Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Vladislav Volarevic and Version 2 by Rita Xu.
Dry eye disease (DED) is a multifactorial disorder of the lacrimal system and ocular surface, characterized by a deficiency in the quality and/or quantity of the tear fluid. The multifactorial nature of DED encompasses a number of interconnected underlying pathologies, including loss of homeostasis, instability and hyperosmolarity of the tears, and the induction and propagation of detrimental inflammatory responses in the eyes, which finally results in the development of neurosensory dysfunction and visual disruption.
- tear hyperosmolarity
- dry eye disease
- corneal epithelial cells
1. Introduction
Dry eye disease (DED), also known as keratoconjunctivitis sicca or dysfunctional tear syndrome, is a widespread, multifactorial disorder of the lacrimal system and ocular surface, characterized by a deficiency in the quality and/or quantity of the tear fluid [1].
The ocular surface is highly exposed to environmental threats, which are efficiently eliminated by the tears [2]. Accordingly, an efficient generation and adequate turnover of tears is crucially important for proper eye function [2]. The lacrimal functional unit (LFU) is composed of the lacrimal and meibomian glands, mucin-producing goblet cells, ocular surface secretory cells, lacrimal outflow pathways, and corneal and conjunctival epithelial cells [3]. All components of the LFU work together to maintain the tear film, protect the transparency of the cornea, and preserve the integrity of the ocular surface [3]. It is important to note that the LFU interacts with the neurological and endocrine systems and is not a standalone system. Destabilizing the tear film will result in the development of DED if any LFU component is damaged, as well as if neural and endocrine disorders (such as sensory and motor nerve dysfunction, or hormonal imbalance) arise [3]. An unbalanced tear film’s inability to appropriately nourish or protect the ocular surface results in permanent damage to the corneal and conjunctival epithelial cells and corneal nerve fibers [1][3][1,3].
There are two main subtypes of DED: evaporative dry eye (EDE), which is typically attributable to excessive evaporation of the tear fluid; and aqueous tear-deficient dry eye (ADDE), which is characterized by inefficiency or failure of the lacrimal glands to generate tears [4]. While the cause of ADDE may be autoimmune or related to a breach in the integrity of the LFU, EDE usually develops due to meibomian gland dysfunction (MGD) [4]. In clinical settings, DED is frequently observed as a “hybrid” or “mixed” version of these two subtypes, wherein each subtype acquires some of the clinical traits of the other, initiating and aggravating its pathology [4].
The multifactorial nature of DED encompasses a number of interconnected underlying pathologies, including a loss of homeostasis, instability and hyperosmolarity of the tears, and the induction and propagation of detrimental inflammatory responses in the eyes, which finally results in the development of neurosensory dysfunction and visual disruption [1][5][1,5]. These detrimental events create a “pathological loop” that promotes the development and exacerbation of DED (Figure 1) [1].
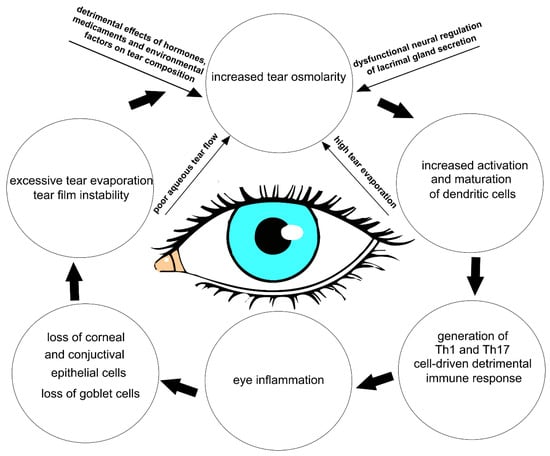
Figure 1. Crucial factors contributing to the development of THO and DED. Hormones, medicaments, environmental factors, dysfunctional neural regulation of lacrimal gland secretion, poor aqueous tear flow, and excessive tear evaporation result in the development of THO. THO induces increased activation and maturation of dendritic cells, which generates a detrimental Th1 and Th17 cell-driven immune response in the eyes of DED patients. Through the production of inflammatory cytokines, Th1 and Th17 cells induce inflammation, which causes injury to the epithelial and goblet cells in the eyes of DED patients. The loss of goblet, corneal, and conjunctival epithelial cells results in excessive tear evaporation and tear film instability, which crucially contribute to the development of THO and DED.
