Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 1 by Marion Mackonochie.
Metabolic syndrome (MetS) is a growing global health problem. Evidence suggests that diets rich in phytochemical-containing herbs and spices can contribute to reducing the risk of chronic diseases.
- diabetes
- herbs and spices
- metabolic syndrome
- nutrition
- phytochemicals
- preventative health
1. Introduction
Metabolic syndrome (MetS) and its associated conditions, such as obesity, diabetes and cardiovascular disease, are a growing global health problem. Between 2000 and 2019, global diabetes rates grew by more than 1.5% annually and prevalence rates for all other metabolic diseases also increased [1]. Poor diet and physical inactivity are risk factors for the development of MetS and lifestyle changes are key for treatment [2]. MetS involves the dysregulation of blood glucose, insulin resistance, raised blood lipids, increased inflammation and high blood pressure [2]. Therefore, measuring these biomarkers in healthy individuals can indicate the risk of MetS developing or can be used to monitor progress in those with MetS.
Research indicates that the inclusion of herbs and spices in the diet, as is often the case in Mediterranean and Asian diets, may contribute to positive long-term health outcomes [3,4][3][4]. Herbs and spices are a particularly rich source of phytochemicals and the consumption of diets rich in phytochemicals has been linked with a reduced risk of cardiometabolic disease and obesity [5,6][5][6].
Many studies looking at the health benefits of herbs and spices use high-dose extracts; however, these do not reflect the main way that the general public might be able to take advantage of these relatively cheap additions to their diet. Are these more expensive high-dose formulations necessary for everyone to benefit from herbs and spices, or do culinary doses provide benefits too?
Some researchers have begun to investigate this question. Clinical studies using herb and spice mixes to improve physiological responses to food have indicated that the inclusion of herbs/spices in the diet may have preventative or therapeutic benefits [7,8,9,10,11,12,13,14,15][7][8][9][10][11][12][13][14][15]. The spice mixes used in these studies ranged in dose from 6 g to 23.5 g and positively impacted vascular function, blood glucose and insulin and blood lipids following meals. These effects may contribute to a reduced risk of MetS and its associated conditions when herbs and spices are consumed regularly. The reasons for the specific herb/spice mixes chosen and doses used were often not explained. Doses of 6 g of Italian herb mixes [8], 23.5 g of Asian spices [11] or a combination of Mediterranean herbs and Asian spices at doses of 14.5 g [10] and between 0.5 and 6.6 g [13,14][13][14] have been found to have benefits. The lack of consistency in herb/spice mix formulations makes it challenging to attribute benefits to a particular herb/spice, a combination of herb/spices or a dose.
Zanzer et al. assessed the effect of the concentrated liquid extracts of individual spices, but standardized them to equal polyphenol contents, enabling the different effects from each spice to be elucidated [15]. The dose of polyphenols provided from each extract corresponded to the amount found in 6 g of cinnamon. Cinnamon and turmeric positively impacted on blood sugar levels, and turmeric reduced appetite; however, ginger and star anise did not have any effect. Therefore, the individual effects from different herbs goes beyond a general benefit from polyphenol intake and needs to be clarified.
2. Black Pepper, Cardamom and Chilli
There was one single-blind cross-over trial on black pepper in healthy adults. A dose of 1.3 g added to a meal had no impact on appetite or thermogenesis [138][16]. Ten studies (eight double-blind RCTs, one single-blind RCT and one clinical study) looked at the impact of cardamom on inflammation and a range of metabolic markers in individuals with hypertension [27][17], diabetes [29[18][19][20],32,59], prediabetes [28][21], poly-cystic ovarian syndrome (PCOS) [34,35][22][23] and non-alcoholic fatty liver disease (NAFLD) [30,33][24][25]. All the studies on cardamom used 3 g/day for between 8 and 20 weeks. Five out of six studies that investigated inflammatory markers found positive effects [28[19][21][22][23][24][26],30,31,32,34,35], two studies found benefits on blood glucose and insulin and two studies found no benefit from cardamom on blood lipids, while effects on blood pressure were variable. Eleven clinical studies [9,36,37,38,39,40,41,42,43,44,45][9][27][28][29][30][31][32][33][34][35][36] investigated the effects of chilli on appetite, vascular function and blood glucose, insulin and lipids. Apart from one study looking at the effect of chilli on glucose and insulin in pregnant women with gestational diabetes [42][33], all the included studies were in healthy individuals. Four of the intervention studies used doses of 30 g of fresh chilli [36,37[27][28][29][30],38,39], the other seven intervention studies used doses of 0.6 g [40][31], 1.25 g [42][33], 3.09 g [44,45][35][36] or 5 g [43][34], a meal with chilli containing 5.82 mg of capsaicinoids [9] or chilli capsules containing 10 mg of capsaicinoids [41][32]. Appetite and/or thermogenesis or metabolic rate were measured in eight out of thirteen of the studies and five of these found a beneficial effect. There were as many studies finding positive results as those showing no effect for the key metabolic biomarkers of blood glucose, insulin and lipids (see Figure 21).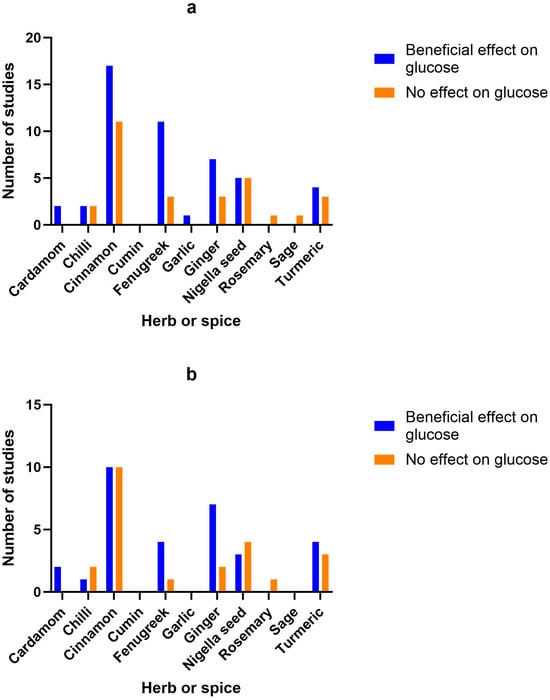
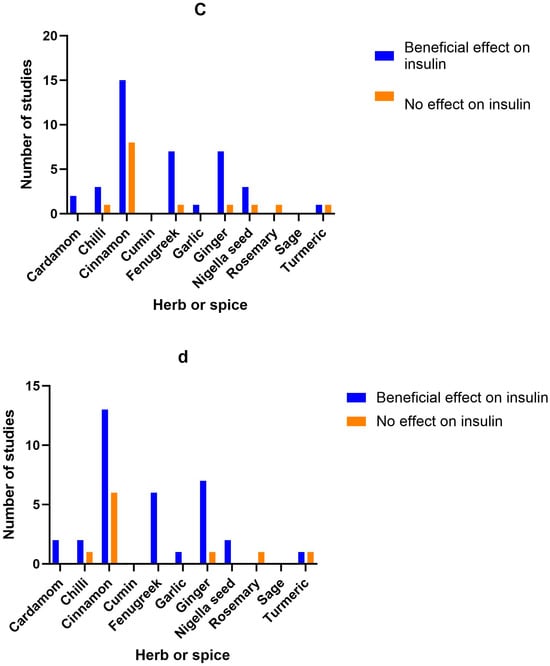
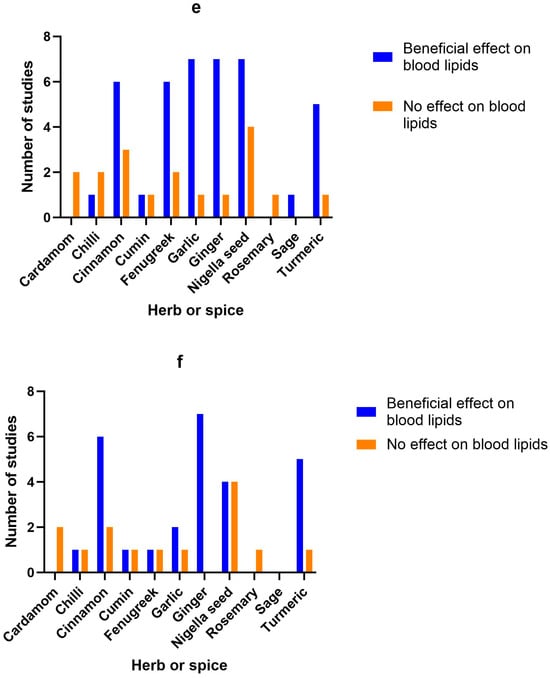
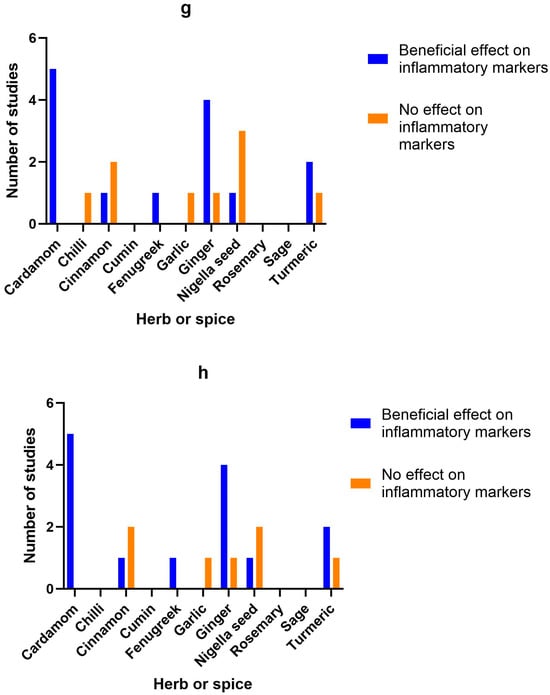
Figure 21. Number of studies and high-quality studies demonstrating the effect of herbs/spices in specific cardiometabolic biomarkers. Figure 21 identifies the main health markers measured and whether effects were seen for each of the herbs and spices in all studies and only in high-quality studies: (a) Number of studies showing an effect or lack of effect for each of the herbs and spices on blood glucose; (b) Number of high-quality studies showing an effect or lack of effect for each of the herbs and spices on blood glucose; (c) Number of studies showing an effect or lack of effect for each of the herbs and spices on insulin; (d) Number of high-quality studies showing an effect or lack of effect for each of the herbs and spices on insulin; (e) Number of studies showing an effect or lack of effect for each of the herbs and spices on blood lipids; (f) Number of high-quality studies showing an effect or lack of effect for each of the herbs and spices on blood lipids; (g) Number of studies showing an effect or lack of effect for each of the herbs and spices on inflammatory markers; (h) Number of high-quality studies showing an effect or lack of effect for each of the herbs and spices on inflammatory markers.
