Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Toncho Dinev and Version 2 by Camila Xu.
The union of aquaculture and hydroponics is named aquaponics—a system where microorganisms, fish and plants coexist in a water environment. Bacteria are essential in processes which are fundamental for the functioning and equilibrium of aquaponic systems.
- pathogenic bacteria
- yeasts
- molds
- aquaponics
- human health
1. Introduction
The rapid increase in world population has led to several challenges, such as water scarcity, degradation of arable land, and climate change, which in turn affects food production. However, conventional agriculture is renowned for requiring a large amount of water and land and high nutrient intake. Crops are also more likely to be infected by soil-borne diseases as a result of cultivation that also degrades the quality of the soil. To bridge the mismatch between resource availability and food demand, a shift from an infinite growth-based economic model to balanced and sustainable food production methods to ensure food security is required [1][2][1,2].
The Food and Agriculture Organization of the United Nations (FAO) defines aquaculture as the cultivation of aquatic organisms in both fresh and salt water under controlled conditions. On the other hand, hydroponics is the cultivation of plants without the use of soil, in which the nutrients necessary for the growth of the plants are supplied through an aqueous solution. The union of aquaculture and hydroponics is a comparatively new technology named aquaponics [3]. An aquaponic system could be either coupled or decoupled. A coupled system is designed so that water returns to the fish tank following plant irrigation. In decoupled system the produce irrigation water does not return to the fish tank [4]. Compared to soil-based farms, hydroponic cropping systems are not restricted by climate or location, better utilize vertical spaces, save approximately 90% irrigation water, and can supply fruit and vegetables to surrounding communities year-round. In addition, hydroponically grown plants have a higher yield and amount of some bioactive compounds than conventionally grown ones. On the other hand, freshwater fish excrete nutrients in their gills, urine, and feces waste streams, many of which are essential for plant growth and development in aquaponic systems. Thus, hydroponics and aquaponics are viewed as a promising solution for feeding the growing global population [1][5][6][1,5,6]. In addition to coupled aquaponics, the recent trends showed an increasing focus on the development of inland saline and marine aquaponics as the future of this farming system [7].
Although aquaponics is an innovative system, aquaponic products are already commercially available in many countries such as the USA, the UK, Canada, Australia, Israel, Philippines, Italy, India, South Africa, Uganda, Hungary, Portugal, Oman, China, Brazil, Ghana, Malaysia, Malta, Mauritius, and Japan. The most commonly raised aquatic animals by percentage are tilapia (Tilapia spp.), ornamental fish, catfish (order Siluriformes), other aquatic animals (such as shrimp and prawns, suborder Dendrobranchiata, and crayfish, Astacoidea and Parastacoidea families), perch (Perca spp.), bluegill (Lepomis macrochirus) trout (Oncorhynchus spp., Salmo spp., Salvenlius spp.), bass (Micropterus spp., Morone spp.), carp (Cyprinidae family), and other fish. The most frequently raised plants among commercial producers are basil, salad greens, non-basil herbs, tomatoes, head lettuce, peppers, cucumber, and other plants [8].
Along with plants and fish, microorganisms are also present in aquaponics. Bacteria are key players in processes which are fundamental for the functioning and equilibrium of aquaponic systems. For example, the process of nitrification is carried out mainly by ammonia-oxidizing and nitrite-oxidizing bacteria. Microorganisms can also contribute to the extraction of various macro- and micronutrients from the feed leftovers and solid feces and make them available for plant intake [9]. Also, aquaponics can be similar to soil production in terms of microbial communities [10]. However, in aquaponic systems there are not only beneficial, but also potentially harmful microorganisms of fish, human, and plant origin. In this respect, a coupled aquaponic system is a potential risk factor because the water circulates in the system, thus providing a perfect environment for waste accumulation, leading to continuous microbial and parasitic growth, i.e., outbreak of diseases [6]. The removal of pathogens is difficult if no mitigation methods are established. These methods are restricted in aquaponic systems because if they are able to reduce pathogenic microbial load, they are likely to reduce beneficial microbial load as well. Nevertheless, potential mitigation methods that can help reduce the pathogenic microbial loads, such as UV irradiation, ozonation, and filtration, have been explored [4].
The term “zoonosis” refers to a disease that can be transferred from animals to humans. Human infections caused by pathogens transmitted from fish or the aquatic environment are quite common and depend on the season, the patient’s contact with fish, and the associated environment, dietary habits, and state of the immune system of the exposed individual [11]. Such zoonotic infections can be divided into two categories: first, foodborne infections caused by eating raw or undercooked fish and ingesting water or other substances contaminated with infected fish feces/mucus and second, topically acquired infections caused by contact with fish pathogens through open wounds or skin scratches/abrasions [12][13][12,13]. Each year in the United States approximately 260,000 people get sick from contaminated fish. In the period between 1998 and 2015, a review on the data of the Centers of Disease Control and Prevention of the United States found 857 foodborne disease outbreaks associated with fish, resulting in 4814 illnesses, 359 hospitalizations, and four deaths. Most hospitalizations were caused by Salmonella spp. (31%) and ciguatoxin (31%) [14].
Many plant pathogens exist, but until recently the ability of plant pathogens to cause disease in humans and animals was thought to be of little importance. However, recent evidence suggests that animal and human infections caused by plant pathogens (bacteria, viruses, and fungi) may have critical impacts on human and animal health and safety. In the majority of cases, such infections result from infection through damaged skin or the respiratory tract, or were infections of immunocompromised individuals. As such, infections by phytopathogens can generally be considered opportunistic [15]. In the last several decades, multiple foodborne disease outbreaks have been traced back to the pre-harvest period contamination of fresh plant produce. In the period between 1973 and 2012, the Centers for Disease Control and Prevention of the United States received report of 606 leafy vegetable-associated outbreaks, with 20003 associated illnesses, 1030 hospitalizations, and 19 deaths. The pathogens most commonly causing leafy vegetable-associated outbreaks were norovirus (55% of outbreaks with confirmed etiology), Shiga toxin-producing Escherichia coli (18%) and Salmonella spp. (11%) [16].
