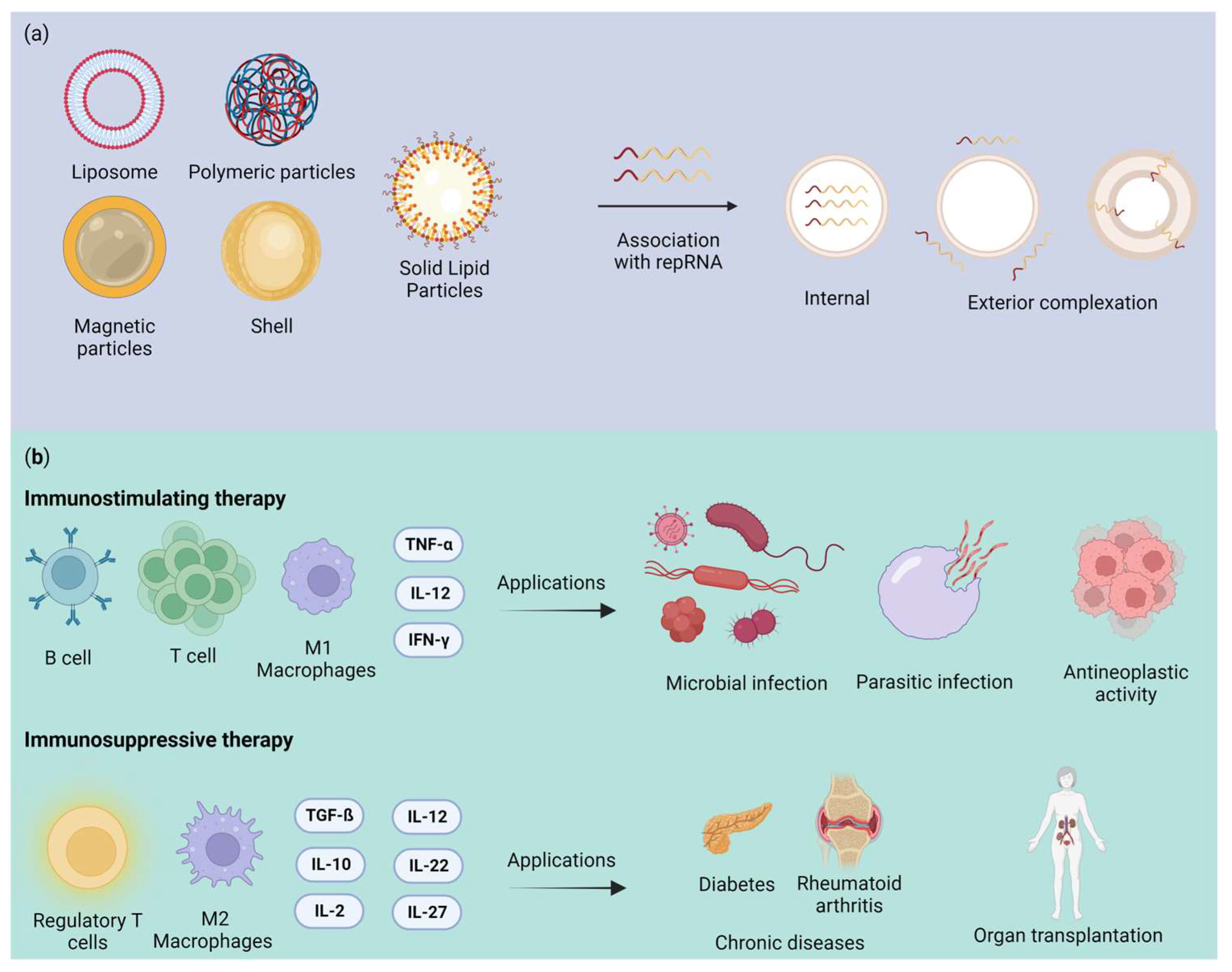
Nucleic acid-based therapies have the potential to address numerous diseases that pose significant challenges to more traditional methods. RNA-based therapies have emerged as a promising avenue, utilizing nanoformulation treatments to target a range of pathologies. Nanoformulation offers several advantages compared to other treatment modalities, including targeted delivery, low toxicity, and bioactivity suitable for drug loading. Various types of nanoformulations are available, such as liposomes, polymeric nanoparticles (NPs), magnetic NPs, nanoshells, and solid lipid nanoparticles (SLNs). RNA-based therapy utilizes intracellular gene nanoparticles with messenger RNA (mRNA) emerging prominently in cancer therapy and immunotechnology against infectious diseases. The approval of mRNA-based technology opens doors for future technological advancements, particularly self-amplifying replicon RNA (repRNA). RepRNA is a novel platform in gene therapy, comprising viral RNA with a unique molecular property that enables the amplification of all encoded genetic information countless times. As a result, repRNA-based therapies have achieved significant levels of gene expression.
