Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Andreia Garces and Version 2 by Camila Xu.
Antibiotic resistance is a global concern that affects not only human health but also the health of wildlife and the environment. Wildlife can serve as reservoirs for antibiotic-resistant bacteria, and antibiotics in veterinary medicine and agriculture can contribute to the development of resistance in these populations.
- mammals
- wild
- carnivores
- bacteria
- antibiotics
- contamination
- resistance
1. Introduction
Antimicrobial resistance (AMR) is considered one of the leading public health problems of the 21st century [1]. Although AMR has always existed, the overuse and misuse of antibiotics have increased antibiotic-resistant strains [2]. In recent decades, selective pressure has been generated by the use of antibiotics in medicine, veterinary, and agricultural practices, which has been responsible for a significant increase in antibiotic resistance [3].
“One Health” is a concept wherein human, animal, and environmental health are interconnected [4]. One of the greatest problems with “One Health” is antimicrobial resistance. This problem affects these three groups simultaneously. Humans and domestic and wild animals can be hosts and spreaders of AMR bacteria. Moreover, bacteria are continuously exchanged between the different environmental niches [5][6][5,6].
Although most wildlife prefer to live far from humans, some species have adapted and can live in contact with domestic animals or humans in urban environments. Therefore, they can be recognized as potential indicators of AMR dissemination [7]. Wild animals usually do not receive antibiotics or veterinary care, except in cases of interventions in endangered animals, admissions to wildlife rehabilitation centers, or treatments during disease outbreaks [8]. Studies have shown that AMR in most wildlife is associated with environmental exposure to anthropogenic AMR contamination [8]. Air, water, land, and food are some of the sources of AMR [9]. Bodies of water, such as rivers, lakes, or seas, can be contaminated with industrial discharges, agricultural discharges (fecal sludge from farms), domestic sewage, discharges from hospitals (human and veterinary), and wastewater treatment plants, among others [8][10][11][8,10,11]. Fertilizers used in agriculture can be a source of AMR [8]. In addition to environmental pressures, there are intrinsic mechanisms in bacteria that may contribute to the development of antimicrobial resistance, such as bacterial permeability, efflux pumps, target receptor modification, or horizontal gene transfer between bacteria via mobile genetic elements (e.g., plasmids, transposons, integrons) [3][12][3,12]. The presence of AMR in wildlife is also associated with other factors, such as habitat use, foraging behavior, and species’ habitats [3][8][3,8]. Habitat destruction, the loss of biodiversity, climate change, the accumulation of toxic pollutants, and the invasion of exotic species and pathogens have also contributed to the spread of AMR [13].
Contact between anthropogenic source areas and wild animals has increased due to human expansion. Some animals—for example, foxes and hedgehogs—have adapted and now live and thrive in urban areas [1][14][1,14]. Animals in these areas can feed on human domestic waste [15]. These contacts can potentially contribute to the emergence of new pathogens and AMR in wildlife, which can promote higher mortality rates. When animals survive, they can become bacterial reservoirs and spread throughout the environment again [13][16][13,16]. A study performed in Botswana showed that the prevalence of AMR Escherichia coli was highest in carnivores (62.5%) and animals using urban habitats (25.6%) when compared to herbivores (9.1%) and animals using protected/rural habitats (9.0%) [8].
Despite the abundance of literature on AMR in the medical and veterinary fields, available studies focus mainly on some bacterial species, such as Escherichia coli or Salmonella spp., and some species of wild animals, mainly birds and mammals [6][7][8][6,7,8]. Carnivores are a very diverse group of species in Europe, with some populations living in remote areas and others in urban areas in close contact with humans [10][15][10,15].
2. European Wild Carnivorous
Carnivora is an order of mammals that eats meat, by predation or necrophagy. They have specialized teeth for their meat-based diet, with fang-like canines, which they use to kill their prey and cut the meat into pieces [17][18][17,18]. Some animals in this order can also consume vegetation, insects (omnivores), and meat [17]. Carnivores can be found in diverse habitats, including cold polar regions, desert regions, forests, open seas, and urban areas [19]. The order Carnivora includes 16 families and 9 terrestrial families: Canidae, Felidae, Ursidae, Procyonidae, Mustelidae, Herpestidae, Viverridae, and Hyaenidae. In Europe, there are approximately 63 species of carnivorous mammals, both terrestrial and marine. Some of these species are threatened according to the IUCN Red List of Threatened Species, such as the Iberian lynx (endangered) or the Balkan lynx (critically endangered) [17]. These include larger predators, such as wolves, bears, and lynxes, and smaller carnivores like foxes, weasels, and mustelids. Historically, throughout the continent, these species have all experienced a dramatic decline in their populations and distributions due to anthropogenic factors (hunting, habitat destruction, pollution) [18][20][21][18,20,21]. Table 1 presents some information regarding the distribution, conservation status, and diet of some of the carnivorous species included in this research, to understand better the source of the acquisition of AMR strains of bacteria.Table 1. Species, family, distribution, diet, habitat, behavior, and conservation status (LC—Least Concern, V—Vulnerable, NT—Near Threat) of wild carnivore species from Europe.
