.J.; Teunissen, M.B.; Zorgdrager, F.; Picavet, D.; Cornelissen, M. Lichen planus remission is associated with a decrease of human herpes virus type 7 protein expression in plasmacytoid dendritic cells. Arch. Dermatol. Res. 2007, 299, 213–219.
- Wang, J.H.; Hung, S.J. Lichen planus associated with hepatitis B, hepatitis C, and liver cirrhosis in a nationwide cohort study. J. Am. Acad. Dermatol. 2021, 84, 1085–1086.
- Cozzani, E.; Herzum, A.; Burlando, M.; Parodi, A. Cutaneous manifestations of HAV, HBV, HCV. Ital. J. Dermatol. Venerol. 2021, 156, 5–12.
- Mizukawa, Y.; Horie, C.; Yamazaki, Y.; Shiohara, T. Detection of varicella-zoster virus antigens in lesional skin of zosteriform lichen planus but not in that of linear lichen planus. Dermatology 2012, 225, 22–26.
- Ashraf, S.; Al-Maweri, S.A.; Alaizari, N.; Umair, A.; Ariffin, Z.; Alhajj, M.N.; Kassim, S.; Awan, K.H. The association between Epstein-Barr virus and oral lichen planus: A systematic review and meta-analysis. J. Oral Pathol. Med. 2020, 49, 969–976.
- Lahouel, M.; Aounallah, A.; Mokni, S.; Sriha, B.; Belajouza, C.; Denguezli, M. Severe childhood lichen planus pemphigoides after hepatitis A vaccination. Skin Health Dis. 2022, 2, e94.
- Calista, D.; Morri, M. Lichen planus induced by hepatitis B vaccination: A new case and review of the literature. Int. J. Dermatol. 2004, 43, 562–564.
- Lai, Y.C.; Yew, Y.W. Lichen planus and lichenoid drug eruption after vaccination. Cutis 2017, 100, E6–E20.
- Torre, K.; Grant-Kels, J.M.; Oliviero, M.; Rabinovitz, H. Lichen planus eruption following annual influenza vaccination. JAAD Case Rep. 2021, 10, 116–118.
- An, I.; Demir, V.; İbiloğlu, İ.; Akdeniz, S. Lichen planus secondary to rabies vaccination. Dermatol. Online J. 2017, 23, 13030.
- Rosengard, H.C.; Wheat, C.M.; Tilson, M.P.; Cuda, J.D. Lichen planus following tetanus-diphtheria-acellular pertussis vaccination: A case report and review of the literature. SAGE Open Med. Case Rep. 2018, 6, 2050313X17750335.
- Awada, B.; Abdullah, L.; Kurban, M.; Abbas, O. Inverse lichen planus post Oxford-AstraZeneca COVID-19 vaccine. J. Cosmet. Dermatol. 2022, 21, 883–885.
- Diab, R.; Araghi, F.; Gheisari, M.; Kani, Z.A.; Moravvej, H. Lichen planus and lichen planopilaris flare after COVID-19 vaccination. Dermatol. Ther. 2022, 35, e15283.
- Herzum, A.; Burlando, M.; Molle, M.F.; Micalizzi, C.; Cozzani, E.; Parodi, A. Lichen planus flare following COVID-19 vaccination: A case report. Clin. Case Rep. 2021, 9, e05092.
- Guarneri, C.; Ceccarelli, M.; Rinaldi, L.; Cacopardo, B.; Nunnari, G.; Guarneri, F. Helicobacter pylori and skin disorders: A comprehensive review of the available literature. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 12267–12287.
- Li, S.; Zhang, Y.; Yang, Z.; Li, J.; Li, Y.; Li, H.; Li, W.; Jia, J.; Ge, S.; Sun, Y. Helicobacter pylori infection is correlated with the incidence of erosive oral lichen planus and the alteration of the oral microbiome composition. BMC Microbiol. 2021, 21, 122.
- Kazanowska-Dygdala, M.; Dus, I.; Radwan-Oczko, M. The presence of Helicobacter pylori in oral cavities of patients with leukoplakia and oral lichen planus. J. Appl. Oral Sci. 2016, 24, 18–23.
- Lin, D.; Yang, L.; Wen, L.; Lu, H.; Chen, Q.; Wang, Z. Crosstalk between the oral microbiota, mucosal immunity, and the epithelial barrier regulates oral mucosal disease pathogenesis. Mucosal. Immunol. 2021, 14, 1247–1258.
- Ghone, U.; Sarode, G.S.; Sengupta, N.; Sarode, S.C. Are fungi responsible for the pathogenesis of oral lichen planus? Med. Hypotheses 2021, 156, 110689.
- Zhong, E.F.; Chang, A.; Stucky, A.; Chen, X.; Mundluru, T.; Khalifeh, M.; Sedghizadeh, P.P. Genomic Analysis of Oral Lichen Planus and Related Oral Microbiome Pathogens. Pathogens 2020, 9, 952.