- RNA replicon therapy
- RNA replicon vaccines
- self-amplifying RNA
1. Introduction
2. Nanotechnology’s Impact on Healthcare: Advancements, Applications, and RNA Nanotechnology
The prefix “nano”, derived from Greek, signifies something minuscule, measuring as small as less than one-millionth of a meter [17]. This minuscule scale is fundamental to nanotechnology’s core concept. Conversely, technology denotes the systematic study of processes within a specific domain [18]. However, nanotechnology takes this a step further. Following this initial definition, nanotechnology is regarded as a scientific discipline dedicated to comprehending matter at nanometric scales, typically ranging from 1 to 100 nanometers, with the aim of precise control and manipulation to usher in technological advancements across diverse domains [19]. Our civilization has greatly benefited from nanotechnology, which has made significant contributions to numerous prominent industries [20]. Among these industries, over the past two decades, nanotechnology’s advancement in the medical and healthcare sectors have played a crucial role in preventing, diagnosing, and treating various illnesses [20]. Within the realm of healthcare, the application of nanotechnology is termed “nanomedicine,” a field that has yielded a profound understanding of cellular mechanisms in living organisms [21]. This profound understanding has paved the way for various applications encompassing pharmaceutical therapy and the prevention, diagnosis, monitoring, and treatment of many diseases [22]. The implications of nanotechnology in scientific research are highly promising, transcending the limitations of conventional therapies by enhancing the mechanisms employed, particularly in safeguarding the desired drug [21]. To achieve these advancements, nanotechnology employs top-down and bottom-up assembly methods to create and utilize materials at the nanometer scale. Notably, DNA, RNA, and protein macromolecules possess inherent properties at the nanoscale, making them promising building blocks for the bottom-up construction of nanostructures and nanodevices [15]. Research into the folding and structure of RNA has a long history. However, it is important to note that RNA nanotechnology distinguishes itself from conventional RNA structure and folding studies [23]. RNA nanotechnology is the study of RNA-based structures with a primary framework at the nanoscale [24]. This unique focus necessitates a comprehensive understanding of not only intramolecular interactions and folding but also intermolecular interactions. A crucial aspect of RNA nanotechnology involves characterizing the physical, chemical, biological, and pharmacological properties of nanoparticles that researchers can homogenize through purification [23]. An important milestone in the field was the assembly of RNA dimer, trimer, and hexamer nanoparticles using reengineered RNA fragments derived from pRNA (packaging RNA), a vital component responsible for driving the DNA packaging motor in bacteriophage phi29 [25]. RNA nanotechnology, as opposed to conventional RNA biology research, focuses on using the characteristics of RNA to create structures for use in nanomedicine [24]. This approach is particularly promising for therapeutic applications, where nanoformulations offer synergistic actions and efficient delivery systems, notably in the treatment of diverse cancer types [26]. Beyond medicinal technology, a range of industrial sectors, including electronics, environmental science, food production, and textiles, have expressed keen interest in nanotechnology due to its potential to enhance product quality, safety, and durability [22].2.1. Nanoformulation
Researchers engineer nanoformulations to optimize drug delivery, increase drug solubility, improve bioavailability, and enable targeted drug release, thereby enhancing the overall efficacy and safety of pharmaceuticals [26]. In terms of therapeutic effectiveness, researchers have observed that nanoparticles exhibit optimal internalization by cancer cells, especially in the treatment of diseases like breast cancer [27]. Their enhanced permeation into the target cells not only improves drug delivery, but also renders the nanoformulation more cytotoxic when compared to free drugs [28]. These nanodelivery technologies can also apply to phytocompounds. Various phytocompounds, including cannabidiol (CBD), have received attention for delivery using nanocarriers as a viable platform, with the aim of restricting the variety of negative consequences [29]. Nanodelivery technologies have improved the stability of phytocompounds, enhanced their absorption, shielded them from early enzymatic depletion or metabolism within the body, and prolonged their circulation duration [29]. Therefore, the significance of this technology lies in advancing the treatment of various diseases and offering expanded therapeutic possibilities [30]. Furthermore, its economic advantages are compelling, as it allows for easy industrial scale-up, making it a practical choice in this sector. These innovative nanoformulations hold the potential to revolutionize drug delivery and substantially improve patient outcomes across a wide range of medical conditions. With this in mind, Table 1 shows some nanoformulations and their main components that have already been approved for therapeutic use by regulatory agencies such as the FDA.|