| Species | Family | Distribution | Diet | Habitat | Behavior | Conservation Status | Ref. |
|---|
| Species | SpeciesCountry | Year | Type of Sample | Isolated Bacteria | Antibiotic Resistance * | Resistance Genes | Ref. |
|---|---|---|---|---|---|---|---|
| Country | Year | Type of Sample | Isolated Bacteria | Antibiotic Resistance * | Resistance Genes | Ref. | |
| Beech marten (Martes foina, Erxleben, 1777) | Mustelidae | Europe, except most Mediterranean islands, the Balkan peninsula, the Scandinavian peninsula, and the United Kingdom | |||||
| Iberian Lynx (Lynx pardinus) | Portugal | 2008–2010 | Feces | E. casseliflavus | |||
| Eurasian otter ( | Plants, fruit, rats, mice, small mammals, birds | Urban areas, forest habitats, and rural areas | Crepuscular and nocturnal | LC | |||
| S. sciuri | |||||||
| group, | |||||||
| S. equorum | |||||||
| , | |||||||
| S. capitis | |||||||
| MET, CL, AMC, AMP, ENR, FD, DA, TET | |||||||
| mecA | |||||||
| [ | |||||||
| 8 | |||||||
| ] | |||||||
* AMC: amoxicillin/clavulanic acid; AMP: ampicillin; STR: streptomycin; E: erythromycin; ENR: enrofloxacin; E: erythromycin; BE: benzylpenicillin; C: chloramphenicol; CD: clindamycin; CEF: ceftiofur; CEP: cephalothin; CN: gentamicin; CPN: cephalexin; CRO: ceftriaxone; CTX: cefotaxime; DXT: doxycycline; F: nitrofurantoin; IMI: imipenem; INN: cefovecin; KF: cephalothin; MAR: marbofloxacin; NEO: neomycin; PRA: pradofloxacin; PX: cefpodoxime; SXT: trimethoprim/sulfamethoxazole; TE: tetracycline; N: nalidixic acid; CIP: Ciprofloxacin; KAN: kanamycin; VAN: vancomycin; Q–D: quinupristin–dalfopristin; CZA: ceftazidime; FEP: cefepime; FOX: cefoxitin: FA: fusidic acid; DA: clindamycin; MET: methicillin.
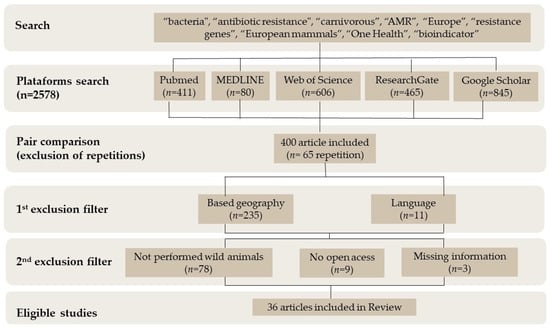
Table 3. Antibiotic resistance in animals from the family Ursidae regarding species, country, year, type of sample, bacteria isolated, antibiotic resistance, and resistance genes.