3. Cinnamon
There were 41 studies looking at the benefits of culinary doses of cinnamon. Ten in healthy individuals [46,48,49,50,54[37][38][39][40][41][42][43][44][45][46],55,56,57,81,82], nineteen in those with diabetes [47[20][47][48][49][50][51][52][53][54][55][56][57][58][59][60][61][62][63][64],53,59,60,61,63,64,66,67,68,69,70,71,74,75,76,78,79,84], six in women with PCOS [58,65[65][66][67][68][69][70],72,73,80,83], one in Asian Indians with MetS [77][71], one in patients with NAFLD [62][72], one in individuals with impaired glucose tolerance [51][73], one in sedentary women with obesity [52][74], one in women with dyslipidaemia [86][75] and one in prediabetic individuals [166][76]. Doses ranged from 1 to 6 g, either as a single dose or daily for between 2 weeks and 6 months. Whether a positive effect was seen or not did not appear to correlate with dosage. Beneficial effects on glucose were found in 6 randomized cross-over studies, 1 randomized trial and 10 double-blind RCTs from doses of 0.5–6 g/day, 100 mL of cinnamon tea or single doses of 5–6 g of cinnamon [46,48,52,53,54[37][38][41][42][43][44][46][48][59][60][61][62][63][68][71][72][74],55,56,57,62,73,74,75,76,77,78,79,82], while 7 double-blind RCTs, 3 single-blind RCTs and 1 randomized cross-over study found no effect from a single dose of 1–6 g or 1–1.5 g/day [47,49,51,60,61,63,65,70,71,80,166][39][47][49][50][51][57][58][66][69][73][76]. Beneficial effects on insulin were found in 4 randomized cross-over studies, 10 double-blind RCTs and 1 single-blind RCT from doses of 1–3 g/day or single doses of 3–6 g of cinnamon [46,48,49,57,59,62,68,70,73,75[20][37][38][39][44][55][57][60][62][63][68][69][70][71][72],77,78,79,80,83], while 6 double-blind RCTs, 1 single-blind RCT and 1 randomized cross-over study found no effect from doses of 1–1.5 g/day or a single dose of 6 g [47,49,51,53,60,67,71,166][39][47][48][49][54][58][73][76].4. Coriander Seed, Cumin and Fennel
One single-blind RCT found that 2 g/day of coriander seeds for 40 days improved average body mass index (BMI) from 27.3 to 26.7 and blood lipids (total cholesterol, low-density lipoprotein (LDL) and high-density lipoprotein (HDL)), as well as systolic blood pressure, in patients with hyperlipidaemia [116][77]. Two clinical studies looked at the benefit of cumin on anthropometric measures, blood insulin and blood lipid levels in overweight adults [85][78] and women with dyslipidaemia [86][75]. The randomised clinical trial by Zare et al. used a dose of 6 g/day for 3 months and this reduced all blood lipid measurements, as well as anthropometric measurements of weight, body mass index (BMI), waist circumference and fat [85][78], while Pishdad et al. used 3 g/day for 8 weeks in a double-blind RCT and found a benefit on total cholesterol, but not LDL or HDL cholesterol [86][75]. One single-blind crossover study found that a single dose of 2 g of fennel as a tea decreased appetite in healthy women, but did not impact food consumption [87][79].5. Fenugreek
There were twenty studies looking at fenugreek, mainly for its impact on blood glucose, insulin and lipids, in healthy individuals [87[79][80][81][82],91,92,95], diabetics [89,90[83][84][85][86][87][88][89][90][91][92][93][94][95][96],93,94,96,97,98,99,100,101,103,104,105,106], individuals with coronary artery disease [137][97] and adults with hyperlipidaemia/hypercholesterolaemia [88,102][98][99]. Quantities ranged from 2 g up to 100 g, with the majority of studies using 10–15 g/day. Effects on blood insulin, glucose and lipids were promising, with 11 out of 14 studies showing significant positive effects on blood glucose, 7 out of 8 studies finding significant changes in insulin and 6 out of 8 studies significantly improving blood lipids, regardless of dose used. However, excluding low-quality studies reduced the number of studies indicating a benefit on blood glucose (to 4 out of 5 studies) and blood lipid levels (to 1 out of 2 studies).6. Garlic
There were ten clinical studies (four double-blind RCTs and six single-blind or randomised clinical studies) looking at the benefits of garlic. Both clinical trials that looked at the effect of garlic on blood pressure (BP) found benefits when participants consumed 20 g or 100 mg/kg bodyweight of fresh garlic daily [107,111][100][101]. Most of the studies investigated the impact of garlic on blood lipids. One clinical study was carried out on overweight smokers [112][102]. Four clinical studies looked at platelet function [110][103], cholesterol [108[104][105],109], immunity and cancer markers [168][106] in healthy individuals. Two studies looked at multiple outcomes in patients with MetS [107[100][107],115], one study investigated NAFLD [114][108] and two studies looked at individuals with hyperlipidaemia [111,116][77][101]. For the interventional studies, doses ranged from 1.6 g to 40 g, with higher doses of fresh garlic compared with dried garlic powder. All but two of the clinical studies looked at blood lipids and seven out of eight found a benefit. Fresh garlic in doses of 100 mg/kg body weight, 20 g or 40 g/day significantly reduced triglycerides in three studies [107,108[100][101][104],111], while two studies found that 1.6 g/day of dried garlic reduced triglycerides [113,115][107][109]. Total cholesterol was significantly reduced by 1.6, 2 or 3 g/day dried garlic and 20 g or 40 g of fresh garlic [108,109,111,113,116][77][101][104][105][109]. Only one study of overweight participants at risk of cardiovascular disease found no impact of 2.1 g of garlic on blood lipids [112][102].7. Ginger
Out of a total of 24 studies on ginger, 6 were carried out on healthy individuals to look at blood clotting [119][110], energy intake and appetite [138][16], thermoregulatory function or thermogenesis and appetite [118[111][112],120], anthropometric measurements [128[113][114],133], anthropometric measurements and blood glucose and fats [130][115] and cardiovascular risk factors [137][97]. There were 11 studies on patients with type 2 diabetes looking at the impact of ginger on blood sugar, insulin and blood lipids [126[116][117][118],134,135], metabolic health and inflammation [125[119][120],132], fasting blood glucose and insulin sensitivity [127[121][122],129], blood glucose, insulin and inflammation [121][123], vascular function [122][124], anthropometric measurements and blood pressure [84][64] and anthropometric measurements and inflammation [124][125]. One study looked at the effects of 1.5 g of ginger on anthropometric measurements and insulin resistance in women with PCOS [83][70]. One study looked at the effect of 3 g/day on blood lipids in individuals with hyperlipidaemia [136][126]. Two studies looked at the impact of ginger on liver function, anthropometric measurements, blood sugar and inflammatory markers in individuals with NAFLD [117,123][127][128]. One looked at the impact of 1 g of ginger daily in obese children with NAFLD [117][127], while, in the other study, adults were given 1.5 g/day [123][128]. A pilot study investigated the impact of 1 g/day of ginger on thyroid symptom score, anthropometric measurements, blood glucose and blood lipids in hypothyroid patients [131][129]. Ginger was used in doses that ranged from 1 g to 10 g of dried powdered ginger for a single dose or up to 12 weeks daily, apart from one study that used 15 g of fresh ginger or 40 g of cooked ginger [119][110] and another study that used 20 g of fresh ginger [138][16]. There did not appear to be a correlation between dose and efficacy. All seven studies that investigated the impact of ginger (doses of 1.5–3 g/day) on insulin found a benefit, ten out of twelve found positive effects on blood glucose (doses of 1.2–3 g/day), six out of seven found a positive effect on blood lipids, such as total cholesterol, LDL and triglycerides (doses of 1–3 g) and four out of five studies looking at inflammatory markers (doses of 1.5–3 g) found a benefit. The studies were mainly of high quality (22 out of 24) according to Jadad scoring, with 18 double-blind RCTs, 3 randomized cross-over studies and 3 placebo-controlled study.8. Nigella Seeds