Classification |
Name (Trade Tame) |
Main Component |
Delivery Route |
Indication |
Approval (Year) |
|---|---|---|---|---|---|
|
Liposome |
AmBisome |
Liposomal amphotericin B |
Intravenous |
Fungal/protozoal infections |
FDA (1997) EMA (2006) ANVISA (1997) |
|
Doxil/ Caelyx |
Liposomal doxorubicin |
Intravenous |
Antineoplastic agents (ovarian and breast cancer; multiple myeloma; Karposi’s Sarcoma) |
FDA (1995, 2005, 2008) EMA (1996) ANVISA (2011) |
|
|
Myocet (Myoce liposomal) |
Liposomal doxorubicin |
Intravenous |
Antineoplastic agents (breast neoplasms) |
FDA (2000) EMA (2000) |
|
|
Visudyne |
Liposomal verteporfin |
Intravenous |
Ophthalmic agents (myopia; ocular histoplasmosis; macular degeneration, wet age-related) |
FDA (2000) ANVISA (2004) EMA (2007) |
|
|
Marqibo |
Liposomal vincristine |
Intravenous |
Antineoplastic agents (hematologic malignancies and solid tumors) |
FDA (2012) |
|
|
Onivyde (Onivyde pegylated liposomal) |
Liposomal irinotecan |
Intravenous |
Antineoplastic agents (pancreatic cancer) |
FDA (2015) EMA (2016) |
|
|
Polymer-based nanoparticles |
Eligard |
Leuprolide acetate and polymer (PLGH (poly (DL-Lactide-co-glycolide))) |
Subcutaneous |
Antineoplastic agents (prostate cancer) |
FDA (2002) ANVISA (2006) |
|
Mircera |
Methoxy polyethylene glycol-epoetin beta |
Subcutaneous/ Intravenous |
Anemia associated with chronic kidney disease |
FDA (2007) EMA (2007) ANVISA (2008) |
|
|
Cimzia |
PEGylated antibody fragment (Certolizumab) |
Subcutaneous |
Anti-inflammatory action (Crohn’s disease; rheumatoid arthritis; psoriatic arthritis; ankylosing spondylitis) |
FDA (2008, 2009, 2013) EMA (2009) ANVISA (2017) |
|
|
PegIntron |
PEGylated IFN alpha-2b protein |
Subcutaneous |
Immunomodulator (hepatitis C) |
FDA (2001) EMA (2000) ANVISA (2011) |
|
|
Magnetic nanoparticles |
NanoTherm |
Iron oxide coated with amino silane |
Intratumoral injection |
Antineoplastic agents (glioblastoma) |
FDA (2010) EMA (2013) |
|
Feraheme |
Iron oxide and a polyglucose sorbitol carboxymethyether |
Intravenous |
Treatment of anemia |
FDA (2009) EMA (2012) |
|
|
Lipid nanoparticle |
Patisiran (Onpattro) |
Phospholipids, cholesterol, ionizable cationic lipid (DLin-MC3-DMA), and polyethylene glycol-modified lipid |
Intravenous |
Polyneuropathy |
FDA (2018) |
2.2. Nanotoxicology Challenges and Opportunities
3. Virus-Based Delivery System
4. Advantages and Challenges of Replicon RNA Therapy
|
Carrier |
RNA Replicon |
Results |
Reference |
|---|---|---|---|
|
Cationic nanocarrier |
RepRNA PMIF (macrophage migration inhibitory factor and cytokine). |
It improved host cellular and humoral immunity against Plasmodium infection in the liver and blood and conferred complete protection against malaria reinfection in murine mice. |
|
|
Nanostructured lipid transporters (NLCs) |
RepRNA ZIKV-117 mAb. |
Rapid protection against Zika virus infection in mice. |
|
|
Lipid InOrganic Nanoparticles (LION) |
LION/repRNA-CoV2S |
LION/repRNA-CoV2S vaccine intramuscularly to mice, a significant amount of anti-SARS-CoV-2 S protein IgG antibody isotypes, resembling a Type 1 T helper cell response, were produced. |
|
|
Cationic nanocarrier |
RepRNA CCHFV (Crimean–Congo hemorrhagic fever virus) encoding NP (nucleoprotein), GPC (glycoprotein precursor) or both |
It provided robust protection against Crimean–Congo hemorrhagic fever virus in lethal mice. |
|
|
Cationic liposomes |
samPfRH5 replicon (Plasmodium falciparum reticulocyte binding protein homologue 5) |
The liposome–replicon complexes showed high transfection efficiencies. They elicited antibodies capable of inhibiting the growth of the parasite in vitro |
|
|
Mannosylation of lipid nanoparticles (LNPs) |
Self-amplifying mRNA encoded an influenza (hemagglutinin) |
Compared to LNPs, mannnosylated lipid nanoparticles (MLNPs) showed higher levels of IgG1 and IgG2a. |
|
|
Polymeric nanoparticle |
Nanoparticle (MDNP)-delivered VEEV replicon RNA encoding the hemagglutinin protein (HA) of an H1N1 influenza virus (A/WSN/33) or the Ebola virus (EBOV) glycoprotein (GP) |
The vaccine elicits both CD8+ T-cell and antibody responses and can be created with numerous antigen-expressing replicons. |
References
- Lundstrom, K. Nanoparticle-Based Delivery of Self-Amplifying RNA. Gene Ther. 2020, 27, 183–185.