| Species | Country | Year | Type of Sample | Isolated Bacteria | Antibiotic Resistance * | Resistance Genes | Ref. | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Polar bear (Ursus maritimus) | [ | Svalbard | 22 | ] | ||||||||||||||||
| 2014 | Fecal | Clostridiales | n/a | Lutra lutra) | bla | TEM | TE, Q–D, E, STR | vanC2, tetM, ermB, hyl, cylA, acm, ebpABCcylL, | , gelE, [37] | |||||||||||
| Portugal | 2006–2008 | Feces | E. faecalis | , E. faecium, E. durans | n/a | ace, cylA, tetM, pbp5, vanB, vanD | [49] | , aac(60)-Ie-aph | [53] | European polecat (Mustela putorius, Linnaeus, 1758) | Mustelidae | Western European Russia, Western Belarus, Western Ukraine, Central and Western Europe, and North Africa | Lagomorphs, small rodents, amphibians, birds, reptiles, and insects | PortugalRiparian and agricultural areas to meadows and forest areas | Nocturnal | LC | [ | |||
| Svalbard | 2004–2006 | Fecal | Clostridiales, Firmicutes, E. coli | 23 | ] | |||||||||||||||
| n/a | 2008–2010 | Feces | ||||||||||||||||||
| Portugal | 2015–2016 | Enterococcus | spp., E. coli | bla | TEM | TE, E, STR, N, SXT, | Feces | Enterococcus spp.cpd, cylB, and cylL, | AMC, AMP, C, CN, DA, ENR, P, TE, VANblaTEM, tetA, aadA, cmlA, [50] | n/a | dfrA1 + aadA1, dfrA12 + aadA2, fimA | [36] | Brown bear (Ursus arctos, Linnaeus, 1758) | Ursidae | Europe, Asia, Atlas Mountains, North America | Omnivore | Mountain woodlands, forest | Crepuscular | LC | [24] |
| Brown bears (Ursus arctos) | Slovenia | 2010–2012 | Fecal | E. coli | ||||||||||||||||
| [ | 54 | ] | n/a | fimH | , | ompT, kpsMT, ibeA, traT | [51 | Portugal] | 2008–201034] | |||||||||||
| Feces | Enterococcus | spp. | TE, E, KAN, N | Italy | ||||||||||||||||
| Portugal | 2022 | Forearm wound, exposed fracture | Streptococcus dysgalactiae spp. equisimilis, Leclercia adecarboxilara | AMP, C, CEF, CEP, CN, CPN, DX, ENR, INN, MAR, PRA, PX, SXT, TE | n/a | [34] | ||||||||||||||
| Italy | 2022 | Carpal wound, intraarticular swab | ||||||||||||||||||
| Slovakia | 2020 | Feces | Enterococcus spp. | TE, AMP, VAN, E | [46] | Streptococcus canis, E. coli, Pseudomonas aeruginosa | AMP, C, CPN, CEP, DXT, ENR, INN, MAR, NEO, PRA, SXT, TE, AMC, CEF, CN, CPN, IMI, F | n/a | [34] | |||||||||||
| Iberian wolves (Canis lupus signatus) | Portugal | 2008–2010 | Feces | E. coli | TE, AMP, STR, CEP, N, SXT, CIP | cdt, chuA, cvaC, eaeA, paa, bfpA, blaCTX-M-1, blaCTX-M-9 | [35] | |||||||||||||
| Portugal | 2008–2009 | Feces | Enterococcus faecium, E. hirae, E. faecalis, E. durans | AMP, TE, STR | tetM, tetL, ermB, blaTEM, tetA, tetB, aadA, strA-strB | [36] | ||||||||||||||
| Portugal | 2008–2010 | Feces | E. faecium, E. gallinarum | TET, VAN, AMP, E, KAN | vanC1, vanA, tetM, ermB; aph(3′)-IIIa, tet(L); Tn916, hyl | [37] | ||||||||||||||
| Golden jackal (Canis aureus) | Italy | 2023 | Lung, liver, spleen, kidney, and intestine | n/a | n/a | tetM, tetP, Southeastern Europe, Moldova, Asia Minor, and the Caucasus | Omnivorous diet, plants, fruit, rodents, rabbits | Valleys, beside rivers canals, lakes, seashores | Crepuscular | LC | [32] |
3. Antibiotic Resistance in Wild Carnivores
For this research, the inclusion criteria were as follows: studies only performed in free-range animals, species of European terrestrial carnivores, studies conducted in Europe, and studies that included bacteria, phenotypic resistance, and/or resistance genes. The initial search identified 2578 articles on the databases (ResearchGate, MEDLINE, PubMed, Web of Science, and Google Scholar) using the terms “bacteria”, “antibiotic resistance”, “carnivorous”, “AMR”, “Europe”, “resistance genes”, “European mammals”, “One Health”, and “bioindicator”. On the 2578 articles collected, a first screening was performed based on the information in the abstracts. A total of 2178 were excluded since they did not have the necessary information for the research. From the remaining 400, 65 were duplicates and therefore excluded. Another 235 were excluded due to geography (studies performed outside Europe). Eleven were removed due to language, since only English, Spanish, and Portuguese manuscripts were included in this research. With a secondary exclusion filter screening the full articles, 78 were excluded since they were not performed in wild animals or did not include all the information required, and 9 were not open-access full articles. Therefore, a total of 36 articles had all the information required and were included in this research (Figure 1). Table 2, Table 3, Table 4 and Table 5 is presented the information from the papers selected.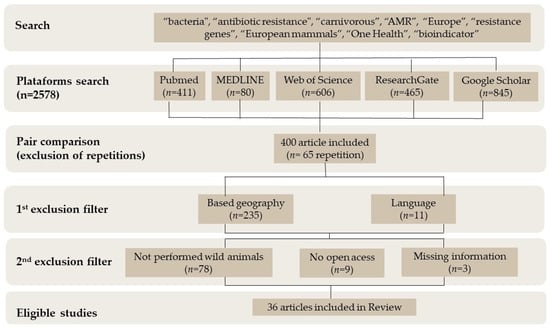
Figure 1.