Dryness, grittiness, scratchiness, discomfort, inflammation, burning, watering, a feeling of a foreign substance in the eye, ocular fatigue, pain, and decreased functional visual acuity are all common symptoms of DED [5][6][5,6]. Eye dysfunction drastically attenuates patients’ quality of life and impairs patients’ abilities to do daily tasks that depend on their vision.
Long-term symptom relief is currently the main therapeutic goal of DED treatment, along with reestablishing the natural equilibrium on the surface of the eye [7]. Accordingly, tear replacement medications are increasingly offered to DED patients in order to attenuate dry eye-related symptoms [8]. However, the complex etiology of DED necessitates a more comprehensive therapeutic approach that can interfere with the intracellular signaling pathways, which are responsible for the development of pathological changes in the eyes of DED patients [6][7][6,7]. Therefore, a better understanding of the pathophysiological processes that regulate the development and progression of DED is crucially important for the establishment of new and more effective DED-related treatment approaches, which would significantly improve the quality of life of DED patients [1][6][1,6].
2. The Impacts of Dysfunctional Neural Regulation of Lacrimal Gland Secretion on the Development of THO and DED Progression
Dysfunction in the neural control of glandular tear secretion plays a significant role in the development of THO and DED progression [9][18]. When sensory neurons in the cornea and conjunctiva detect changes in osmolarity, they transmit signals to the lacrimal glands, initiating tear secretion [9][18]. A large number of experimental and clinical studies have demonstrated that transient receptor potential (TRP) channels are mainly responsible for the neural regulation of tear production [9][10][11][12][13][14][15][16][17][18][19][18,19,20,21,22,23,24,25,26,27,28]. TRP channels belong to a heterogeneous superfamily of widely expressed, functionally varied cation channels that display intricate regulation patterns and are sensitive to a variety of stimuli, including THO [14][15][23,24]. Among various TRP channels, the transient receptor potential melastatin 8 (TRPM8) and transient receptor potential vanilloid 1 (TRPV1) are dominantly expressed in sensory neurons of the cornea and conjunctiva [13][14][15][22,23,24]. TRP channels are essential for normal neuronal functioning and play a crucial role in sensory perception, neuronal excitability, and synaptic transmission [16][25]. The activation of TRP channels in presynaptic terminals can modulate the release of neurotransmitters, affecting synaptic transmission and neuronal communication [16][25]. It should be emphasized that TRP channels are also expressed in non-neuronal corneal cells and in all three layers of the cornea [16][25]. These channels are essential for maintaining the health and functionality of the cornea, contributing to clear vision and overall ocular well-being. In addition to sensory transduction, TRP channels are involved in maintaining corneal integrity and promoting the repair and regeneration of injured tissue [16][25]. TRP channels affect the proliferation, differentiation, and migration of corneal epithelial and stromal cells, enabling remodeling of the extracellular matrix and wound healing [15][16][24,25]. Furthermore, TRP channels, particularly TRPM8 and TRPV4, are involved in regulating tear secretion and osmolarity. Activation of these TRP channels can stimulate tear production and maintain a stable tear film, preventing dry eye conditions [16][25]. In addition to sensory transduction, TRP channels play a crucial role in the regulation of corneal integrity, wound healing, and tear film homeostasis [13][14][15][16][22,23,24,25]. Although there are distinctly different functions of TRP channels between neuronal and non-neuronal cells, the activation mechanisms are the same [16][25]. After TRP channel activation, calcium release occurs through various pathways, depending on the specific TRP channel and cellular context [12][13][14][15][16][21,22,23,24,25]. Some TRP channels are involved in the regulation of store-operated calcium entry. In this process, TRP channels act as calcium-permeable channels located on the plasma membrane. When the endoplasmic reticulum (ER) calcium stores are depleted, usually due to receptor-mediated activation of phospholipase C (PLC) and subsequent inositol trisphosphate (IP3) production, the stromal interaction molecule (STIM) undergoes conformational changes and migrates to regions of the ER close to the plasma membrane, where it activates TRP channels [14][15][16][23,24,25]. This activation allows Ca2+ ions to enter the cytoplasm through the TRP channels, replenishing the depleted ER stores. Some other TRP channels can directly allow Ca2+ ions to