There were 17 studies on nigella seeds, mainly investigating their effect on anthropometric measurements, blood glucose, insulin and lipids. One double-blind RCT was carried out on healthy male volunteers [141][130]. A large double-blind RCT looked at the impact of 1.5 g/day of nigella seeds in 250 healthy men with MetS [165][131]. One double-blind RCT was carried out on men with obesity [153][132]. Two studies were carried out with thyroiditis patients [147,150][133][134], four in individuals with MetS [139[135][136][137][138],140,143,152], three in patients with hyperlipidemia/hypercholesterolaemia [144[139][140][141],146,154], three in patients with type 2 diabetes [142,145,151][142][143][144] and two in patients with NAFLD [148,149][145][146]. The studies on nigella seeds used between 500 mg and 3 g/day for durations ranging from 4 weeks to 1 year. Nigella seeds improved anthropometric measurements such as BMI and weight in three out of seven studies (at doses of 2–3 g/day), improved blood glucose in five out of ten studies (at doses of 500 mg–2 g/day), insulin (at 2 g/day) in three out of four studies, blood lipids in seven out of eleven studies (at 500 mg–2 g/day) and inflammatory markers in one out of four studies (at a dose of 2 g/day). Of the 17 studies, 13 were high-quality according to Jadad.9. Rosemary, Sage and Turmeric
The one high-quality, double-blind RCT on rosemary found no impact on liver enzymes, anthropometric measurements, fasting blood glucose, insulin and blood lipids from 4 g/day for 8 weeks in patients with NAFLD [155][147]. One low-quality, non-randomised cross-over study found that drinking 600 mL of sage tea daily for 4 weeks improved lipid profile but had no effect on blood glucose in healthy female volunteers aged 40–50 years [156][148]. Five out of the eleven studies on turmeric looked at patients with type 2 diabetes [157,159,161,162,164][149][150][151][152][153]. One turmeric study was carried out on healthy volunteers to investigate glycaemic effect [158][154]. Two other studies were carried out on individuals who were stated to be overweight, obese or prediabetic, with no other health issues [166,167][76][155]. Two studies looked at the effect of turmeric on NAFLD [163,169][156][157]. The studies used between 1 and 3 g/day for between 4 and 12 weeks, or single doses of 1 g [166][76] and 6 g [158][154]. All studies were of a high quality according to Jadad. Three out of five studies investigating anthropometric measurements, such as weight and BMI, found some positive effect from turmeric (at a dose of 2.1 g/day). Four out of seven studies found improvements in blood glucose levels (at doses of 2.1–2 g/day), one out of two studies found improvements in insulin (from a dose of 2 g/day) and five out of six studies found improvements in blood lipids such as triglycerides, total cholesterol and LDL (at doses of 2.1–2.4 g/day). Out of three studies looking at inflammatory markers, two found beneficial effects from 2.1 to 2.4 g/day of turmeric powder in capsules.10. Herb/Spice Efficacy
Figure 21 identifies the main health markers measured and whether effects were seen for each of the herbs and spices in all studies and only in high-quality studies. Blood glucose and insulin were the most commonly measured markers, followed by blood lipids, then inflammatory markers. Only including high-quality studies did not make a big difference to the pattern of responses seen for glucose, insulin or inflammatory markers. However, the benefits of fenugreek and garlic on blood lipids were not apparent when only high-quality studies were considered.11. Adverse Effects
No adverse effects were reported for any of the studies at the doses used.References
- Chew, N.W.S.; Ng, C.H.; Tan, D.J.H.; Kong, G.; Lin, C.; Chin, Y.H.; Lim, W.H.; Huang, D.Q.; Quek, J.; Fu, C.E.; et al. The global burden of metabolic disease: Data from 2000 to 2019. Cell Metab. 2023, 35, 414–428.e3.
- Alkhatib, D.H.; Jaleel, A.; Tariq, M.N.M.; Feehan, J.; Apostolopoulos, V.; Cheikh Ismail, L.; Stojanovska, L.; Al Dhaheri, A.S. The role of bioactive compounds from dietary spices in the management of metabolic syndrome: An overview. Nutrients 2021, 14, 175.
- Jiang, T.A. Health benefits of culinary herbs and spices. J. AOAC Int. 2019, 102, 395–411.
- Pallauf, K.; Giller, K.; Huebbe, P.; Rimbach, G. Nutrition and healthy ageing: Calorie restriction or polyphenol-rich “MediterrAsian” diet? Oxid. Med. Cell Longev. 2013, 2013, 707421.
- Bahadoran, Z.; Golzarand, M.; Mirmiran, P.; Saadati, N.; Azizi, F. The association of dietary phytochemical index and cardiometabolic risk factors in adults: Tehran Lipid and Glucose Study. J. Hum. Nutr. Diet. 2013, 26 (Suppl. 1), 145–153.
- Dzah, C.S.; Asante-Donyinah, D.; Letsyo, E.; Dzikunoo, J.; Adams, Z.S. Dietary polyphenols and obesity: A review of polyphenol effects on lipid and glucose metabolism, mitochondrial homeostasis, and starch digestibility and absorption. Plant Foods Hum. Nutr. 2022, 78, 1–12.
- Haldar, S.; Chia, S.C.; Henry, C.J. Polyphenol-rich curry made with mixed spices and vegetables increases postprandial plasma GLP-1 concentration in a dose-dependent manner. Eur. J. Clin. Nutr. 2018, 72, 297–300.
- Huang, Y.; Tsai, M.F.; Thorat, R.S.; Xiao, D.; Zhang, X.; Sandhu, A.K.; Edirisinghe, I.; Burton-Freeman, B.M. Endothelial function and postprandial glucose control in response to test-meals containing herbs and spices in adults with overweight/obesity. Front. Nutr. 2022, 9, 811433.
- Kroff, J.; Hume, D.J.; Pienaar, P.; Tucker, R.; Lambert, E.V.; Rae, D.E. The metabolic effects of a commercially available chicken peri-peri (African bird’s eye chilli) meal in overweight individuals. Br. J. Nutr. 2017, 117, 635–644.
- McCrea, C.E.; West, S.G.; Kris-Etherton, P.M.; Lambert, J.D.; Gaugler, T.L.; Teeter, D.L.; Sauder, K.A.; Gu, Y.; Glisan, S.L.; Skulas-Ray, A.C. Effects of culinary spices and psychological stress on postprandial lipemia and lipase activity: Results of a randomized crossover study and in vitro experiments. J. Transl. Med. 2015, 13, 7.
- Nakayama, H.; Tsuge, N.; Sawada, H.; Masamura, N.; Yamada, S.; Satomi, S.; Higashi, Y. A single consumption of curry improved postprandial endothelial function in healthy male subjects: A randomized, controlled crossover trial. Nutr. J. 2014, 13, 67.
- Oh, E.S.; Petersen, K.S.; Kris-Etherton, P.M.; Rogers, C.J. Spices in a high-saturated-fat, high-carbohydrate meal reduce postprandial proinflammatory cytokine secretion in men with overweight or obesity: A 3-period, crossover, randomized controlled trial. J. Nutr. 2020, 150, 1600–1609.
- Petersen, K.S.; Rogers, C.J.; West, S.G.; Proctor, D.N.; Kris-Etherton, P.M. The effect of culinary doses of spices in a high-saturated fat, high-carbohydrate meal on postprandial lipemia and endothelial function: A randomized, controlled, crossover pilot trial. Food Funct. 2020, 11, 3191–3200.
- Petersen, K.S.; Davis, K.M.; Rogers, C.J.; Proctor, D.N.; West, S.G.; Kris-Etherton, P.M. Herbs and spices at a relatively high culinary dosage improves 24-hour ambulatory blood pressure in adults at risk of cardiometabolic diseases: A randomized, crossover, controlled-feeding study. Am. J. Clin. Nutr. 2021, 114, 1936–1948.
- Zanzer, Y.C.; Plaza, M.; Dougkas, A.; Turner, C.; Östman, E. Black pepper-based beverage induced appetite-suppressing effects without altering postprandial glycaemia, gut and thyroid hormones or gastrointestinal well-being: A randomized crossover study in healthy subjects. Food Funct. 2018, 9, 2774–2786.