Flow diagram of data collection.
Table 2. Antibiotic resistance in animals from the family Canidae regarding species, country, year, type of sample, bacteria isolated, antibiotic resistance, and resistance genes.
| Species | Country | Year | Type of Sample | Isolated Bacteria | Antibiotic Resistance * | Resistance Genes | Ref. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Apennine wolf (Canis lupus italicus) | Italy | 2015–2017 | Feces | Citrobacter spp., Escherichia coli, Hafnia alvei, Salmonella spp., Serratia spp. | AMC, AMP, STR | n/a | [33] | ||||||||
| Italy | 2017 | Feces | n/a | TE | tetA, tetP | [7] | |||||||||
| Italy | 2022 | Endocardial swab, lung, thoracic effusion | Staphylococcus pseudointermedius, Enterococcus faecalis, E. coli | 2006AMC, E, ENR, MAR, CXT, C, SXT, TE, P, DXT | Feces | Aeromonas hydrophila, A. hydrophila/caviae, A. sobriatetM, tetL, ermB, aac (6′)-Ie-aph(2″)-Ia, ant(6)-Ia, aph(3′)-IIIa | [52] | ||||||||
| Polar bear (Ursus maritimus, Phipps, 1774) | |||||||||||||||
| P, CLI, E, VAN, AMP | n/a | [ | 55 | ] | Ursidae | Greenland, Canada, Alaska, Russia, and the Svalbard Archipelago of Norway | Seals, walruses, sea birds, eggs, small mammals, fish, reindeer/caribou, seaweed/kelp, land plants | Portugal | 2008–2010Ice fields | Diurnal | V | Feces | E. coli | TE, STR, SXT, N, AMP, CIP | blaTEM, blaSHV, tetA[25] |
| n/a | [ | 34 | ] | ||||||||||||
| Italy | 2022 | Peritoneal effusion, lung, endocardial swab, liver parenchyma, pleural effusion | Klebsiella oxytoca | AMP | , tetB, aadA, strA-strB, aac(3)-II, aac (3)-IV, aadA1, dfrA1 + aadA1, estX + psp + aadA2, aer, cnf1, fimA, papC, papG-allele III | [52] | |||||||||
| Portugal | 2006–2008 | Feces | S. arizona, S. pullorum, S. choleraesuis arizona | AMC, C, P, AMP, CL, ENR, GN, NA, S, TE | n/a | [16] | Red fox (Vulpes vulpes, Linnaeus, 1758) | Canidae | Northern hemisphere | Plants, rodents, birds, leporids, porcupines, raccoons, opossums, reptiles, insects, invertebrates | Scrubland, forest, agricultural fields, urban areas | Nocturnal | Wild cat (Felis silvestrisLC | ) | Germany[26] |
| n/a | [ | 2014 | Nasal swab | ||||||||||||
| Portugal | 2009 | Feces | E. coli, | S. aureus | Enterococcusn/a | spp.gapA, katA, CoA, Spa, sbi, nuc1, sarA, saeS, | CTX, ENR, SvraS, agrl | n/a | , hid | [13[45] | European badger (Meles meles, Linnaeus, 1758) | ||||
| ] | Mustelidae | Europe (except Scandinavia), Russia, and parts of Asia | Omnivores: plants, earthworms, large insects, small mammals, fruits | Lynx (Lynx lynx) | |||||||||||
| Spain | Sweden | 2006 | Liver tissue | 2018–2021 | FecesS. aureus | E. coli, Pseudomonas fluorescensDeciduous, mixed, and coniferous forests, agro-silver-pastoral landscapes, Mediterranean scrub forests, and open areas with patches of riparian vegetation | , Crepuscular and nocturnal | LC | Hafnia alvei, Serratia marcescensn/a | CIP, ENR, CN, SXT, TE, C | ermB, blaCTX-M-15, gapA, katA, CoA, Spa, sbi, nuc1, sarA, saeS, vraS, agrl, hid, agrlV, mecC[27] | ||||
| [ | 45 | ] | European otter (Lutra lutra, Linnaeus, 1758) | Mustelidae | Eurasia, North Africa, the Middle East, Sri Lanka, a part of India, and Indonesia | Fish, amphibians, insects | Rivers, streams, marshes, lagoons, and reservoirs | Nocturnal | NT | [28] |
* AMP: ampicillin; STR: streptomycin; E: erythromycin; SXT: trimethoprim/sulfamethoxazole; TE: tetracycline; N: nalidixic acid; CIP: ciprofloxacin; KAN: kanamycin; Q–D: quinupristin–dalfopristin.