- Sergeeva, O.V.; Koteliansky, V.E.; Zatsepin, T.S. MRNA-Based Therapeutics–Advances and Perspectives. Biochemistry 2016, 81, 709–722.
- Guo, P.; Haque, F.; Hallahan, B.; Reif, R.; Li, H. Uniqueness, Advantages, Challenges, Solutions, and Perspectives in Therapeutics Applying RNA Nanotechnology. Nucleic Acid. Ther. 2012, 22, 226–245.
- Tenchov, R.; Bird, R.; Curtze, A.E.; Zhou, Q. Lipid Nanoparticles from Liposomes to MRNA Vaccine Delivery, a Landscape of Research Diversity and Advancement. ACS Nano 2021, 15, 16982–17015.
- Beck, J.D.; Reidenbach, D.; Salomon, N.; Sahin, U.; Türeci, Ö.; Vormehr, M.; Kranz, L.M. MRNA Therapeutics in Cancer Immunotherapy. Mol. Cancer 2021, 20, 69.
- Sahin, U.; Karikó, K.; Türeci, Ö. MRNA-Based Therapeutics-Developing a New Class of Drugs. Nat. Rev. Drug Discov. 2014, 13, 759–780.
- Démoulins, T.; Englezou, P.C.; Milona, P.; Ruggli, N.; Tirelli, N.; Pichon, C.; Sapet, C.; Ebensen, T.; Guzmán, C.A.; McCullough, K.C. Self-Replicating RNA Vaccine Delivery to Dendritic Cells. In Methods in Molecular Biology; Humana Press Inc.: Totowa, NJ, USA, 2017; Volume 1499, pp. 37–75.
- Lin, G.; Yan, H.; Sun, J.; Zhao, J.; Zhang, Y. Self-Replicating RNA Nanoparticle Vaccine Elicits Protective Immune Responses against SARS-CoV-2. Mol. Ther. Nucleic Acids 2023, 32, 650–666.
- Lundstrom, K. Self-Replicating RNA Viruses for RNA Therapeutics. Molecules 2018, 23, 3310.
- Nakamura, A.; Kotaki, T.; Nagai, Y.; Takazawa, S.; Tokunaga, K.; Kameoka, M. Construction and Evaluation of a Self-Replicative RNA Vaccine against SARS-CoV-2 Using Yellow Fever Virus Replicon. PLoS ONE 2022, 17, e0274829.
- Dana, H.; Mahmoodi Chalbatani, G.; Mahmoodzadeh, H.; Karimloo, R.; Rezaiean, O.; Moradzadeh, A.; Mehmandoost, N.; Moazzen, F.; Mazraeh, A.; Marmari, V.; et al. Molecular Mechanisms and Biological Functions of SiRNA. Int. J. Biomed. Sci. IJBS 2017, 13, 48–57.
- Alshaer, W.; Zureigat, H.; Al Karaki, A.; Al-Kadash, A.; Gharaibeh, L.; Hatmal, M.M.; Aljabali, A.A.A.; Awidi, A. SiRNA: Mechanism of Action, Challenges, and Therapeutic Approaches. Eur. J. Pharmacol. 2021, 905, 174178.
- Yu, B.; Tai, H.C.; Xue, W.; Lee, L.J.; Lee, R.J. Receptor-Targeted Nanocarriers for Therapeutic Delivery to Cancer. Mol. Membr. Biol. 2010, 27, 286–298.
