Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 1 by Jacob Yoong-Leong Oh.
The main advantage of Oblique Lumbar Interbody Fusion (OLIF) is its ability to provide safe access to the lumbar spine while being a robust interbody fusion technique through a minimally invasive approach. The rate of major complications after OLIF is minimal, making it a safe procedure with significant benefits outweighing the risks. The advantages of OLIF L2-5 with posterior stabilisation over stand-alone OLIF L2-5 is a subject of discussion.
- postoperative complications
- spinal fusion
- spine
- spondylosis
1. Introduction
The evolution of Oblique Lumbar Interbody Fusion (OLIF) dates back to 1997, when Mayer reported two new approaches to the lumbar spine: a retroperitoneal approach for lumbar levels L2-5, and a transperitoneal approach for L5-S1 [1]. Even though these approaches were initially termed as anterior approaches, they are now referred to as lateral approaches to the lumbar spine. Over time, the lateral retroperitoneal approach has been widely adopted for interbody fusion surgeries addressing various lumbar pathologies, especially degenerative conditions. This method has demonstrated its effectiveness as a robust technique for achieving interbody fusion through a minimally invasive approach. While fusion procedures performed using this approach can collectively be termed Lateral Lumbar Interbody Fusion (LLIF), they can be classified as either Oblique Lumbar Interbody Fusion (OLIF) or Direct Lateral Interbody Fusion (DLIF/XLIF) depending on whether the psoas muscle is retracted or split to reach the disc space (Figure 1) [2]. Recently, the lateral retroperitoneal approach has also been adapted for the L5-S1 level, which was previously considered to be only approachable through an anterior transperitoneal approach [3]. Hence, in addition to Posterior Lumbar Interbody Fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), and Anterior Lumbar Interbody Fusion (ALIF), OLIF has become a popular technique for treatment of multiple lumbar spinal conditions including spondylosis, spondylolisthesis, and kyphoscoliosis.
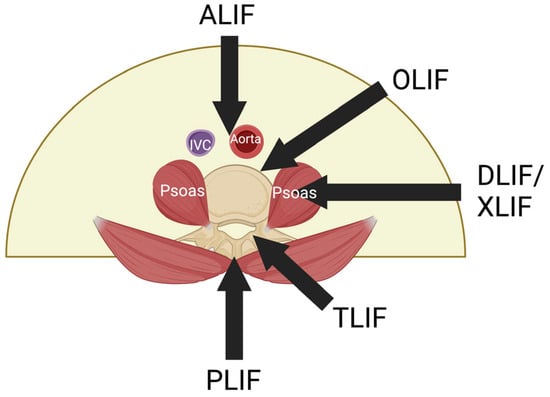
Figure 1. Various lateral interbody fusion approaches. ALIF is conducted through the anterior abdominal wall, bypassing the aorta and inferior vena cava. DLIF/XLIF approach is through the psoas major muscle. OLIF uses the oblique corridor anterior to the psoas major muscle. ALIF: Anterior Lumbar Interbody Fusion; OLIF: Oblique Lumbar Interbody fusion; DLIF: Direct Lateral Interbody fusion; XLIF: Extreme Lateral Interbody Fusion; TLIF: Transforaminal Lumbar Interbody Fusion; PLIF: Posterior Lumbar Interbody Fusion.
The advantages of the lateral approach have been well established [4]. It allows for the placement of a wide-bodied interbody cage, which allows for more stability and provides a larger surface area [5]. In addition, there are other benefits such as good sagittal and coronal correction, the ability of indirect decompression, multi-level minimally invasive surgery (MIS) fusions, and an excellent fusion technique [6,7][6][7]. This is especially so in the context of revision surgeries, where scar tissue may make it difficult to conduct the operation. Among the lateral approaches, OLIF for lumbar levels L2-5 (OLIF L2-5) offers an additional advantage over the DLIF/XLIF approach, as it does not require the dissection of the psoas major muscle that risks disruption of the lumbar nerve plexus which can lead to post-operative hip flexion weakness (27.5%) and other neurologic injuries (36.07%) [8,9][8][9]. Hence, OLIF has become a safer alternative to posterior approaches, especially for lumbar levels L2-5 as the retroperitoneal corridor that is being accessed is anterior to the psoas major muscle [10], avoiding complications of damaging it, and also avoiding anatomical complications of the anterior approach [11].