Table 5. Antibiotic resistance in animals from the family Mustelidae regarding species, country, year, type of sample, bacteria isolated, antibiotic resistance, and resistance genes.
| tetM | |||||||||||||
| , | |||||||||||||
| bla | |||||||||||||
| CMY-2 | |||||||||||||
| , | |||||||||||||
| tetM | [ | 56 | ] | ||||||||||
| Germany | 2000–2012 | Nasal and perineal swabs | S. aureus | AMC, AMP, P, | mecC | [57] | |||||||
| Apennine wolf (Canis lupus italicus, Altobello, 1921) | Canidae | Italy, France, Spain, Switzerland | Roe deer, wild boar, red deer, livestock sheep, horses, Mouflon, Italian hare, birds, invertebrates, fruit, berries, grasses, herbs, and garbage | Temperate coniferous forests | Crepuscular, diurnal | ||||||||
| Portugal | 2018–2019 | Feces | E. coli, | AMP, SXT, TE, CTX, KAN, CN, PX, DXT, T | aac(3)-IV, aph(4)-Ia, aph(6)-Id, blaTEM-1B | V | , lnu(F), tet(B), aac(3)-Iva, aadA1, aac(2′)-Iia, qnrB19, adA5, aph(3″)-Ib, catA1, qnrB19, qnrB82, [29] | ||||||
| sulII | , | dfrA17 | [ | 58 | ] | Iberian wolves (Canis lupus signatus, Cabrera, 1907) | Canidae | Portugal, Spain | Wild boars, rabbits, roe deer, red deer, ibexes, small carnivores, and fish | Temperate forests | Crepuscular, diurnal | ||
| Slovakia | 2020 | Feces | EN | Enterococcus spp. | [ | 30 | ] | ||||||
| TE, E, AMP, VAN | n/a | [ | 46 | ] | Iberian Lynx (Lynx pardinus, Temminck, 1827) | Felidae | Portugal, Spain | Rabbits, small rodents | Mediterranean forests of woodland and shrubland interspersed with natural and artificial pastures | Crepuscular and nocturnal | EN | mcr-1 | |
| Spain | 2012–2015 | , | Nasal and rectal swabs | tetA | , | Staphylococcus spp.tetL, | N, P, FOX, FAtetM, tetO | n/a | , sul3, | [49[31] | |||
| bla | TEM−1 | ] | [ | 38 | ] | Golden jackal (Canis aureus, Linnaeus, 1758) | Canidae | ||||||
| Red Fox (Vulpes vulpes) | Portugal | 2008–2009 | Feces | E. coli | STR, TE, SXT, AMP | ||||||||
| Spain | adA, tetA, tetB, sul1, bla | TEM | 2015–2015 | [ | 39 | ] | |||||||
| Fecal | E. coli | AMP, TET, SXT | dfrA1 aadA1 qacE 1 | , | sul1, sul2, tetA | [59] | Portugal | 2008–2009 | Feces | E. faecium | TE | tetM, tetL, ermB, aph(30)-IIIa | [39] |
| Badger (Meles meles) | Ireland | 2018–2019 | Fecal, nasopharyngeal swabs | Salmonella spp., E. coli | AMP, CZA, CEP, CTX | n/a | [60] | Portugal | 2008–2009 | Feces | E. faecium, E. durans | ||
| Spain | TE, E | 2016–2017 | Swabs | E. coli | CIP, N, C, S, TermB, tetM, tetL, Tn916 | bla[40] | |||||||