enter the cell upon activation. These channels have a high permeability to calcium and are often referred to as calcium-permeable TRP channels. Activation of these TRP channels leads to conformational changes that open the channel pore, allowing Ca2+ ions to flow into the cytoplasm from the extracellular environment. The influx of calcium through these TRP channels can rapidly increase cytoplasmic calcium levels, triggering various cellular responses [14][15][16][23,24,25]. Following the evaporation of the tear film, activated TRPM8 receptors allow Ca2+ ions to enter the cell [11][12][20,21]. The increased intracellular calcium concentration activates calcium-dependent protein kinases (protein kinase C (PKC) and calcium/calmodulin-dependent protein kinase II (CaMKII)). PKC and CaMKII phosphorylate downstream target proteins, resulting in the activation of transcriptional factors (nuclear factors of activated T cells (NFAT) and cAMP response element-binding proteins (CREB)), which enhances the expression of genes that regulate the production and secretion of neuropeptides (substance P and calcitonin gene-related peptide (CGRP)) [11][12][20,21]. These neuropeptides stimulate tear production in lacrimal glands. Upon binding to neurokinin-1 and CGRP receptors, substance P and CGRP initiate the activation of cyclic adenosine monophosphate (cAMP) and PLC-driven intracellular signaling cascades within the lacrimal gland cells [11][12][20,21]. The cAMP pathway stimulates the opening of chloride (Cl-) channels, allowing the secretion of Cl- ions into the lacrimal gland ducts. This is followed by the efflux of sodium (Na+) ions and water, creating an osmotic gradient that drives the secretion of tears. Activated PLC catalyzes the hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2) into inositol 1,4,5-trisphosphate (IP3) and diacylglycerol (DAG) [10][11][19,20]. IP3 diffuses into the ER of lacrimal gland cells and binds to IP3 receptors, causing the release of Ca2+ ions from intracellular stores. The increase in intracellular calcium concentration activates calcium-activated chloride channels (CaCCs) present on the apical membrane of lacrimal gland cells [11][12][20,21]. These channels allow the efflux of chloride ions (Cl-) from the cytoplasm into the lumen of the lacrimal gland ducts. The efflux of chloride ions creates an osmotic gradient, which drives the movement of sodium ions (Na+) and water from the interstitium into the lumen of the ducts through paracellular and transcellular pathways [10][11][19,20]. Along with fluid secretion, the activation of the PLC pathway also stimulates the secretion of electrolytes into the lacrimal gland ducts. The combined effect of fluid and electrolyte secretion in the lacrimal gland results in tear production [11][12][20,21]. Since TRPM8/neuropeptide-dependent activation of cAMP and PLC in lacrimal gland cells is essential for optimal tear production and proper hydration of the ocular surface, any dysfunction of the TRPM8 receptors leads to reduced tear production and causes dryness of the ocular surface [11][12][13][14][20,21,22,23]. In addition to its effect on tear secretion, TRPM8 modulates the expression of genes that regulate the syntheses of tight junction proteins (occludin, claudin), adhesion molecules (E-cadherin), and actin-binding proteins (myosin light chain), maintaining the stability and integrity of the epithelial barrier on the ocular surface [13][14][22,23]. Accordingly, dysfunction of the TRPM8 receptors causes an increased permeability of the ocular surface epithelium, enhanced evaporation of tears, decreased tear film stability, and dryness of the ocular surface [14][15][23,24]. Also, TRPM8 dysfunction causes heightened ocular surface sensitivity, discomfort, and pain, which are the main clinical symptoms reported by DED patients [13][14][15][22,23,24]. These findings are in line with results obtained by other researchers in two pilot clinical trials, which revealed that topical administration of the TRPM8 agonist (cryosim-3) significantly increased basal tear production and lessened neuropathic pain in DED patients, indicating that the use of TRPM8 agonists could be considered as a potential new therapeutic approach for the treatment of DED-related ocular discomfort [20][21][29,30]. Approximately half of corneal TRPM8+ neurons express the TRPV1 channel that allows the passage of calcium, sodium, and potassium ions [22][31]. TRPV1 is highly expressed in corneal and conjunctival TRPM8+ sensory neurons, and in anterior eye samples and trigeminal ganglia of mice and rats with DED [13][22]. An increased osmolarity of the tear film triggers a conformational change in these TRPV1 channels, leading to their opening. Massive influxes of cations cause disruption to cellular homeostasis [14][23]. Accordingly, THO-dependent prolonged activation of TRPV1 