- Friedrich, M.; Aigner, A. Therapeutic SiRNA: State-of-the-Art and Future Perspectives. BioDrugs 2022, 36, 549–571.
- Shu, Y.; Pi, F.; Sharma, A.; Rajabi, M.; Haque, F.; Shu, D.; Leggas, M.; Evers, B.M.; Guo, P. Stable RNA Nanoparticles as Potential New Generation Drugs for Cancer Therapy. Adv. Drug Deliv. Rev. 2014, 66, 74–89.
- Li, M.; Li, Y.; Li, S.; Jia, L.; Wang, H.; Li, M.; Deng, J.; Zhu, A.; Ma, L.; Li, W.; et al. The Nano Delivery Systems and Applications of MRNA. Eur. J. Med. Chem. 2022, 227, 113910.
- Antunes Filho, S.; Backx, B.P. Nanotecnologia e Seus Impactos Na Sociedade. Rev. Tecnol. Soc. 2020, 16, 1–15.
- Bayda, S.; Adeel, M.; Tuccinardi, T.; Cordani, M.; Rizzolio, F. The History of Nanoscience and Nanotechnology: From Chemical-Physical Applications to Nanomedicine. Molecules 2020, 25, 112.
- Fialkoski, D.; Malfatti, C.R.M. Nanotecnologia: Uma Prospecção Tecnológica No Âmbito Nacional e Internacional. Cad. Prospecção 2019, 12, 590.
- Nunes, A.R.; Costa, E.C.; Alves, G.; Silva, L.R. Nanoformulations for the Delivery of Dietary Anthocyanins for the Prevention and Treatment of Diabetes Mellitus and Its Complications. Pharmaceuticals 2023, 16, 736.
- Chakravarty, M.; Vora, A. Nanotechnology-Based Antiviral Therapeutics. Drug Deliv. Transl. Res. 2021, 11, 748–787.
- Cui, F.; Liu, J.; Pang, S.; Li, B. Recent Advance in Tumor Microenvironment-Based Stimuli-Responsive Nanoscale Drug Delivery and Imaging Platform. Front. Pharmacol. 2022, 13, 929854.
- Guo, P. The Emerging Field of RNA Nanotechnology. Nat. Nanotechnol. 2010, 5, 833–842.
- Jasinski, D.; Haque, F.; Binzel, D.W.; Guo, P. Advancement of the Emerging Field of RNA Nanotechnology. ACS Nano 2017, 11, 1142–1164.
- Guo, P.; Zhang, C.; Chen, C.; Garver, K.; Trottier, M. Inter-RNA Interaction of Phage Φ29 PRNA to form a Hexameric Complex for Viral DNA Transportation. Mol. Cell 1998, 2, 149–155.
- Zafar, A.; Alruwaili, N.K.; Imam, S.S.; Alharbi, K.S.; Afzal, M.; Alotaibi, N.H.; Yasir, M.; Elmowafy, M.; Alshehri, S. Novel Nanotechnology Approaches for Diagnosis and Therapy of Breast, Ovarian and Cervical Cancer in Female: A Review. J. Drug Deliv. Sci. Technol. 2021, 61, 102198.
- Maji, R.; Dey, N.S.; Satapathy, B.S.; Mukherjee, B.; Mondal, S. Preparation and Characterization of Tamoxifen Citrate Loaded Nanoparticles for Breast Cancer Therapy. Int. J. Nanomed. 2015, 9, 3107–3118.
- Carvalho Lopes, J.; Pereira Torres, M.L. Utilização de Nanopartículas No Tratamento Do Câncer: Aspectos Gerais, Mecanismos de Ação Antineoplásicos e Aplicabilidades Tumorais. Rev. Bras. Cancerol. 2020, 65, e-13400.
- Assadpour, E.; Rezaei, A.; Das, S.S.; Krishna Rao, B.V.; Singh, S.K.; Kharazmi, M.S.; Jha, N.K.; Jha, S.K.; Prieto, M.A.; Jafari, S.M. Cannabidiol-Loaded Nanocarriers and Their Therapeutic Applications. Pharmaceuticals 2023, 16, 487.
- Lashkari, A.; Ranjbar, R. Nanoparticles and Nanoformulated Drugs as Promising Delivery System in Treatment of Microbial-Induced CNS Infection: A Systematic Review of Literature. J. Neurovirol. 2021, 27, 542–549.