OLIF L2-5 can be performed alone or with additional posterior stabilisation with pedicle screws [12]. For patients with no comorbidities such as obesity, osteoporosis, or lumbar disc herniation, stand-alone OLIF may be sufficient and is shown to be equally stable as OLIF with posterior stabilisation due to the presence of intact posterior elements and bilateral spinal muscles [12]. However, OLIF with posterior stabilisation allows for a better dispersal of impact and therefore offers additional protection to the endplates than a stand-alone OLIF, thereby increasing fusion rates and decreasing rates of post-operative cage subsidence [13,14][13][14]. However, additional posterior stabilisation may pose a higher risk for complications as it increases operative time, tissue damage, and blood loss, and also incurs higher implant costs to patients [12,15][12][15].
2. Complications Associated with Oblique Lumbar Interbody Fusion
The pre-psoas approach for OLIF involves placing the patient in a lateral decubitus position, dissecting the abdominal wall muscles, mobilizing the peritoneum anteriorly, and then retracting the psoas muscle to reach the disc space [41,42][16][17]. This is followed by discectomy and implantation of a wide-bodied interbody cage. As discussed earlier, this stand-alone OLIF can be considered sufficient for patients without any co-morbidities and requiring short fusion [12]. However, given the stability and other advantages that a posterior fixation can offer, OLIF combined with posterior stabilisation is often performed nowadays [13[13][14],14], for which the patient is turned prone after placement of the OLIF cage and posterior instrumentation is performed with pedicle screws and rods in the usual way. This can either be completed in a single sitting or in two sittings, as per the surgeon’s discretion. Despite the various advantages that this type of fusion offers, as with any procedure, it comes with a set of reported complications that need to be considered.
On the other hand, the OLIF technique has evolved, and since many surgeons have now adopted this technique, the mean operative time for single-level OLIF was found to be shorter when compared to the study by Mayer, which is 107.3 ± 14.5 min [1]. The technique can also be considered safe, as reflected by the pooled major complications rate of just 1.7% inferred in the study. Of the five major complications which were deemed to be life-threatening or had long-term debilitative effects, three were major vascular injuries. All three had left common iliac vein injury, which was ligated and repaired intraoperatively. The other two were spinal nerve root injuries. In addition, there were 16 minor complications involving the segmental arteries or the lumbar venous plexus, which are associated with lower morbidity and mortality.
Even though none of the patients required a re-operation, especially due to implant related issues, adjacent segment disease (ASD) led to re-operation in three cases, reported by Kotani et al., where initially OLIF with posterior fixation was performed [31][18]. Overall, it noted ASD to be reported in five studies with an incidence of 2.8%. Being a common complication following spinal fusion occurring due to increased mechanical stress on adjacent discs [46[19][20],47], it needs to be monitored in follow-up radiographs. If need be, re-operation is required to extend the fusion and instrumentation to include the newly degenerated level [48][21].
Further analysis by comparing stand-alone OLIF L2-5 and OLIF L2-5 with posterior stabilisation showed that there was no significant difference in pooled prevalence of complications in general, as well as pertaining to major complications specifically. This corroborates with He et al.’s study, wherein they concluded that there was no significant difference in complications between the two OLIF subtypes [12]. Given that the addition of posterior pedicle screws does not lead to any additional major complications, considering the stability it offers, it can be performed safely if deemed necessary by the surgeon [12]. Biomechanical studies highlight the significant stability that the addition of posterior stabilisation could offer to OLIF [49][22]. Looking at cage subsidence, OLIF L2-5 with posterior stabilisation had almost a similar subsidence rate of 4.5% compared to 3.2% with stand-alone OLIF L2-5. This also indicates that, if cases are chosen appropriately, stand-alone OLIF offers adequate stability, probably due to the intact posterior elements and bilateral spinal muscles, which could help stabilize the spine. However, it should be noted that not all studies reported subsidence based on number of patients. Three studies reported based on number of levels rather than patients, and hence were excluded from our analysis [20,25,27][23][24][25]. Considering the clinical outcomes at two years post-op, He et al. showed that there is no significant difference between stand-alone OLIF L2-5 and OLIF L2-5 with posterior stabilisation [12].
Furthermore, scrutinizing the follow-up times between stand-alone-only and posterior stabilisation-only studies shows that the stand-alone-only studies may not have had a long-enough follow-up period with patients to detect cage subsidence. All three stand-alone-only OLIF papers reported results up to a maximum of 3–12 months post-operatively [21,30,33][26][27][28]. Compared to the other studies collated, where there were results reported longer post-operatively, the short time of reported results may have caused bias in the data collected, hence skewing the numbers regarding complications post-OLIF. This is even more pertinent for late post-operative complications such as cage subsidence, where other studies have indicated that average time-to-subsidence is 3.7 months post-OLIF [50][29]. As such, the risk–benefit analysis of using OLIF L2-5 with posterior stabilisation compared to stand-alone OLIF L2-5 is still up to debate, and surgeons should be wary of these limitations.