- Gregersen, N.T.; Belza, A.; Jensen, M.G.; Ritz, C.; Bitz, C.; Hels, O.; Frandsen, E.; Mela, D.J.; Astrup, A. Acute effects of mustard, horseradish, black pepper and ginger on energy expenditure, appetite, ad libitum energy intake and energy balance in human subjects. Br. J. Nutr. 2013, 109, 556–563.
- Verma, S.K.; Jain, V.; Katewa, S.S. Blood pressure lowering, fibrinolysis enhancing and antioxidant activities of cardamom (Elettaria cardamomum). Indian J. Biochem. Biophys. 2009, 46, 503–506.
- Aghasi, M.; Koohdani, F.; Qorbani, M.; Nasli-Esfahani, E.; Ghazi-Zahedi, S.; Khoshamal, H.; Keshavarz, A.; Sotoudeh, G. Beneficial effects of green cardamom on serum SIRT1, glycemic indices and triglyceride levels in patients with type 2 diabetes mellitus: A randomized double-blind placebo controlled clinical trial. J. Sci. Food Agric. 2019, 99, 3933–3940.
- Ghazi Zahedi, S.; Koohdani, F.; Qorbani, M.; Nasli-Esfahani, E.; Aghasi, M.; Khoshamal, H.; Sotoudeh, G. The effects of Elettaria cardamom supplementation on inflammatory markers and vascular function in patients with type 2 diabetes mellitus: A mechanism -based randomized clinical trial. J. Herb. Med. 2021, 25, 100403.
- Crawford, P. Effectiveness of cinnamon for lowering hemoglobin A1C in patients with type 2 diabetes: A randomized, controlled trial. J. Am. Board. Fam. Med. 2009, 22, 507–512.
- Kazemi, S.; Yaghooblou, F.; Siassi, F.; Rahimi Foroushani, A.; Ghavipour, M.; Koohdani, F.; Sotoudeh, G. Cardamom supplementation improves inflammatory and oxidative stress biomarkers in hyperlipidemic, overweight, and obese pre-diabetic women: A randomized double-blind clinical trial. J. Sci. Food Agric. 2017, 97, 5296–5301.
- Cheshmeh, S.; Elahi, N.; Ghayyem, M.; Mosaieby, E.; Moradi, S.; Pasdar, Y.; Tahmasebi, S.; Moradinazar, M. Effect of green cardamom on the expression of genes implicated in obesity and diabetes among obese women with polycystic ovary syndrome: A double blind randomized controlled trial. Genes. Nutr. 2022, 17, 17.
- Cheshmeh, S.; Ghayyem, M.; Khamooshi, F.; Heidarzadeh-Esfahani, N.; Rahmani, N.; Hojati, N.; Mosaieby, E.; Moradi, S.; Pasdar, Y. Green cardamom plus low-calorie diet can decrease the expression of inflammatory genes among obese women with polycystic ovary syndrome: A double-blind randomized clinical trial. Eat. Weight. Disord. 2022, 27, 821–830.
- Daneshi-Maskooni, M.; Keshavarz, S.A.; Qorbani, M.; Mansouri, S.; Alavian, S.M.; Badri-Fariman, M.; Jazayeri-Tehrani, S.A.; Sotoudeh, G. Green cardamom supplementation improves serum irisin, glucose indices, and lipid profiles in overweight or obese non-alcoholic fatty liver disease patients: A double-blind randomized placebo-controlled clinical trial. BMC Complement. Altern. Med. 2019, 19, 59.
- Daneshi-Maskooni, M.; Keshavarz, S.A.; Qorbani, M.; Mansouri, S.; Alavian, S.M.; Badri-Fariman, M.; Jazayeri-Tehrani, S.A.; Sotoudeh, G. Green cardamom increases Sirtuin-1 and reduces inflammation in overweight or obese patients with non-alcoholic fatty liver disease: A double-blind randomized placebo-controlled clinical trial. Nutr. Metab. 2018, 15, 63.
- Ghazi Zahedi, S.; Koohdani, F.; Qorbani, M.; Nasli-Esfahani, E.; Aghasi, M.; Khoshamal, H.; Keshavarz, A.; Sotoudeh, G. Effects of green cardamom supplementation on serum levels of Hs-CRP, dimethylarginine, nitric oxide and blood pressure in patients with type 2 diabetes: A randomized, double-blind, placebo controlled, clinical trial. J. Herb. Med. 2022, 32, 100555.
- Clegg, M.E.; Golsorkhi, M.; Henry, C.J. Combined medium-chain triglyceride and chilli feeding increases diet-induced thermogenesis in normal-weight humans. Eur. J. Nutr. 2013, 52, 1579–1585.
- Ahuja, K.D.; Robertson, I.K.; Geraghty, D.P.; Ball, M.J. Effects of chili consumption on postprandial glucose, insulin, and energy metabolism. Am. J. Clin. Nutr. 2006, 84, 63–69.
- Ahuja, K.D.; Ball, M.J. Effects of daily ingestion of chilli on serum lipoprotein oxidation in adult men and women. Br. J. Nutr. 2006, 96, 239–242.
- Ahuja, K.D.; Robertson, I.K.; Geraghty, D.P.; Ball, M.J. The effect of 4-week chilli supplementation on metabolic and arterial function in humans. Eur. J. Clin. Nutr. 2007, 61, 326–333.
- Reinbach, H.C.; Martinussen, T.; Møller, P. Effects of hot spices on energy intake, appetite and sensory specific desires in humans. Food Qual. Prefer. 2010, 21, 655–661.
- Kang, C.; Zhang, Y.; Zhu, X.; Liu, K.; Wang, X.; Chen, M.; Wang, J.; Chen, H.; Hui, S.; Huang, L.; et al. Healthy subjects differentially respond to dietary capsaicin correlating with specific gut enterotypes. J. Clin. Endocrinol. Metab. 2016, 101, 4681–4689.
- Yuan, L.J.; Qin, Y.; Wang, L.; Zeng, Y.; Chang, H.; Wang, J.; Chen, S.-H.; Zhang, Q.-Y.; Zhu, J.-D.; Zhou, Y.; et al. Capsaicin-containing chili improved postprandial hyperglycemia, hyperinsulinemia, and fasting lipid disorders in women with gestational diabetes mellitus and lowered the incidence of large-for-gestational-age newborns. Clin. Nutr. 2016, 35, 388–393.
- Chaiyasit, K.; Khovidhunkit, W.; Wittayalertpanya, S. Pharmacokinetic and the effect of capsaicin in Capsicum frutescens on decreasing plasma glucose level. J. Med. Assoc. Thai. 2009, 92, 108–113.
- Janssens, P.L.; Hursel, R.; Martens, E.A.; Westerterp-Plantenga, M.S. Acute effects of capsaicin on energy expenditure and fat oxidation in negative energy balance. PLoS ONE 2013, 8, e67786.
- Janssens, P.L.; Hursel, R.; Westerterp-Plantenga, M.S. Capsaicin increases sensation of fullness in energy balance, and decreases desire to eat after dinner in negative energy balance. Appetite 2014, 77, 44–49.
- Solomon, T.P.; Blannin, A.K. Changes in glucose tolerance and insulin sensitivity following 2 weeks of daily cinnamon ingestion in healthy humans. Eur. J. Appl. Physiol. 2009, 105, 969–976.
- Solomon, T.P.; Blannin, A.K. Effects of short-term cinnamon ingestion on in vivo glucose tolerance. Diabetes Obes. Metab. 2007, 9, 895–901.
- Hlebowicz, J.; Hlebowicz, A.; Lindstedt, S.; Björgell, O.; Höglund, P.; Holst, J.J.; Darwiche, G.; Almér, L.-O. Effects of 1 and 3 g cinnamon on gastric emptying, satiety, and postprandial blood glucose, insulin, glucose-dependent insulinotropic polypeptide, glucagon-like peptide 1, and ghrelin concentrations in healthy subjects. Am. J. Clin. Nutr. 2009, 89, 815–821.
- Markey, O.; McClean, C.M.; Medlow, P.; Davison, G.W.; Trinick, T.R.; Duly, E.; Shafat, A. Effect of cinnamon on gastric emptying, arterial stiffness, postprandial lipemia, glycemia, and appetite responses to high-fat breakfast. Cardiovasc. Diabetol. 2011, 10, 78.
- Magistrelli, A.; Chezem, J.C. Effect of ground cinnamon on postprandial blood glucose concentration in normal-weight and obese adults. J. Acad. Nutr. Diet. 2012, 112, 1806–1809.
- Bernardo, M.A.; Silva, M.L.; Santos, E.; Moncada, M.M.; Brito, J.; Proença, L.; Singh, J.; de Mesquita, M.F. Effect of cinnamon tea on postprandial glucose concentration. J. Diabetes Res. 2015, 2015, 913651.
- Hlebowicz, J.; Darwiche, G.; Björgell, O.; Almér, L.O. Effect of cinnamon on postprandial blood glucose, gastric emptying, and satiety in healthy subjects. Am. J. Clin. Nutr. 2007, 85, 1552–1556.