- Lopalco, A.; Denora, N. Nanoformulations for Drug Delivery: Safety, Toxicity, and Efficacy. In Methods in Molecular Biology; Humana Press Inc.: Totowa, NJ, USA, 2018; Volume 1800, pp. 347–365.
- Sharma, S.; Parveen, R.; Chatterji, B.P. Toxicology of Nanoparticles in Drug Delivery. Curr. Pathobiol. Rep. 2021, 9, 133–144.
- Huang, H.J.; Lee, Y.H.; Hsu, Y.H.; Liao, C.T.; Lin, Y.F.; Chiu, H.W. Current Strategies in Assessment of Nanotoxicity: Alternatives to in Vivo Animal Testing. Int. J. Mol. Sci. 2021, 22, 4216.
- Savage, D.T.; Hilt, J.Z.; Dziubla, T.D. In Vitro Methods for Assessing Nanoparticle Toxicity. In Methods in Molecular Biology; Humana Press Inc.: Totowa, NJ, USA, 2019; Volume 1894, pp. 1–29.
- Chenthamara, D.; Subramaniam, S.; Ramakrishnan, S.G.; Krishnaswamy, S.; Essa, M.M.; Lin, F.H.; Qoronfleh, M.W. Therapeutic Efficacy of Nanoparticles and Routes of Administration. Biomater. Res. 2019, 23, 20.
- Gupta, R.; Xie, H. Nanoparticles in Daily Life: Applications, Toxicity and Regulations. J. Environ. Pathol. Toxicol. Oncol. 2018, 37, 209–230.
- Elsaesser, A.; Howard, C.V. Toxicology of Nanoparticles. Adv. Drug Deliv. Rev. 2012, 64, 129–137.
- Sung, Y.K.; Kim, S.W. Recent Advances in the Development of Gene Delivery Systems. Biomater. Res. 2019, 23, 8.
- Eshka, S.F.A.; Bahador, M.; Gordan, M.M.; Karbasi, S.; Tabar, Z.M.; Basiri, M. A Systematic Review of Gene Editing Clinical Trials. medRxiv 2022.
- Kontogiannis, O.; Karalis, V. On the in Vivo Kinetics of Gene Delivery Vectors. medRxiv 2022.
- Nayerossadat, N.; Ali, P.; Maedeh, T. Viral and Nonviral Delivery Systems for Gene Delivery. Adv. Biomed. Res. 2012, 1, 27.
- Wang, D.; Tai, P.W.L.; Gao, G. Adeno-Associated Virus Vector as a Platform for Gene Therapy Delivery. Nat. Rev. Drug Discov. 2019, 18, 358–378.
- Abinaya, R.V.; Viswanathan, P. Biotechnology-Based Therapeutics. In Translational Biotechnology; Elsevier: Amsterdam, The Netherlands, 2021; pp. 27–52.
- Trobridge, G.D. Foamy Virus Vectors for Gene Transfer. Expert. Opin. Biol. Ther. 2009, 9, 1427–1436.
- Deregowski, V.; Canalis, E. Gene Delivery by Retroviruses. In Osteoporosis. Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2008; Volume 455.
- Cavalieri, V.; Baiamonte, E.; Lo Iacono, M. Non-Primate Lentiviral Vectors and Their Applications in Gene Therapy for Ocular Disorders. Viruses 2018, 10, 316.
- Worgall, S.; Crystal, R.G. Gene Therapy. In Principles of Tissue Engineerin, 4th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2013; pp. 657–686. ISBN 9780123983589.
- Wong, L.-F.; Goodhead, L.; Kyriacos, C.P.; Mitrophanous, K.A.; Kingsman, S.M.; Mazarakis, N.D. Lentivirus-Mediated Gene Transfer to the Central Nervous: Therapeutic and Research Applications. Hum. Gene Ther. 2006, 17, 1–9.
- Lee, C.S.; Bishop, E.S.; Zhang, R.; Yu, X.; Farina, E.M.; Yan, S.; Zhao, C.; Zeng, Z.; Shu, Y.; Wu, X.; et al. Adenovirus-Mediated Gene Delivery: Potential Applications for Gene and Cell-Based Therapies in the New Era of Personalized Medicine. Genes. Dis. 2017, 4, 43–63.
- Kasala, D.; Yoon, A.R.; Hong, J.; Kim, S.W.; Yun, C.O. Evolving Lessons on Nanomaterial-Coated Viral Vectors for Local and Systemic Gene Therapy. Nanomedicine 2016, 11, 1689–1713.