3. Conclusions
Even though the overall results indicated a complication rate of 24.7%, major complications were very minimal at 1.7%. Hence, OLIF can be considered safe, wherein the benefits largely outweigh the risks. Currently, the benefits of employing OLIF L2-5 with posterior stabilisation in contrast to performing stand-alone OLIF L2-5 can be a subject for discussion. However, as the body of evidence on performing OLIF L2-5 with posterior stabilisation grows, further studies and meta-analysis could unveil the specifics concerning the supplementary posterior stabilisation. Furthermore, studies explicitly stating all complications, be it major or minor, are necessary to establish precise evidence regarding the benefits of OLIF in comparison to other fusion techniques. This will allow surgeons to make informed decisions along with patients prior to surgery.References
- Mayer, H.M. A New Microsurgical Technique for Minimally Invasive Anterior Lumbar Interbody Fusion. Spine 1997, 22, 691–700.
- Allain, J.; Dufour, T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop. Traumatol. Surg. Res. 2020, 106, S149–S157.
- Orita, S.; Shiga, Y.; Inage, K.; Eguchi, Y.; Maki, S.; Furuya, T.; Aoki, Y.; Inoue, M.; Hynes, R.A.; Koda, M.; et al. Technical and Conceptual Review on the L5-S1 Oblique Lateral Interbody Fusion Surgery (OLIF51). Spine Surg. Relat. Res. 2021, 5, 1–9.
- Salzmann, S.N.; Shue, J.; Hughes, A.P. Lateral Lumbar Interbody Fusion-Outcomes and Complications. Curr. Rev. Musculoskelet. Med. 2017, 10, 539–546.
- Yuan, W.; Kaliya-Perumal, A.K.; Chou, S.M.; Oh, J.Y. Does Lumbar Interbody Cage Size Influence Subsidence? A Biomechanical Study. Spine 2020, 45, 88–95.
- Patel, R.S.; Suh, S.W.; Kang, S.H.; Nam, K.Y.; Siddiqui, S.S.; Chang, D.G.; Yang, J.H. The Radiologic and Clinical Outcomes of Oblique Lateral Interbody Fusion for Correction of Adult Degenerative Lumbar Deformity. Indian J. Orthop. 2019, 53, 502–509.
- Shimizu, T.; Fujibayashi, S.; Otsuki, B.; Murata, K.; Matsuda, S. Indirect decompression via oblique lateral interbody fusion for severe degenerative lumbar spinal stenosis: A comparative study with direct decompression transforaminal/posterior lumbar interbody fusion. Spine J. 2021, 21, 963–971.
- Tohmeh, A.G.; Rodgers, W.B.; Peterson, M.D. Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J. Neurosurg. Spine 2011, 14, 31–37.
- Hijji, F.Y.; Narain, A.S.; Bohl, D.D.; Ahn, J.; Long, W.W.; DiBattista, J.V.; Kudaravalli, K.T.; Singh, K. Lateral lumbar interbody fusion: A systematic review of complication rates. Spine J. 2017, 17, 1412–1419.
- Ng, J.P.; Kaliya-Perumal, A.K.; Tandon, A.A.; Oh, J.Y. The Oblique Corridor at L4-L5: A Radiographic-Anatomical Study into the Feasibility for Lateral Interbody Fusion. Spine 2020, 45, E552–E559.
- Li, R.; Li, X.; Zhou, H.; Jiang, W. Development and Application of Oblique Lumbar Interbody Fusion. Orthop. Surg. 2020, 12, 355–365.
- He, W.; He, D.; Sun, Y.; Xing, Y.; Wen, J.; Wang, W.; Xi, Y.; Liu, M.; Tian, W.; Ye, X. Standalone oblique lateral interbody fusion vs. combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet. Disord. 2020, 21, 184.
- Huang, S.; Min, S.; Wang, S.; Jin, A. Biomechanical effects of an oblique lumbar interbody fusion combined with posterior augmentation: A finite element analysis. BMC Musculoskelet. Disord. 2022, 23, 611.
- Bereczki, F.; Turbucz, M.; Kiss, R.; Eltes, P.E.; Lazary, A. Stability Evaluation of Different Oblique Lumbar Interbody Fusion Constructs in Normal and Osteoporotic Condition—A Finite Element Based Study. Front. Bioeng. Biotechnol. 2021, 9, 749914.