- Atkinson, F.S.; Stockmann, K.S.; Ek, K.L.; Brand-Miller, J.C. Cassia but not cinnamon reduces postprandial glucose and insulin responses to oatmeal in lean, young adults. Asia Pacific J. Clin. Nutr. 2008, 17, S137.
- Soares, A.P.D.C.; de Faria, N.C.; Graciano, G.F.; Dos Santos, A.L.S.; Valenzuela, V.D.C.; Toulson Davisson Correia, M.I.; Cosenza, G.P.; Anastácio, L.R. Cinnamon infusion reduces satiety and increases energy intake: A randomized crossover trial. Ann. Nutr. Metab. 2022, 78, 265–272.
- Mettler, S.; Schwarz, I.; Colombani, P.C. Additive postprandial blood glucose-attenuating and satiety-enhancing effect of cinnamon and acetic acid. Nutr. Res. 2009, 29, 723–727.
- Vanschoonbeek, K.; Thomassen, B.J.; Senden, J.M.; Wodzig, W.K.; van Loon, L.J. Cinnamon supplementation does not improve glycemic control in postmenopausal type 2 diabetes patients. J. Nutr. 2006, 136, 977–980.
- Sahib, A.S. Anti-diabetic and antioxidant effect of cinnamon in poorly controlled type-2 diabetic Iraqi patients: A randomized, placebo-controlled clinical trial. J. Intercult. Ethnopharmacol. 2016, 5, 108–113.
- Suppapitiporn, S.; Kanpaksi, N.; Suppapitiporn, S. The effect of cinnamon cassia powder in type 2 diabetes mellitus. J. Med. Assoc. Thai. 2006, 89 (Suppl. 3), S200–S205.
- Blevins, S.M.; Leyva, M.J.; Brown, J.; Wright, J.; Scofield, R.H.; Aston, C.E. Effect of cinnamon on glucose and lipid levels in non insulin-dependent type 2 diabetes. Diabetes Care 2007, 30, 2236–2237.
- Talaei, B.; Amouzegar, A.; Sahranavard, S.; Hedayati, M.; Mirmiran, P.; Azizi, F. Effects of cinnamon consumption on glycemic indicators, advanced glycation end products, and antioxidant status in type 2 diabetic patients. Nutrients 2017, 9, 991.
- Mirmiran, P.; Davari, M.; Hashemi, R.; Hedayati, M.; Sahranavard, S.; Bahreini, S.; Tavakoly, R.; Talaei, B. A randomized controlled trial to determining the effect of cinnamon on the plasma levels of soluble forms of vascular adhesion molecules in type 2 diabetes mellitus. Eur. J. Clin. Nutr. 2019, 73, 1605–1612.
- Davari, M.; Hashemi, R.; Mirmiran, P.; Hedayati, M.; Sahranavard, S.; Bahreini, S.; Tavakoly, R.; Talaei, B. Effects of cinnamon supplementation on expression of systemic inflammation factors, NF-kB and sirtuin-1 (SIRT1) in type 2 diabetes: A randomized, double blind, and controlled clinical trial. Nutr. J. 2020, 19, 1.
- Altschuler, J.A.; Casella, S.J.; MacKenzie, T.A.; Curtis, K.M. The effect of cinnamon on A1C among adolescents with type 1 diabetes. Diabetes Care 2007, 30, 813–816.
- Akilen, R.; Tsiami, A.; Devendra, D.; Robinson, N. Glycated haemoglobin and blood pressure-lowering effect of cinnamon in multi-ethnic Type 2 diabetic patients in the UK: A randomized, placebo-controlled, double-blind clinical trial. Diabet. Med. 2010, 27, 1159–1167.
- Wainstein, J.; Stern, N.; Heller, S.; Boaz, M. Dietary cinnamon supplementation and changes in systolic blood pressure in subjects with type 2 diabetes. J. Med. Food 2011, 14, 1505–1510.
- Zahedifar, A.; Khodashenas, M.; Bijari, B.; Zahedifar, F. Effects of cinnamon on fasting blood sugar and hemoglobin A1C in patients with type II diabetes mellitus: A randomized clinical trial. . J. Mazandaran Univ. Med. Sci. 2018, 27, 80–88.
- Zahmatkesh, M.; Fallah Huseini, H.; Hajiaghaee, R.; Heidari, M.; Mehrafarin, A.; Tavakoli-far, B. The effects of Cinnamomum zeylanicum J. Presl on blood glucose level in patients with type 2 diabetes, a double-blind clinical trial. J. Med. Plants 2012, 11 (Suppl. 8), 258–263.
- Mirfeizi, M.; Mehdizadeh Tourzani, Z.; Mirfeizi, S.Z.; Asghari Jafarabadi, M.; Rezvani, H.R.; Afzali, M. Controlling type 2 diabetes mellitus with herbal medicines: A triple-blind randomized clinical trial of efficacy and safety. J. Diabetes. 2016, 8, 647–656.
- Mirmiranpour, H.; Huseini, H.F.; Derakhshanian, H.; Khodaii, Z.; Tavakoli-Far, B. Effects of probiotic, cinnamon, and synbiotic supplementation on glycemic control and antioxidant status in people with type 2 diabetes; a randomized, double-blind, placebo-controlled study. J. Diabetes Metab. Disord. 2019, 19, 53–60.
- Khan, A.; Safdar, M.; Ali Khan, M.M.; Khattak, K.N.; Anderson, R.A. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care 2003, 26, 3215–3218.
- Lira Neto, J.C.G.; Damasceno, M.M.C.; Ciol, M.A.; de Freitas, R.W.J.F.; de Araújo, M.F.M.; Teixeira, C.R.S.; Carvalho, G.C.N.; Lisboa, K.W.S.C.; Marques, R.L.L.; Alencar, A.M.P.G.; et al. Efficacy of cinnamon as an adjuvant in reducing the glycemic biomarkers of type 2 diabetes mellitus: A three-month, randomized, triple-blind, placebo-controlled clinical trial. J. Am. Nutr. Assoc. 2022, 41, 266–274.
- Zare, R.; Nadjarzadeh, A.; Zarshenas, M.M.; Shams, M.; Heydari, M. Efficacy of cinnamon in patients with type II diabetes mellitus: A randomized controlled clinical trial. Clin. Nutr. 2019, 38, 549–556.
- Azimi, P.; Ghiasvand, R.; Feizi, A.; Hosseinzadeh, J.; Bahreynian, M.; Hariri, M.; Khosravi-Boroujeni, H. Effect of cinnamon, cardamom, saffron and ginger consumption on blood pressure and a marker of endothelial function in patients with type 2 diabetes mellitus: A randomized controlled clinical trial. Blood Press. 2016, 25, 133–140.
- Kort, D.H.; Lobo, R.A. Preliminary evidence that cinnamon improves menstrual cyclicity in women with polycystic ovary syndrome: A randomized controlled trial. Am. J. Obstet. Gynecol. 2014, 211, e1–e6.
- Khan, A.A.; Begum, W. Efficacy of Darchini in the management of polycystic ovarian syndrome: A randomized clinical study. J. Herb. Med. 2019, 15, 100249.
- Borzoei, A.; Rafraf, M.; Niromanesh, S.; Farzadi, L.; Narimani, F.; Doostan, F. Effects of cinnamon supplementation on antioxidant status and serum lipids in women with polycystic ovary syndrome. J. Tradit. Complement. Med. 2017, 8, 128–133.
- Borzoei, A.; Rafraf, M.; Asghari-Jafarabadi, M. Cinnamon improves metabolic factors without detectable effects on adiponectin in women with polycystic ovary syndrome. Asia Pac. J. Clin. Nutr. 2018, 27, 556–563.
- Hajimonfarednejad, M.; Nimrouzi, M.; Heydari, M.; Zarshenas, M.M.; Raee, M.J.; Jahromi, B.N. Insulin resistance improvement by cinnamon powder in polycystic ovary syndrome: A randomized double-blind placebo controlled clinical trial. Phytother. Res. 2018, 32, 276–283.
- Dastgheib, M.; Barati-Boldaji, R.; Bahrampour, N.; Taheri, R.; Borghei, M.; Amooee, S.; Mohammadi-Sartang, M.; Wong, A.; Babajafari, S.; Mazloomi, S.M. A comparison of the effects of cinnamon, ginger, and metformin consumption on metabolic health, anthropometric indices, and sexual hormone levels in women with poly cystic ovary syndrome: A randomized double-blinded placebo-controlled clinical trial. Front. Nutr. 2022, 9, 1071515.
- Gupta Jain, S.; Puri, S.; Misra, A.; Gulati, S.; Mani, K. Effect of oral cinnamon intervention on metabolic profile and body composition of Asian Indians with metabolic syndrome: A randomized double -blind control trial. Lipids Health Dis. 2017, 16, 113.
- Askari, F.; Rashidkhani, B.; Hekmatdoost, A. Cinnamon may have therapeutic benefits on lipid profile, liver enzymes, insulin resistance, and high-sensitivity C-reactive protein in nonalcoholic fatty liver disease patients. Nutr. Res. 2014, 34, 143–148.