- Ahmadi, S.E.; Soleymani, M.; Shahriyary, F.; Amirzargar, M.R.; Ofoghi, M.; Fattahi, M.D.; Safa, M. Viral Vectors and Extracellular Vesicles: Innate Delivery Systems Utilized in CRISPR/Cas-Mediated Cancer Therapy. Cancer Gene Ther. 2023, 30, 936–954.
- Zhang, H.; Wang, H.; An, Y.; Chen, Z. Construction and Application of Adenoviral Vectors. Mol. Ther. Nucleic Acids 2023, 34, 102027.
- Vargas, J.E.; Chicaybam, L.; Stein, R.T.; Tanuri, A.; Delgado-Cañedo, A.; Bonamino, M.H. Retroviral Vectors and Transposons for Stable Gene Therapy: Advances, Current Challenges and Perspectives. J. Transl. Med. 2016, 14, 288.
- Capasso, C.; Garofalo, M.; Hirvinen, M.; Cerullo, V. The Evolution of Adenoviral Vectors through Genetic and Chemical Surface Modifications. Viruses 2014, 6, 832–855.
- Vandendriessche, T.; Naldini, L.; Collen, D.; Chuah, M.K.L. Oncoretroviral and Lentiviral Vector-Mediated Gene Therapy. Methods Enzym. 2002, 346, 573–589.
- Cevher, E.; Demir, A.; Sefik, E. Gene Delivery Systems: Recent Progress in Viral and Non-Viral Therapy. In Recent Advances in Novel Drug Carrier Systems; InTech: London, UK, 2012.
- Travieso, T.; Li, J.; Mahesh, S.; Mello, J.D.F.R.E.; Blasi, M. The Use of Viral Vectors in Vaccine Development. NPJ Vaccines 2022, 7, 75.
- Minnaert, A.K.; Vanluchene, H.; Verbeke, R.; Lentacker, I.; De Smedt, S.C.; Raemdonck, K.; Sanders, N.N.; Remaut, K. Strategies for Controlling the Innate Immune Activity of Conventional and Self-Amplifying MRNA Therapeutics: Getting the Message Across. Adv. Drug Deliv. Rev. 2021, 176, 113900.
- Maruggi, G.; Zhang, C.; Li, J.; Ulmer, J.B.; Yu, D. MRNA as a Transformative Technology for Vaccine Development to Control Infectious Diseases. Mol. Ther. 2019, 27, 757–772.
- Ballesteros-Briones, M.C.; Silva-Pilipich, N.; Herrador-Cañete, G.; Vanrell, L.; Smerdou, C. A New Generation of Vaccines Based on Alphavirus Self-Amplifying RNA. Curr. Opin. Virol. 2020, 44, 145–153.
- Blom, D.J.; Marais, A.D.; Moodley, R.; van der Merwe, N.; van Tonder, A.; Raal, F.J. RNA-Based Therapy in the Management of Lipid Disorders: A Review. Lipids Health Dis. 2022, 21, 41.
- Magadum, A.; Kaur, K.; Zangi, L. MRNA-Based Protein Replacement Therapy for the Heart. Mol. Ther. 2019, 27, 785–793.
- Erasmus, J.H.; Khandhar, A.P.; O’Connor, M.A.; Walls, A.C.; Hemann, E.A.; Murapa, P.; Archer, J.; Leventhal, S.; Fuller, J.T.; Lewis, T.B.; et al. An Alphavirus-Derived Replicon RNA Vaccine Induces SARS-CoV-2 Neutralizing Antibody and T Cell Responses in Mice and Nonhuman Primates. Sci. Transl. Med. 2020, 12, eabc9396.
- McCullough, K.C.; Bassi, I.; Milona, P.; Suter, R.; Thomann-Harwood, L.; Englezou, P.; Démoulins, T.; Ruggli, N. Self-Replicating Replicon-Rna Delivery to Dendritic Cells by Chitosan-Nanoparticles for Translation in Vitro and in Vivo. Mol. Ther. Nucleic Acids 2014, 3, e173.
- Blakney, A.K.; McKay, P.F.; Yus, B.I.; Aldon, Y.; Shattock, R.J. Inside out: Optimization of Lipid Nanoparticle Formulations for Exterior Complexation and in Vivo Delivery of SaRNA. Gene Ther. 2019, 26, 363–372.
- Feng, X.; Xu, W.; Li, Z.; Song, W.; Ding, J.; Chen, X. Immunomodulatory Nanosystems. Adv. Sci. 2019, 6, 1900101.