- Rasul, T.F.; Anderson, J.; Bergholz, D.R.; Faiz, A.; Prasad, R.R. Gold Dental Implant-Induced Oral Lichen Planus. Cureus 2022, 14, e21852.
- Belhareth, K.; Korbi, M.; Belhadjali, H.; Soua, Y.; Moussa, A.; Youssef, M.; Zili, J. Pediatric lichen planus pigmentosus possibly triggered by mercury dental amalgams. Pediatr. Dermatol. 2020, 37, 375–376.
- Thanyavuthi, A.; Boonchai, W.; Kasemsarn, P. Amalgam Contact Allergy in Oral Lichenoid Lesions. Dermatitis 2016, 27, 215–221.
- Reichart, P.A.; Warnakulasuriya, S. Oral lichenoid contact lesions induced by areca nut and betel quid chewing: A mini review. J. Investig. Clin. Dent. 2012, 3, 163–166.
- Liu, W.; Yang, Y.; Zhang, X.; Shi, H. Oral potentially malignant disorder research in Taiwan and mainland China: A scientometric analysis. J. Dent. Sci. 2022, 17, 1854–1858.
- Guillet, G.; Coindre, M.; Levillain, P.; Guillet, M.H. Lichenoid dermatitis resulting from sensitization to dimethylfumarate: Atypical presentation of “Chinese sofa dermatitis”. Ann. Dermatol. Venereol. 2009, 136, 279–281.
- Ajaaouani, R.; Hali, F.; Marnissi, F.; Meftah, A.; Chiheb, S. A Generalized Form of Lichen Planus Pemphigoid Induced by an Oral Antidiabetic. Cureus 2022, 14, e31094.
- Fessa, C.; Lim, P.; Kossard, S.; Richards, S.; Fernandez Penas, P. Lichen planus-like drug eruptions due to β-blockers: A case report and literature review. Am. J. Clin. Dermatol. 2012, 13, 417–421.
- Baccino, D.; Merlo, G.; Cozzani, E.; Rosa, G.M.; Tini, G.; Burlando, M.; Parodi, A. Cutaneous effects of antihypertensive drugs. G. Ital. Dermatol. Venereol. 2020, 155, 202–211.
- Yuyaem, T.; Sudchada, P.; Srisuttiyakorn, C.; Juntawong, J.; Khanngern, N.; Watcharapokin, N.; Chansangiam, P. Ethambutol Induced Lichenoid Drug Eruption: A Case Report. Curr. Drug. Saf. 2021, 16, 296–298.
- Mastorino, L.; Ortoncelli, M.; Giura, M.T.; Avallone, G.; Viola, R.; Quaglino, P.; Ribero, S. Lichen ruber planus arising during dupilumab treatment for atopic dermatitis. Ital. J. Dermatol. Venerol. 2022, 157, 449–450.
- Oliveira, S.C.; Vasconcelos, A.H.C.; Magalhaes, E.P.B.; Correa, F.J.V.; Rodrigues, C.E.M. Clinical, Histopathological and Outcome Analysis of Five Patients with Lichenoid Eruption following Anti-Tumor Necrosis Factor-Alpha Therapy for Ankylosing Spondylitis: Report of One Case and Review of the Literature. Cureus 2020, 12, e10598.
- Shah, R.R.; Bhate, C.; Hernandez, A.; Ho, C.H. Lichen planus pemphigoides: A unique form of bullous and lichenoid eruptions secondary to nivolumab. Dermatol. Ther. 2022, 35, e15432.
- Kluger, N. Radiation-associated lichen planus: A case report and literature review. Acta Dermatovenerol. Alp. Pannonica Adriat. 2017, 26, 105–108.
- Zhang, X.; Lei, L.; Jiang, L.; Fu, C.; Huang, J.; Hu, Y.; Zhu, L.; Zhang, F.; Chen, J.; Zeng, Q. Characteristics and pathogenesis of Koebner phenomenon. Exp. Dermatol. 2022, 1–14.
- Lim, A.; Tang, P.Y.; Oh, C.C. Lichen planus pemphigoides after body tattooing. J. Cosmet. Dermatol. 2020, 19, 3048–3052.
- Cerqueira, J.D.M.; Moura, J.R.; Arsati, F.; Lima-Arsati, Y.B.O.; Bittencourt, R.A.; Freitas, V.S. Psychological disorders and oral lichen planus: A systematic review. J. Investig. Clin. Dent. 2018, 9, e12363.
- Chen, H.X.; Blasiak, R.; Kim, E.; Padilla, R.; Culton, D.A. Triggers of oral lichen planus flares and the potential role of trigger avoidance in disease management. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 248–252.
- Sufiawati, I.; Megawati, A.; Al Farisyi, M.; Putra, I. A Case Series of Psychological Stress Evaluation as a Risk Factor for Oral Lichen Planus. Case Rep. Dent. 2022, 2022, 1915122.
- Geng, L.; Zhang, X.; Tang, Y.; Gu, W. Identification of Potential Key Biomarkers and Immune Infiltration in Oral Lichen Planus. Dis. Markers 2022, 2022, 7386895.
More