channels causes tear film instability and compromises the integrity of the epithelial barrier in the eyes, exacerbating DED [14][15][23,24]. Also, activation of TRPV1 in human CECs importantly contributes to the development of ocular inflammation in DED patients [23][32]. TRPV1-dependent increases in the intracellular concentration of calcium, which leads to the activation of mitogen-activated protein kinase (MAPK) and transcriptional factor NF-κB, resulting in an enhanced production of inflammatory cytokines (IL-6 and IL-8) [23][32]. Additionally, the nociception experienced with DED is a result of TRPV1 activation on the ophthalmic branch of the corneal trigeminal nerve endings [24][33]. Bearing in mind that a continuous activation of TRPV1 aggravates DED [13][14][15][22,23,24], Benitez-Del-Castillo and colleagues conducted phase I and II pilot clinical trials to test the safety and efficacy of SYL1001 (TRPV1-specific short interfering RNA) in DED patients [25][34]. Topical administration of SYL1001 significantly extended tear break-up time, prevented THO, improved the disease index score of ocular surfaces, and attenuated conjunctival hyperemia in the eyes of DED patients, without causing any severe side effects [25][34].The Impact of Hormones, Medication, and Environmental Factors on Tear Osmolarity
Hormones (cortisol, aldosterone, thyroid hormones, etc.), medications (antihistamines, beta-blockers, diuretics, isotretinoin, anti-cholinergics, etc.), and environmental factors all affect tear osmolarity and regulate tear-dependent eye protection. Cortisol can increase tear osmolarity by enhancing the expression of sodium channels in CECs, which can lead to an increase in the transportation of sodium ions into the tear film. Aldosterone, on the other hand, can increase the production of sodium–potassium pumps in the cornea, which can lead to an increase in the transportation of potassium ions out of the tear film [26][27][28][15,16,17]. This can also lead to an increase in tear osmolarity. Thyroid hormones (thyroxine (T4) and triiodothyronine (T3)) can affect the metabolism of cells in the lacrimal gland, which can influence the production and composition of tears, affecting tear osmolarity [29][35]. The increased production of thyroid hormones in overactive thyroid glands usually results in increased tear production and decreased tear osmolarity, as the metabolism of cells in the lacrimal gland is increased. Therefore, epiphora, watery eyes, is frequently observed in patients with hyperthyroidism. On the other hand, patients with hypothyroidism, or an underactive thyroid gland, may have a decreased tear production and an increased tear osmolarity, as the metabolism of cells in the lacrimal gland is decreased [27][28][16,17]. Lucius and colleagues showed that a thyroxine metabolite, 3-iodothyronamine (3T1AM), could act as a TRPM8 agonist. A significant increase in the intracellular Ca2+ influx was observed in 3T1AM-exposed immortalized human CECs, suggesting that 3T1AM-type analogs should be used as the leading compounds in developing drugs that would directly activate TRPM8 and reduce desiccation of the anterior ocular surface epithelia [29][35].3. THO-Related Pathological Changes in the Eyes of DED Patients
Lid margins, preocular tear film, and conjunctival sacs display distinct tear volumes and different tear osmolarities [30][36]. Decreased tear flow and environmental factors (low relative humidity, high wind speed, raised air temperature) may increase tear osmolarity [31][37]; it is at its the lowest upon waking, and rises very quickly during the day, reaching baseline levels within 40 min [31][32][37,38]. Tear osmolarities are usually measured using samples drawn from the lower tear meniscus in resting conditions [32][38]. The average tear osmolarity in resting conditions, measured in lower tear menisci of healthy eyes in resting conditions, is 302 ± 9.7 mOsm/L. The ocular surface, when exposed to tears with osmolarities ranging from 292.3 to 311.7 mOsm/L, is protected from any harmful effects of osmolarity [32][38]. The most sensitive baseline for distinguishing normal eyes from those with mild–moderate DED is a tear osmolarity of 308 mOsm/L (measured in the lower meniscus), and the most definite cut-off is 316 mOsm/L [32][38]. Tear osmolarities of up to 519 mOsm/L have been reported clinically [33][39], and the highest levels of osmolarity have been hypothesized to be at sites of tear film break-up [34][40]. The tear film is composed of three distinct (lipid, aqueous, and mucin) layers, which work together to provide lubrication, protect the ocular surface from infections, and maintain clear vision [35][41]. The lipid layer reduces tear evaporation, the aqueous layer provides moisture and nutrients, and the mucin layer ensures the proper adherence and distribution of tears. Any