- Machado, B.A.S.; Hodel, K.V.S.; Fonseca, L.M.D.S.; Mascarenhas, L.A.B.; Andrade, L.P.C.d.S.; Rocha, V.P.C.; Soares, M.B.P.; Berglund, P.; Duthie, M.S.; Reed, S.G.; et al. The Importance of Rna-Based Vaccines in the Fight against COVID-19: An Overview. Vaccines 2021, 9, 1345.
- Wadhwa, A.; Aljabbari, A.; Lokras, A.; Foged, C.; Thakur, A. Opportunities and Challenges in the Delivery of Mrna-Based Vaccines. Pharmaceutics 2020, 12, 102.
- Cullis, P.R.; Hope, M.J. Lipid Nanoparticle Systems for Enabling Gene Therapies. Mol. Ther. 2017, 25, 1467–1475.
- Kowalski, P.S.; Rudra, A.; Miao, L.; Anderson, D.G. Delivering the Messenger: Advances in Technologies for Therapeutic MRNA Delivery. Mol. Ther. 2019, 27, 710–728.
- Garcia, A.B.; Siu, E.; Sun, T.; Exler, V.; Brito, L.; Hekele, A.; Otten, G.; Augustijn, K.; Janse, C.J.; Ulmer, J.B.; et al. Neutralization of the Plasmodium-Encoded MIF Ortholog Confers Protective Immunity against Malaria Infection. Nat. Commun. 2018, 9, 2714.
- Erasmus, J.H.; Archer, J.; Fuerte-Stone, J.; Khandhar, A.P.; Voigt, E.; Granger, B.; Bombardi, R.G.; Govero, J.; Tan, Q.; Durnell, L.A.; et al. Intramuscular Delivery of Replicon RNA Encoding ZIKV-117 Human Monoclonal Antibody Protects against Zika Virus Infection. Mol. Ther. Methods Clin. Dev. 2020, 18, 402–414.
- Leventhal, S.S.; Meade-White, K.; Rao, D.; Haddock, E.; Leung, J.; Scott, D.; Archer, J.; Randall, S.; Erasmus, J.H.; Feldmann, H.; et al. Replicating RNA Vaccination Elicits an Unexpected Immune Response That Efficiently Protects Mice against Lethal Crimean-Congo Hemorrhagic Fever Virus Challenge. Lancet 2022, 82, 104188.
- Fotoran, W.L.; da Silva, J.R.; Glitz, C.; Ferreira, L.C.d.S.; Wunderlich, G. Establishment of an Antiplasmodial Vaccine Based on PfRH5-Encoding RNA Replicons Stabilized by Cationic Liposomes. Pharmaceutics 2023, 15, 1223.
- Goswami, R.; O’hagan, D.T.; Adamo, R.; Baudner, B.C. Conjugation of Mannans to Enhance the Potency of Liposome Nanoparticles for the Delivery of Rna Vaccines. Pharmaceutics 2021, 13, 240.
- Chahal, J.S.; Khan, O.F.; Cooper, C.L.; McPartlan, J.S.; Tsosie, J.K.; Tilley, L.D.; Sidik, S.M.; Lourido, S.; Langer, R.; Bavari, S.; et al. Dendrimer-RNA Nanoparticles Generate Protective Immunity against Lethal Ebola, H1N1 Influenza, and Toxoplasma Gondii Challenges with a Single Dose. Proc. Natl. Acad. Sci. USA 2016, 113, E4133–E4142.
- McCullough, K.C.; Milona, P.; Thomann-Harwood, L.; Démoulins, T.; Englezou, P.; Suter, R.; Ruggli, N. Self-Amplifying Replicon RNA Vaccine Delivery to Dendritic Cells by Synthetic Nanoparticles. Vaccines 2014, 2, 735–754.
- Brito, L.A.; Chan, M.; Shaw, C.A.; Hekele, A.; Carsillo, T.; Schaefer, M.; Archer, J.; Seubert, A.; Otten, G.R.; Beard, C.W.; et al. A Cationic Nanoemulsion for the Delivery of Next-Generation RNA Vaccines. Mol. Ther. 2014, 22, 2118–2129.
- Erasmus, J.H.; Khandhar, A.P.; Guderian, J.; Granger, B.; Archer, J.; Archer, M.; Gage, E.; Fuerte-Stone, J.; Larson, E.; Lin, S.; et al. A Nanostructured Lipid Carrier for Delivery of a Replicating Viral RNA Provides Single, Low-Dose Protection against Zika. Mol. Ther. 2018, 26, 2507–2522.