| SHV-12 | [ | 61 | ] | Ireland | 2018–2019 | Fecal, nasopharyngeal swabs | E. coli | CZA, TE, SXT, CIP, AMP, FEP | |||||
| Poland | n/a | 2014–2018 | Rectal swabs | E. coli | AMP, S, KAN, C, CIP, S, N, TE | aph(3¢)-Ia, strA, aph(3¢)-Ia, sul2, tetA, tetB, floR, cat, sul3[41] | |||||||
| [ | 62 | ] | Norway | 2006 | Fecal | E. coli | SXT, TE, CIP, N | n/a | [1] | ||||
| Germany | 2011 | Pharyngeal swab | S. aureus | n/a | gapA, katA, CoA, Spa, sbi, nuc1, sarA, saeS, vraS, agrl, hid | [45] | Portugal | 2017–2019 | Fecal | E. coli, Enterococcus spp. | TE, C, CD, CN, AMC, AMP, BE, CEF, CEP, CZA, CPN, CRO | blaTEM, ermB, aadA, tetM, tetW, tetL, drfA1, drfA17 | [42 |
| Spain | ] | ||||||||||||
| 2015–2015 | Fecal | E. coli | AMP, TE | tetB | [ | 59] | Italy | 2016–2018 | Fecal | E. coli | |||
| Spain | n/a | 2012–2015 | eaeA | , | hlyA, stx1, and stx2, | Nasal and rectal swabs[43] | |||||||
| Staphylococcus | spp. | N, P, FOX, FA, CLI | n/a | [ | 63 | ] | Italy | 2002–2010 | Rectal swab | Salmonella enterica, S. typhimurium | AMC, TE, AMP, ENR | n/a | |
| Beech marten (Martes foina) | Poland | 2014–2018 | [ | 44 | ] | ||||||||
| Rectal swabs | E. coli | AMP, STR, KAN, C, CN, CIP, S, N, TE, CTX | strA | , | sul1 | , sul2, tetA, tetB, aph(3¢)-Ia, floR, cat, blaTEM-135 | [62] | Germany, Austria, Sweden | 2013, 2006, 2005, 2014 | Nasal swab | S. aureus | n/a | gapA, katA, CoA, |
| Spain | Spa | , | 2012–2015 | sbi | , nuc1, sarA, | Nasal and rectal swabs | Staphylococcus spp.saeS, | N, PEN, FOX, TEvraS, agrl, | n/ahid | [45] | |||
| [ | 49 | ] | Slovakia | 2020 | Feces | Enterococcus spp. | TE, AMP, VAN, E | n/a | [46] | ||||
| Spain | 2015–2015 | Fecal | E. coli | AMP, NAL, CIP | blaTEM-1b | [59] | Spain | 2012–2015 | Nasal and rectal swabs | Staphylococcus spp. | CD, F, AMP, BE, FOX, FA, NEO | n/a | [47] |
| Spain | 2016–2017 | Swabs | Citrobacter freundii | CIP, NAL, GEN, TET, SUL, TMP | black my-2, blaSHV-12 | [61] | Italy | 2017–2019 | Oral, skin, rectal, tracheal swab, feces | K. oxytoca | AMP, CD | ||
| European pine marten ( | n/a | Martes martes) | [ | 48 | ] | ||||||||
| Slovakia | 2020 | Feces | Enterococcus | spp. | TE, E, AMP, VAN | n/a | [46 | UK | 2007–2008 | Tissues |
* AMP: ampicillin; E: erythromycin; TE: tetracycline; VAN: vancomycin.
Table 4. Antibiotic resistance in animals from the family Felidae regarding species, country, year, type of sample, bacteria isolated, antibiotic resistance, and resistance genes.