disruption or imbalance in these layers can lead to tear film instability, which importantly contributes to THO development [35][41]. Tears are drained via the nasolacrimal system and lost via evaporation. Enhanced tear evaporation disrupts the layered structure of the tear film and increases its osmolarity [35][36][41,42]. Specifically, tear osmolarity will double if evaporation reduces the aqueous layer of tear film to half of its initial thickness, provided that any tear solutes, including salts, are not lost from the aqueous layer (for example, via diffusion out of the region) [6]. In addition to increased tear osmolarity, enhanced evaporation reduces the tear film thickness, disrupting its normal structure and making it more susceptible to break-up [31][32][37,38]. Evaporation-driven tear film rupture is observed using fluorescence imaging as black circular spots, linear streaks, or irregular pools on a yellow-green fluorescence background [35][41]. The tear film is refreshed by blinking, which, in people with healthy eyes, occurs with a frequency of 10 to 30 times per minute [31][32][37,38]. When blinking is slowed, tear film break-ups appear within 15 to 40 s, in individuals with healthy eyes. However, tear film break-up regions (“black spots/streaks”) have been observed in the eyes of DED patients every 2–3 s [36][37][42,43]. Importantly, these “black spots/streaks” arose in areas where the aqueous layer of the tear film was entirely ruptured down to the underlying mucin/corneal interface, leaving the underlying epithelial cells completely unprotected [36][37][42,43]. Since osmolarity in the tear film break-up regions of DED patients can be dramatically high (between 800 and 900 mOsM) [38][44], THO is recognized as a major cause of ocular surface damage in DED patients. The most damaging THO-dependent pathological changes mainly develop in local salinity spots, which arise in the black spots of tear breakup [34][37][40,43]. Since the process of osmoregulation, which guard the ocular surface epithelia and maintain normal vision, is affected when the osmolarity of the tears is greater than that of the epithelial cells, THO is considered as an initial, important step in the development, progression, and aggravation of DED [6][27][39][6,9,16]. Hypertonicity induces activation of the TRPV1 signaling pathway in CECs, resulting in the activation of nuclear factor kappa B (NF-κB) [38][40][44,45]. By triggering NF-κB signaling, THO induces apoptotic cell death in CECs and disrupts the integrity of the corneal epithelial barrier, leading to increased permeability and susceptibility to infection [38][40][44,45]. In line with these findings are the results recently obtained by Guindolet and colleagues, who demonstrated that hyperosmotic environments caused the apoptosis of corneal and conjunctival epithelial cells by inducing dysfunction in the ER (Figure 2) [41][46]. The ER is cellular organelle that contains chaperones and folding enzymes, which facilitate the assembly of newly synthesized proteins, preventing their misfolding and aggregation [42][47]. A hyperosmotic microenvironment affects the transportation of secretory content in the ER and attenuates its capacity to fold proteins [41][46]. The resulting accumulation of unfolded proteins activates a cascade of stress-related signaling, referred to as the unfolded protein response (UPR), which transiently attenuates translation and increases protein folding in ERs of stressed epithelial cells [41][46]. An increased UPR activity, induced by THO, enhances the synthesis of transcription factor X-box binding protein 1 (XBP1), which directs the expression of chaperones and folding enzymes to restore homeostasis. If THO induces severe ER stress that cannot be attenuated by XBP1s, the UPR increases the activity of DNA damage-inducible transcript 3 protein (DDIT3), initiating apoptosis and the removal of stressed corneal and conjunctival epithelial cells. THO-dependent induction of ER-stress-associated programmed death of these cells results in the disruption of the ocular surface epithelial barrier, paving the way for the entrance of invading pathogens in the eyes of DED patients [41][46].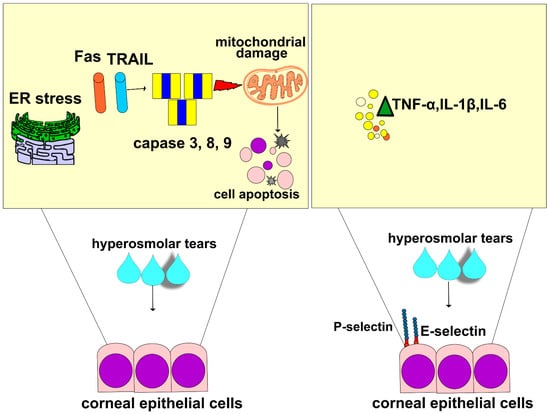
Figure 2. THO-induced changes in the phenotype and function of CECs. Apoptotic cell death is observed in THO-exposed CECs. THO induces stress in the ER and promotes mitochondrial damage by enhancing Fas- and TRAIL-dependent activation of caspase-3, capsase-8, and caspase-9, which results in apoptosis of THO-exposed CECs. Additionally, THO promotes an increased expression of E and P selectins and induces an enhanced production of inflammatory cytokines (TNF-α, IL-1β, IL-6) in CECs, which results in a massive influx of circulating immune cells in inflamed eyes of DED patients, resulting in the aggravation of ongoing inflammation.