- Cai, K.; Luo, K.; Zhu, J.; Zhang, K.; Yu, S.; Ye, Y.; Jiang, G. Effect of pedicle-screw rod fixation on oblique lumbar interbody fusion in patients with osteoporosis: A retrospective cohort study. J. Orthop. Surg. Res. 2021, 16, 429.
- Woods, K.R.; Billys, J.B.; Hynes, R.A. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017, 17, 545–553.
- Davis, T.T.; Hynes, R.A.; Fung, D.A.; Spann, S.W.; MacMillan, M.; Kwon, B.; Liu, J.; Acosta, F.; Drochner, T.E. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: An anatomic study. J. Neurosurg. Spine 2014, 21, 785–793.
- Kotani, Y.; Koike, Y.; Ikeura, A.; Tokunaga, H.; Saito, T. Clinical and radiologic comparison of anterior-posterior single-position lateral surgery versus MIS-TLIF for degenerative lumbar spondylolisthesis. J. Orthop. Sci. 2020, 26, 992–998.
- Lee, J.C.; Choi, S.W. Adjacent Segment Pathology after Lumbar Spinal Fusion. Asian Spine J. 2015, 9, 807–817.
- Donnally III, C.J.; Patel, P.D.; Canseco, J.A.; Divi, S.N.; Goz, V.; Sherman, M.B.; Shenoy, K.; Markowitz, M.; Rihn, J.A.; Vaccaro, A.R. Current incidence of adjacent segment pathology following lumbar fusion versus motion-preserving procedures: A systematic review and meta-analysis of recent projections. Spine J. 2020, 20, 1554–1565.
- Burch, M.B.; Wiegers, N.W.; Patil, S.; Nourbakhsh, A. Incidence and risk factors of reoperation in patients with adjacent segment disease: A meta-analysis. J. Craniovertebr. Junction Spine 2020, 11, 9–16.
- Fang, G.; Lin, Y.; Wu, J.; Cui, W.; Zhang, S.; Guo, L.; Sang, H.; Huang, W. Biomechanical Comparison of Stand-Alone and Bilateral Pedicle Screw Fixation for Oblique Lumbar Interbody Fusion Surgery-A Finite Element Analysis. World Neurosurg. 2020, 141, e204–e212.
- Jin, C.; Jaiswal, M.S.; Jeun, S.S.; Ryu, K.S.; Hur, J.W.; Kim, J.S. Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J. Orthop. Surg. Res. 2018, 13, 38.
- Zhang, C.; Wang, K.; Jian, F.; Wu, H. Efficacy of Oblique Lateral Interbody Fusion in Treatment of Degenerative Lumbar Disease. World Neurosurg. 2019, 124, e17–e24.
- Lin, G.X.; Kotheeranurak, V.; Zeng, T.H.; Mahatthanatrakul, A.; Kim, J.S. A longitudinal investigation of the endplate cystic lesion effect on oblique lumbar interbody fusion. Clin. Neurol. Neurosurg. 2019, 184, 105407.
- Jin, J.; Ryu, K.S.; Hur, J.W.; Seong, J.H.; Kim, J.S.; Cho, H.J. Comparative Study of the Difference of Perioperative Complication and Radiologic Results: MIS-DLIF (Minimally Invasive Direct Lateral Lumbar Interbody Fusion) Versus MIS-OLIF (Minimally Invasive Oblique Lateral Lumbar Interbody Fusion). Clin. Spine Surg. 2018, 31, 31–36.
- Huo, Y.; Yang, D.; Ma, L.; Wang, H.; Ding, W.; Yang, S. Oblique Lumbar Interbody Fusion with Stand-Alone Cages for the Treatment of Degenerative Lumbar Spondylolisthesis: A Retrospective Study with 1-Year Follow-Up. Pain Res. Manag. 2020, 2020, 9016219.
- Liu, J.; He, Y.; Huang, B.; Zhang, X.; Shan, Z.; Chen, J.; Fan, S.; Zhao, F. Reoccurring discogenic low back pain (LBP) after discoblock treated by oblique lumbar interbody fusion (OLIF). J. Orthop. Surg. Res. 2020, 15, 22.
- Kotheeranurak, V.; Jitpakdee, K.; Lin, G.X.; Mahatthanatrakul, A.; Singhatanadgige, W.; Limthongkul, W.; Yingsakmongkol, W.; Kim, J.S. Subsidence of Interbody Cage Following Oblique Lateral Interbody Fusion: An Analysis and Potential Risk Factors. Glob. Spine J. 2021, 13, 1981–1991.
More