| ] | |||||||
| Italy | |||||||
| 2002–2010 | |||||||
| Rectal swab | |||||||
| Salmonella | |||||||
| spp. | |||||||
| AM, AMC, TE | |||||||
| n/a | |||||||
| [ | |||||||
| 44 | |||||||
| ] | |||||||
| Italy | |||||||
| 2017–2019 | |||||||
| Oral, skin, rectal, tracheal swab, feces | E. coli | AMP, CD | n/a | [ | 48 | ] | |
| European polecat (Mustela putorius) | Poland | 2014–2018 | Rectal swabs | E. coli | AMP, STR, S, TET | strA, sul2, tetA | [62] |
* AMC: amoxicillin/clavulanic acid; AMP: ampicillin; STR: streptomycin; E: erythromycin; ENR: enrofloxacin; E: erythromycin; BE: benzylpenicillin; C: chloramphenicol; CD: clindamycin; CEF: ceftiofur; CEP: cephalothin; CN: gentamicin; CPN: cephalexin; CRO: ceftriaxone; CTX: cefotaxime; DXT: doxycycline; F: nitrofurantoin; IMI: imipenem; INN: cefovecin; KF: cephalothin; MAR: marbofloxacin; NEO: neomycin; PRA: pradofloxacin; PX: cefpodoxime; SXT: trimethoprim/sulfamethoxazole; TE: tetracycline; N: nalidixic acid; CIP: ciprofloxacin; KAN: kanamycin; VAN: vancomycin; Q–D: quinupristin–dalfopristin; CZA: ceftazidime; FEP: cefepime; FOX: cefoxitin: FA: fusidic acid; P: penicillin; T: tobramycin.
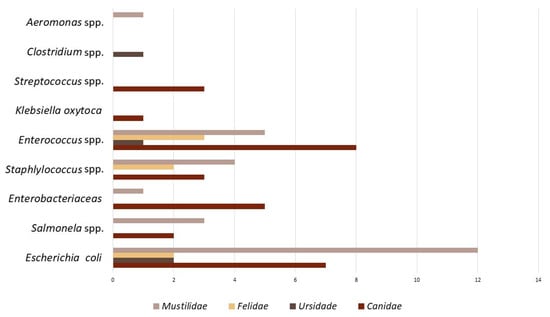 Regarding phenotype resistance, Figure 4 considers the number of articles that describe, in particular, each type of antibiotic resistance reported in the various Carnivora families: Canidae, Ursidae, Felidae, and Mustelidae. The studies are also summarized in Table 2 and Table 3. Many papers report multi-resistant bacteria. The methodology used in these articles was very similar, using the disk diffusion method (DDM) as antibiotic sensitivity testing. All the terminology was also standardized to be included in this graphic.
Regarding phenotype resistance, Figure 4 considers the number of articles that describe, in particular, each type of antibiotic resistance reported in the various Carnivora families: Canidae, Ursidae, Felidae, and Mustelidae. The studies are also summarized in Table 2 and Table 3. Many papers report multi-resistant bacteria. The methodology used in these articles was very similar, using the disk diffusion method (DDM) as antibiotic sensitivity testing. All the terminology was also standardized to be included in this graphic.
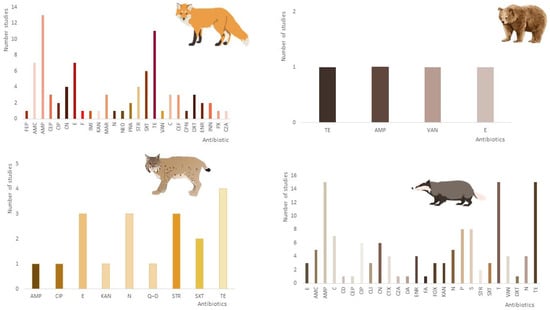 Based on the information collected in the different articles regarding the antibiotic resistance phenotype, it was possible to observe that three of the carnivore families—Canidae, Felidae, and Mustilidae—presented high levels of resistance to ampicillin and tetracyclines (Figure 4). In the case of the Ursidae family, it is impossible to extract any valid information due to the limited number of studies, and the resistance pattern is quite similar.
Based on the information collected in the different articles regarding the antibiotic resistance phenotype, it was possible to observe that three of the carnivore families—Canidae, Felidae, and Mustilidae—presented high levels of resistance to ampicillin and tetracyclines (Figure 4). In the case of the Ursidae family, it is impossible to extract any valid information due to the limited number of studies, and the resistance pattern is quite similar.