- Wickenberg, J.; Lindstedt, S.; Berntorp, K.; Nilsson, J.; Hlebowicz, J. Ceylon cinnamon does not affect postprandial plasma glucose or insulin in subjects with impaired glucose tolerance. Br. J. Nutr. 2012, 107, 1845–1849.
- Gutierrez, J.L.; Bowden, R.G.; Willoughby, D.S. Cassia cinnamon supplementation reduces peak blood glucose responses but does not improve insulin resistance and sensitivity in young, sedentary, obese women. J. Diet. Suppl. 2016, 13, 461–471.
- Pishdad, S.; Nadjarzadeh, A.; Salehi Abargouei, A.; Karimi Nazari, E.; Papoli, M. Effect of cumin and cinnamon on lipid profile in middle-aged women with dyslipidemia: A double blind, randomized controlled clinical trial. Progr. Nutr. 2018, 20, 232–237.
- Lee, M.S.; Wahlqvist, M.L.; Chou, Y.C.; Fang, W.H.; Lee, J.T.; Kuan, J.C.; Liu, H.-Y.; Lu, T.-M.; Xiu, L.; Hsu, C.-C.; et al. Turmeric improves post-prandial working memory in pre-diabetes independent of insulin. Asia Pac. J. Clin. Nutr. 2014, 23, 581–591.
- Zeb, F.; Safdar, M.; Fatima, S.; Khan, S.; Alam, S.; Muhammad, M.; Syed, A.; Habib, F.; Shakoor, H. Supplementation of garlic and coriander seed powder: Impact on body mass index, lipid profile and blood pressure of hyperlipidemic patients. Pak. J. Pharm. Sci. 2018, 31, 1935–1941.
- Zare, R.; Heshmati, F.; Fallahzadeh, H.; Nadjarzadeh, A. Effect of cumin powder on body composition and lipid profile in overweight and obese women. Complement. Ther. Clin. Pract. 2014, 20, 297–301.
- Bae, J.; Kim, J.; Choue, R.; Lim, H. Fennel (Foeniculum vulgare) and fenugreek (Trigonella foenum-graecum) tea drinking suppresses subjective short-term appetite in overweight women. Clin. Nutr. Res. 2015, 4, 168–174.
- Kiss, R.; Szabó, K.; Gesztelyi, R.; Somodi, S.; Kovács, P.; Szabó, Z.; Németh, J.; Priksz, D.; Kurucz, A.; Juhász, B.; et al. Insulin-sensitizer effects of fenugreek seeds in parallel with changes in plasma MCH levels in healthy volunteers. Int. J. Mol. Sci. 2018, 19, 771.
- Gopalpura, P.B.; Jayanthi, C.; Dubey, S. Effect of Trigonella foenum-graecum seeds on the glycemic index of food: A clinical evaluation. Int. J. Diabetes Dev. Ctries. 2007, 27, 41–45.
- Robert, S.D.; Ismail, A.A.; Rosli, W.I. Reduction of postprandial blood glucose in healthy subjects by buns and flatbreads incorporated with fenugreek seed powder. Eur. J. Nutr. 2016, 55, 2275–2280.
- Sharma, R.D.; Raghuram, T.C.; Rao, N.S. Effect of fenugreek seeds on blood glucose and serum lipids in type I diabetes. Eur. J. Clin. Nutr. 1990, 44, 301–306.
- Madar, Z.; Abel, R.; Samish, S.; Arad, J. Glucose-lowering effect of fenugreek in non-insulin dependent diabetics. Eur. J. Clin. Nutr. 1988, 42, 51–54.
- Kassaian, N.; Azadbakht, L.; Forghani, B.; Amini, M. Effect of fenugreek seeds on blood glucose and lipid profiles in type 2 diabetic patients. Int. J. Vitam. Nutr. Res. 2009, 79, 34–39.
- Losso, J.N.; Holliday, D.L.; Finley, J.W.; Martin, R.J.; Rood, J.C.; Yu, Y.; Greenway, F.L. Fenugreek bread: A treatment for diabetes mellitus. J. Med. Food. 2009, 12, 1046–1049.
- Najdi, R.A.; Hagras, M.M.; Kamel, F.O.; Magadmi, R.M. A randomized controlled clinical trial evaluating the effect of Trigonella foenum-graecum (fenugreek) versus glibenclamide in patients with diabetes. Afr. Health Sci. 2019, 19, 1594–1601.
- Tavakoly, R.; Maracy, M.R.; Karimifar, M.; Entezari, M.H. Does fenugreek (Trigonella foenum-graecum) seed improve inflammation, and oxidative stress in patients with type 2 diabetes mellitus? A parallel group randomized clinical trial. Eur. J. Integr. Med. 2018, 18, 13–17.
- Sharma, R.D.; Sarkar, A.; Hazra, D.K.; Misra, B.; Singh, J.B.; Maheshwari, B.B.; Sharma, S.K. Hypolipidaemic effect of fenugreek seeds: A chronic study in non-insulin dependent diabetic patients. Phytother. Res. 1996, 10, 332–334.
- Bhadauria, S.S.; Kushwah, A. Fenugreek seeds as a therapeutic supplement for patients with noninsulin dependent diabetes mellitus: A cross-sectional study. J. Clin. Diagn. Res. 2021, 15, BC21–BC23.
- Hadi, A.; Arab, A.; Hajianfar, H.; Talaei, B.; Miraghajani, M.; Babajafari, S.; Marx, W.; Tavakoly, R. The effect of fenugreek seed supplementation on serum irisin levels, blood pressure, and liver and kidney function in patients with type 2 diabetes mellitus: A parallel randomized clinical trial. Complement. Ther. Med. 2020, 49, 102315.
- Geberemeskel, G.A.; Debebe, Y.G.; Nguse, N.A. Antidiabetic effect of fenugreek seed powder solution (Trigonella foenum-graecum L.) on hyperlipidemia in diabetic patients. J. Diabetes Res. 2019, 2019, 8507453.
- Rafraf, M.; Malekiyan, M.; Asghari-Jafarabadi, M.; Aliasgarzadeh, A. Effect of fenugreek seeds on serum metabolic factors and adiponectin levels in type 2 diabetic patients. Int. J. Vitam. Nutr. Res. 2014, 84, 196–205.
- Hassani, S.S.; Arezodar, F.F.; Esmaeili, S.S.; Gholami-Fesharaki, M. The effect of combined therapy with fenugreek and nutrition training based on iranian traditional medicine on FBS, HGA1C, BMI, and waist circumference in type 2 diabetic patients: A randomized double-blinded clinical trial. J. Adv. Med. Biomed. Res. 2019, 27, 37–42.
- Hassani, S.S.; Fallahi Arezodar, F.; Esmaeili, S.S.; Gholami-Fesharaki, M. Effect of fenugreek use on fasting blood glucose, glycosylated hemoglobin, body mass index, waist circumference, blood pressure and quality of life in patients with type 2 diabetes mellitus: A randomized, double-blinded, placebo-controlled clinical trials. Galen. Med. J. 2019, 8, e1432.
- Sharma, R.D. Effect of fenugreek seeds and leaves on blood glucose and serum insulin responses in human subjects. Nutr. Res. 1986, 6, 1353–1364.
- Bordia, A.; Verma, S.K.; Srivastava, K.C. Effect of ginger (Zingiber officinale Rosc.) and fenugreek (Trigonella foenumgraecum L.) on blood lipids, blood sugar and platelet aggregation in patients with coronary artery disease. Prostaglandins Leukot. Essent. Fatty Acids. 1997, 56, 379–384.
- Sowmya, P.; Rajyalakshmi, P. Hypocholesterolemic effect of germinated fenugreek seeds in human subjects. Plant Foods Hum. Nutr. 1999, 53, 359–365.
- Yousefi, E.; Zareiy, S.; Zavoshy, R.; Noroozi, M.; Jahanihashemi, H.; Ardalani, H. Fenugreek: A therapeutic complement for patients with borderline hyperlipidemia: A randomised, double-blind, placebo-controlled, clinical trial. Adv. Integr. Med. 2017, 4, 31–35.
- Choudhary, P.R.; Jani, R.D.; Sharma, M.S. Effect of raw crushed garlic (Allium sativum L.) on components of metabolic syndrome. J. Diet Suppl. 2018, 15, 499–506.
- Aslani, N.; Entezari, M.H.; Askari, G.; Maghsoudi, Z.; Maracy, M.R. Effect of garlic and lemon juice mixture on lipid profile and some cardiovascular risk factors in people 30–60 years old with moderate hyperlipidaemia: A randomized clinical trial. Int. J. Prev. Med. 2016, 7, 95.
- van Doorn, M.B.; Espirito Santo, S.M.; Meijer, P.; Kamerling, I.M.; Schoemaker, R.C.; Dirsch, V.; Vollmar, A.; Haffner, T.; Gebhardt, R.; Cohen, A.F.; et al. Effect of garlic powder on C-reactive protein and plasma lipids in overweight and smoking subjects. Am. J. Clin. Nutr. 2006, 84, 1324–1329.
- Scharbert, G.; Kalb, M.L.; Duris, M.; Marschalek, C.; Kozek-Langenecker, S.A. Garlic at dietary doses does not impair platelet function. Anesth. Analg. 2007, 105, 1214–1218.