3.1. Species and Spatial Distribution
The main families of carnivores where studies were carried out, in descending order, were as follows: 11.1% (n = 4) Ursidae, 16.6% (n = 6) Felidae, 19.4% (n = 7) Canidae, and 52.7% (n = 19) Mustilidae. The species with the most AMR studies was Vulpes vulpes with 12 studies, followed by Lutra lutra with 11 studies. The countries where the studies were carried out, in ascending order, were as follows: 41.6% (n = 15) Portugal, 25% (n = 9) Italy, 8.3% (n = 3) Norway, 8.3% (n = 3) Germany, 8.3% (n = 3) Slovakia, 5.5% (n = 2) Ireland, 5.5% (n = 2) Slovenia, 5.5% (n = 2) Poland, 2.7% (n = 1) Austria, 2.7% (n = 1) Sweden, 2.7% (n = 1) United Kingdom. Figure 2 represents the number of studies by carnivorous species in each country included in this research.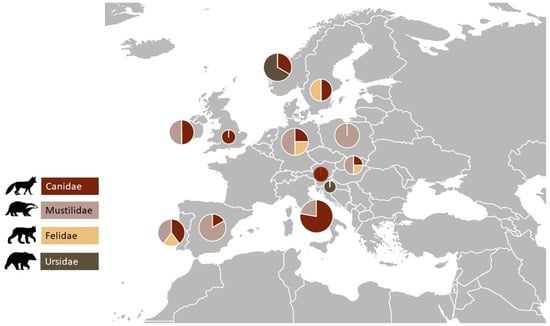
Figure 2.
Distribution of the studies in the different European countries by carnivorous family group.
3.2. Bacteria, Antibiotic Resistance Pattern, and Resistance Genes
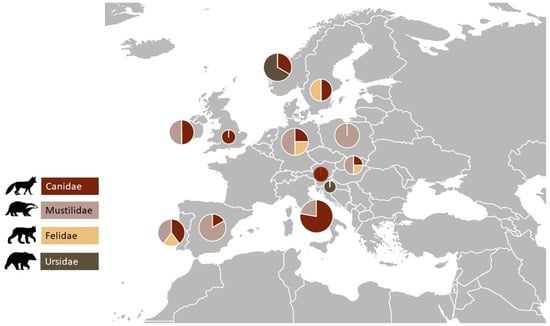
Most of the studies were performed in fecal samples or rectal swabs; therefore, the bacteria isolated mostly were microbiota from the gut microflora (Figure 3).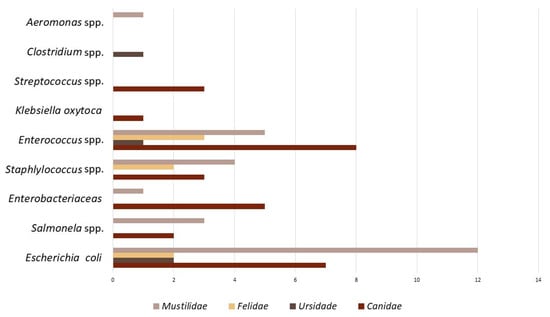
Figure 3.
Bacteria species that predominate in the 36 studies in antibiotic resistance in wild carnivores.
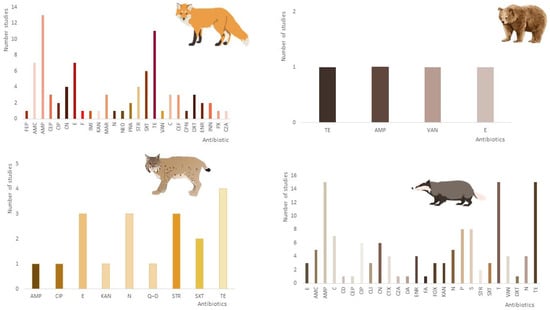
Figure 4. Occurrence of phenotypic antimicrobial resistance profile of bacteria in wild carnivores based on the articles included in this research (AMC: amoxicillin/clavulanic acid; AMP: ampicillin; STR: streptomycin; E: erythromycin; ENR: enrofloxacin; E: erythromycin; BE: benzylpenicillin; C: chloramphenicol; CD: clindamycin; CEF: ceftiofur; CEP: cephalothin; CN: gentamicin; CPN: cephalexin; CRO: ceftriaxone; CTX: cefotaxime; DXT: doxycycline; F: nitrofurantoin; IMI: imipenem; INN: cefovecin; KF: cephalothin; MAR: marbofloxacin; NEO: neomycin; PRA: pradofloxacin; PX: cefpodoxime; SXT: trimethoprim/sulfamethoxazole; TE: tetracycline; N: nalidixic acid; CIP: ciprofloxacin; KAN: kanamycin; VAN: vancomycin; Q–D: quinupristin–dalfopristin; CZA: ceftazidime; FEP: cefepime; FOX: cefoxitin: FA: fusidic acid; P: penicillin; T: tobramycin).