- Bakhsh, R.; Chughtai, M.I. Influence of garlic on serum cholesterol, serum triglycerides, serum total lipids and serum glucose in human subjects. Food/Nahrung 1984, 28, 159–163.
- Roberts, K.; Jahner, D.K.W.; Buddington, R.K. Influence of garlic supplementation on human fecal flora and serum lipid levels. FASEB J. 1998, 12, A876.
- Charron, C.S.; Dawson, H.D.; Albaugh, G.P.; Solverson, P.M.; Vinyard, B.T.; Solano-Aguilar, G.I.; Molokin, A.; Novotny, J.A. A single meal containing raw, crushed garlic influences expression of immunity- and cancer-related genes in whole blood of humans. J. Nutr. 2015, 145, 2448–2455.
- Sangouni, A.A.; Alizadeh, M.; Jamalzehi, A.; Parastouei, K. Effects of garlic powder supplementation on metabolic syndrome components, insulin resistance, fatty liver index, and appetite in subjects with metabolic syndrome: A randomized clinical trial. Phytother. Res. 2021, 35, 4433–4441.
- Sangouni, A.A.; Mohammad Hosseini Azar, M.R.; Alizadeh, M. Effects of garlic powder supplementation on insulin resistance, oxidative stress, and body composition in patients with non-alcoholic fatty liver disease: A randomized controlled clinical trial. Complement. Ther. Med. 2020, 51, 102428.
- Sangouni, A.A.; Mohammad Hosseini Azar, M.R.; Alizadeh, M. Effect of garlic powder supplementation on hepatic steatosis, liver enzymes and lipid profile in patients with non-alcoholic fatty liver disease: A double-blind randomised controlled clinical trial. Br. J. Nutr. 2020, 124, 450–456.
- Janssen, P.L.; Meyboom, S.; van Staveren, W.A.; de Vegt, F.; Katan, M.B. Consumption of ginger (Zingiber officinale roscoe) does not affect ex vivo platelet thromboxane production in humans. Eur. J. Clin. Nutr. 1996, 50, 772–774.
- Miyamoto, M.; Matsuzaki, K.; Katakura, M.; Hara, T.; Tanabe, Y.; Shido, O. Oral intake of encapsulated dried ginger root powder hardly affects human thermoregulatory function, but appears to facilitate fat utilization. Int. J. Biometeorol. 2015, 59, 1461–1474.
- Mansour, M.S.; Ni, Y.M.; Roberts, A.L.; Kelleman, M.; Roychoudhury, A.; St-Onge, M.P. Ginger consumption enhances the thermic effect of food and promotes feelings of satiety without affecting metabolic and hormonal parameters in overweight men: A pilot study. Metabolism 2012, 61, 1347–1352.
- Ebrahimzadeh Attari, V.; Asghari Jafarabadi, M.; Zemestani, M.; Ostadrahimi, A. Effect of Zingiber officinale supplementation on obesity management with respect to the uncoupling protein 1 -3826A>G and ß3-adrenergic receptor Trp64Arg polymorphism. Phytother. Res. 2015, 29, 1032–1039.
- Ebrahimzadeh Attari, V.; Ostadrahimi, A.; Asghari Jafarabadi, M.; Mehralizadeh, S.; Mahluji, S. Changes of serum adipocytokines and body weight following Zingiber officinale supplementation in obese women: A RCT. Eur. J. Nutr. 2016, 55, 2129–2136.
- Ebrahimzadeh Attari, V.; Mahluji, S.; Asghari Jafarabadi, M.; Ostadrahimi, A. Effects of supplementation with ginger (Zingiber officinale Roscoe) on serum glucose, lipid profile and oxidative stress in obese women: A randomized, placebo-controlled clinical trial. Pharm. Sci. 2015, 21, 184–191.
- Mahluji, S.; Attari, V.E.; Mobasseri, M.; Payahoo, L.; Ostadrahimi, A.; Golzari, S.E. Effects of ginger (Zingiber officinale) on plasma glucose level, HbA1c and insulin sensitivity in type 2 diabetic patients. Int. J. Food Sci. Nutr. 2013, 64, 682–686.
- Carvalho, G.C.N.; Lira-Neto, J.C.G.; Araújo, M.F.M.; Freitas, R.W.J.F.; Zanetti, M.L.; Damasceno, M.M.C. Effectiveness of ginger in reducing metabolic levels in people with diabetes: A randomized clinical trial. Rev. Lat. Am. Enfermagem. 2020, 28, e3369.
- Khandouzi, N.; Shidfar, F.; Rajab, A.; Rahideh, T.; Hosseini, P.; Mir Taheri, M. The effects of ginger on fasting blood sugar, hemoglobin a1c, apolipoprotein B, apolipoprotein a-I and malondialdehyde in type 2 diabetic patients. Iran. J. Pharm. Res. 2015, 14, 131–140.
- Mahluji, S.; Ostadrahimi, A.; Mobasseri, M.; Ebrahimzade Attari, V.; Payahoo, L. Anti-inflammatory effects of Zingiber officinale in type 2 diabetic patients. Adv. Pharm. Bull. 2013, 3, 273–276.
- Arablou, T.; Aryaeian, N.; Valizadeh, M.; Sharifi, F.; Hosseini, A.; Djalali, M. The effect of ginger consumption on glycemic status, lipid profile and some inflammatory markers in patients with type 2 diabetes mellitus. Int. J. Food Sci. Nutr. 2014, 65, 515–520.
- Mozaffari-Khosravi, H.; Talaei, B.; Jalali, B.A.; Najarzadeh, A.; Mozayan, M.R. The effect of ginger powder supplementation on insulin resistance and glycemic indices in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Complement. Ther. Med. 2014, 22, 9–16.
- Hajimoosayi, F.; Jahanian Sadatmahalleh, S.; Kazemnejad, A.; Pirjani, R. Effect of ginger on the blood glucose level of women with gestational diabetes mellitus (GDM) with impaired glucose tolerance test (GTT): A randomized double-blind placebo-controlled trial. BMC Complement. Med. Ther. 2020, 20, 116.
- Shidfar, F.; Rajab, A.; Rahideh, T.; Khandouzi, N.; Hosseini, S.; Shidfar, S. The effect of ginger (Zingiber officinale) on glycemic markers in patients with type 2 diabetes. J. Complement. Integr. Med. 2015, 12, 165–170.
- Zarezadeh, M.; Saedisomeolia, A.; Khorshidi, M.; Kord Varkane, H.; Makhdoomi Arzati, M.; Abdollahi, M.; Yekaninejad, M.S.; Hashemi, R.; Effatpanah, M.; Honarvar, N.M. Asymmetric dimethylarginine and soluble inter-cellular adhesion molecule-1 serum levels alteration following ginger supplementation in patients with type 2 diabetes: A randomized double-blind, placebo-controlled clinical trial. J. Complement. Integr. Med. 2018, 16, 20180019.
- Mohammadzadeh Honarvar, N.; Zarezadeh, M.; Khorshidi, M.; Makhdoomi Arzati, M.; Yekaninejad, M.S.; Abdollahi, M.; Effatpanah, M.; Hashemi, R.; Saedisomeolia, A. The effect of an oral ginger supplementation on NF-κB concentration in peripheral blood mononuclear cells and anthropomorphic data of patients with type 2 diabetes: A randomized double-blind, placebo-controlled clinical trial. Complement. Ther. Med. 2019, 42, 7–11.
- Alizadeh-Navaei, R.; Roozbeh, F.; Saravi, M.; Pouramir, M.; Jalali, F.; Moghadamnia, A.A. Investigation of the effect of ginger on the lipid levels. A double blind controlled clinical trial. Saudi Med. J. 2008, 29, 1280–1284.
- Kamari, N.; Moradinazar, M.; Qasemi, M.; Khosravy, T.; Samadi, M.; Abdolahzad, H. Combination of the effect of ginger and anti-inflammatory diet on children with obesity with nonalcoholic fatty liver disease: A randomized clinical trial. Food Sci. Nutr. 2023, 11, 1846–1859.
- Rafie Hosseini, S.A.; Hajiani, E.; Saki Malehi, A.; Mard, S.A. Effect of ginger powder supplementation in patients with non-alcoholic fatty liver disease: A randomized clinical trial. Clin. Exp. Gastroenterol. 2020, 13, 35–45.
- Ashraf, H.; Heydari, M.; Shams, M.; Zarshenas, M.M.; Tavakoli, A.; Sayadi, M. Efficacy of ginger supplementation in relieving persistent hypothyroid symptoms in patients with controlled primary hypothyroidism: A pilot randomized, double-blind, placebo-controlled clinical trial. Evid. Based Complement. Alt. Med. 2022, 2022, 5456855.
- Pelegrin, S.; Galtier, F.; Chalançon, A.; Gagnol, J.P.; Barbanel, A.M.; Pélissier, Y.; Larroque, M.; Lepape, S.; Faucanié, M.; Gabillaud, I.; et al. Effects of Nigella sativa seeds (black cumin) on insulin secretion and lipid profile: A pilot study in healthy volunteers. Br. J. Clin. Pharmacol. 2019, 85, 1607–1611.
- Amin, F.; Islam, N.; Anila, N.; Gilani, A.H. Clinical efficacy of the co-administration of Turmeric and Black seeds (Kalongi) in metabolic syndrome—A double blind randomized controlled trial—TAK-MetS trial. Complement. Ther. Med. 2015, 23, 165–174.
- Datau, E.A.; Wardhana Surachmanto, E.E.; Pandelaki, K.; Langi, J.A. Efficacy of Nigella sativa on serum free testosterone and metabolic disturbances in central obese male. Acta Med. Indones. 2010, 42, 130–134.
- Farhangi, M.A.; Dehghan, P.; Tajmiri, S.; Abbasi, M.M. The effects of Nigella sativa on thyroid function, serum vascular endothelial growth factor (VEGF)-1, Nesfatin-1 and anthropometric features in patients with Hashimoto’s thyroiditis: A randomized controlled trial. BMC Complement. Altern. Med. 2016, 16, 471.
- Farhangi, M.A.; Tajmiri, S. The effects of powdered black cumin seeds on markers of oxidative stress, intracellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM)-1 in patients with Hashimoto’s thyroiditis. Clin. Nutr. ESPEN 2020, 37, 207–212.
- Mohtashami, A. Effects of bread with Nigella Sativa on blood glucose, blood pressure and anthropometric indices in patients with metabolic syndrome. Clin. Nutr. Res. 2019, 8, 138–147.
- Mohtashami, A.; Mahaki, B.; Azadbakht, L.; Entezari, M.H. Effects of bread with Nigella sativa on lipid profiles, apolipoproteins and inflammatory factor in metabolic syndrome patients. Clin. Nutr. Res. 2016, 5, 89–95.
- Ibrahim, R.M.; Hamdan, N.S.; Ismail, M.; Saini, S.M.; Abd Rashid, S.N.; Abd Latiff, L.; Mahmud, R. Protective effects of Nigella sativa on metabolic syndrome in menopausal women. Adv. Pharm. Bull. 2014, 4, 29–33.
- Shirazi, M.; Khodakarami, F.; Feizabad, E.; Ghaemi, M. The effects of Nigella sativa on anthropometric and biochemical indices in postmenopausal women with metabolic syndrome. Endocrine 2020, 69, 49–52.
- Ibrahim, R.M.; Hamdan, N.S.; Mahmud, R.; Imam, M.U.; Saini, S.M.; Rashid, S.N.; Ghafar, S.A.; Latiff, L.A.; Ismail, M. A randomised controlled trial on hypolipidemic effects of Nigella sativa seeds powder in menopausal women. J. Transl. Med. 2014, 12, 82.
- Qidwai, W.; Hamza, H.B.; Qureshi, R.; Gilani, A. Effectiveness, safety, and tolerability of powdered Nigella sativa (kalonji) seed in capsules on serum lipid levels, blood sugar, blood pressure, and body weight in adults: Results of a randomized, double-blind controlled trial. J. Altern. Complement. Med. 2009, 15, 639–644.
- Sabzghabaee, A.M.; Dianatkhah, M.; Sarrafzadegan, N.; Asgary, S.; Ghannadi, A. Clinical evaluation of Nigella sativa seeds for the treatment of hyperlipidemia: A randomized, placebo controlled clinical trial. Med. Arch. 2012, 66, 198–200.
- Bamosa, A.O.; Kaatabi, H.; Lebdaa, F.M.; Elq, A.M.; Al-Sultanb, A. Effect of Nigella sativa seeds on the glycemic control of patients with type 2 diabetes mellitus. Indian J. Physiol. Pharmacol. 2010, 54, 344–354.
- Badar, A.; Kaatabi, H.; Bamosa, A.; Al-Elq, A.; Abou-Hozaifa, B.; Lebda, F.; Alkhadra, A.; Al-Almaie, S. Effect of Nigella sativa supplementation over a one-year period on lipid levels, blood pressure and heart rate in type-2 diabetic patients receiving oral hypoglycemic agents: Nonrandomized clinical trial. Ann. Saudi Med. 2017, 37, 56–63.
- Kaatabi, H.; Bamosa, A.O.; Badar, A.; Al-Elq, A.; Abou-Hozaifa, B.; Lebda, F.; Al-Khadra, A.; Al-Almaie, S. Nigella sativa improves glycemic control and ameliorates oxidative stress in patients with type 2 diabetes mellitus: Placebo controlled participant blinded clinical trial. PLoS ONE 2015, 10, e0113486.
- Darand, M.; Darabi, Z.; Yari, Z.; Saadati, S.; Hedayati, M.; Khoncheh, A.; Hosseini-Ahangar, B.; Alavian, S.M.; Hekmatdoost, A. Nigella sativa and inflammatory biomarkers in patients with non-alcoholic fatty liver disease: Results from a randomized, double-blind, placebo-controlled, clinical trial. Complement. Ther. Med. 2019, 44, 204–209.
- Darand, M.; Darabi, Z.; Yari, Z.; Hedayati, M.; Shahrbaf, M.A.; Khoncheh, A.; Hosseini-Ahangar, B.; Alavian, S.M.; Hekmatdoost, A. The effects of black seed supplementation on cardiovascular risk factors in patients with nonalcoholic fatty liver disease: A randomized, double-blind, placebo-controlled clinical trial. Phytother. Res. 2019, 33, 2369–2377.
- Akbari, S.; Sohouli, M.H.; Ebrahimzadeh, S.; Ghanaei, F.M.; Hosseini, A.F.; Aryaeian, N. Effect of rosemary leaf powder with weight loss diet on lipid profile, glycemic status, and liver enzymes in patients with nonalcoholic fatty liver disease: A randomized, double-blind clinical trial. Phytother. Res. 2022, 36, 2186–2196.
- Sá, C.M.; Ramos, A.A.; Azevedo, M.F.; Lima, C.F.; Fernandes-Ferreira, M.; Pereira-Wilson, C. Sage tea drinking improves lipid profile and antioxidant defences in humans. Int. J. Mol. Sci. 2009, 10, 3937–3950.
- Darmian, M.A.; Hoseini, R.; Amiri, E.; Golshani, S. How combined and separate aerobic training and turmeric supplementation alter lipid profile and glycemic status? A clinical trial in middle-aged females with type 2 diabetes and hyperlipidemia. Int. Cardiovasc. Res. J. 2021, 15, e118791.
- Maithili Karpaga Selvi, N.; Sridhar, M.G.; Swaminathan, R.P.; Sripradha, R. Efficacy of turmeric as adjuvant therapy in type 2 diabetic patients. Indian J. Clin. Biochem. 2015, 30, 180–186.
- Darmian, M.A.; Hoseini, R.; Amiri, E.; Golshani, S. Downregulated hs-CRP and MAD, upregulated GSH and TAC, and improved metabolic status following combined exercise and turmeric supplementation: A clinical trial in middle-aged women with hyperlipidemic type 2 diabetes. J. Diabetes Metab. Disord. 2022, 21, 275–283.
- Adab, Z.; Eghtesadi, S.; Vafa, M.R.; Heydari, I.; Shojaii, A.; Haqqani, H.; Arablou, T.; Eghtesadi, M. Effect of turmeric on glycemic status, lipid profile, hs-CRP, and total antioxidant capacity in hyperlipidemic type 2 diabetes mellitus patients. Phytother. Res. 2019, 33, 1173–1181.
- Srinivasan, A.; Selvarajan, S.; Kamalanathan, S.; Kadhiravan, T.; Prasanna Lakshmi, N.C.; Adithan, S. Effect of Curcuma longa on vascular function in native Tamilians with type 2 diabetes mellitus: A randomized, double-blind, parallel arm, placebo-controlled trial. Phytother. Res. 2019, 33, 1898–1911.
- Wickenberg, J.; Ingemansson, S.L.; Hlebowicz, J. Effects of Curcuma longa (turmeric) on postprandial plasma glucose and insulin in healthy subjects. Nutr. J. 2010, 9, 43.
- Nieman, D.C.; Cialdella-Kam, L.; Knab, A.M.; Shanely, R.A. Influence of red pepper spice and turmeric on inflammation and oxidative stress biomarkers in overweight females: A metabolomics approach. Plant Foods Hum. Nutr. 2012, 67, 415–421.
- Navekar, R.; Rafraf, M.; Ghaffari, A.; Asghari-Jafarabadi, M.; Khoshbaten, M. Turmeric supplementation improves serum glucose indices and leptin levels in patients with nonalcoholic fatty liver diseases. J. Am. Coll. Nutr. 2017, 36, 261–267.
- Jarhahzadeh, M.; Alavinejad, P.; Farsi, F.; Husain, D.; Rezazadeh, A. The effect of turmeric on lipid profile, malondialdehyde, liver echogenicity and enzymes among patients with nonalcoholic fatty liver disease: A randomized double blind clinical trial. Diabetol. Metab. Syndr. 2021, 13, 112.
More