2. Microbial Pathogens in Aquaponic Systems
2.1. Bacteria
Bacteria are considered the main zoonotic agents of fish [10]. However, farmed aquatic species are poikilothermic with a labile body temperature dependent on the environment temperature. Their body temperature is generally too low to be considered optimal for the proliferation of most intestinal bacteria likely to infect humans because they prefer the body temperature of homeotherms [17]. Nevertheless, the rearing of species such as tilapia (Oreochromis niloticus) could allow the proliferation of introduced human pathogens because of the warm temperatures (28–30 °C) required for the optimal growth of these species [18]. However, the recent literature data included a case of an increasing count of E. coli, coliforms, Enterobacteriaceae, and Salmonella spp. from the beginning of the trials to their end while the temperature of the water was 18 °C [19]. These findings suggest that the restrictive effect of water temperature on the proliferation of intestinal bacteria is not absolute. In this respect, Lee et al. [20] found that if E. coli is provided with adequate nutrients, it is still able to grow at temperature as low as 15 °C, but at a reduced rate. Also, in the last years there have been a lot of data suggesting the increasing role of E. coli and coliforms in aquaponic systems [4][19][21][4,19,21]. There are hundreds of types of non-fecal coliform bacteria in the air, water, and soil, as well as fecal coliform bacteria represented mostly by E. coli in the waste of all humans, mammals, and some birds. If present in aquaponic systems, indicator and pathogenic bacteria, such as E. coli and Salmonella spp., most likely originate from warm-blooded animals and humans, since these enteric bacteria are transient in fish gut microflora (Table 1) [22]. However, the vast majority of these coliforms are completely harmless [23]. Nevertheless, coliforms such as E. coli and Klebsiella, and members of Salmonella are known as zoonotic agents of fish. They usually cause topically acquired and/or systemic infections in humans through contact via open wounds, touching fish, or skin scratches, or through foodborne infections via consumption of Salmonella-contaminated fish [13]. Because of their high pathogenic potential, the presence of Salmonella spp. in aquaponic water is considered highly hazardous. It should be noted that the subspecies of Salmonella found in the environment and cold-blooded animals are rare in humans. The four different clinical manifestations of human salmonella infection are enteric fever, gastroenteritis, bacteremia and other extraintestinal complications, and a chronic carrier state [24]. According to the World Health Organization (WHO), Salmonella belongs to the list of high priority pathogens which lists pathogens for which new antibiotics are urgently needed. Salmonella is resistant to fluoroquinolones [25]. Klebsiella spp. are found ubiquitously in nature, including in plants, animals, and humans. They cause several types of infections in humans, including respiratory tract infections, urinary tract infections, and bloodstream infections [26]. K. pneumoniae, one of the most important species of this genus with pathogenic potential, is not only a highly dangerous opportunistic human pathogen but in the last decades many strains of this bacterium demonstrated multidrug resistance, extensive drug resistance, and pandrug resistance, making the treatment of K. pneumoniae infections a real challenge. According to the WHO, Klebsiella belongs to the most critical group of pathogens for which new antibiotics are urgently needed. Klebsiella is carbapenem-resistant and ESBL-producing [25][27][28][25,27,28]. Moreover, K. pneumoniae is a fish pathogen infecting various fish species, including Nile tilapia (Oreochromis niloticus), ornamental Nishikigoi carp (Cyprinus carpio), and Indian major carp (Labeo rohita). [29][30][29,30]. It is established that poor worker hygiene practices can lead to the infiltration of various microorganisms, including pathogens, into aquaponic systems. For example, if the workers of these farms do not switch shoes when entering the farm, even if the sanitizer sink is presented at the entrance it may not eliminate the risk of introducing contaminants from the open environment [6]. The discovery of E. coli in these systems is not necessarily a human health hazard because most of the strains of this bacterium are harmless or opportunistic. This, however, is not the case with Shiga toxin-producing E. coli which are found by Wang et al. [21] in aquaponic water. In humans, this bacterium can cause bloody diarrhea, stomach cramps, and vomiting followed by a serious sequela, hemolytic uremic syndrome (HUS), a condition characterized by thrombocytopenia, hemolytic anemia, and kidney failure [31]. Moreover, although E. coli is intrinsically susceptible to almost all clinically relevant antimicrobial agents, this bacterium has a great capacity to accumulate resistance genes, mostly through horizontal gene transfer resulting in multidrug resistance. Therefore, in the WHO list, E. coli belongs to the first priority critical group of pathogens for which new antibiotics are urgently needed. E. coli is carbapenem-resistant and ESBL-producing [25][32][25,32]. The human health hazards are especially serious when considering the potential for internalization of E. coli (including E. coli O157:H7) and Salmonella spp. that has been demonstrated in lettuce, spinach, and tomatoes grown in an inoculated hydroponic system [33][34][35][36][33,34,35,36]. However, Macarisin et al. [36] found that experimental contamination of spinach plants grown in soil resulted in a greater number of internalization events than in those grown hydroponically, suggesting that E. coli O157:H7 internalization depends on root damage, which is more likely to occur when plants are grown in soil. This hypothesis is supported by the fact that injury to the root system in hydroponically grown spinach increased the frequency of E. coli O157:H7 internalization [36]. Generally, the pathogens could penetrate the plant through the stomata, the roots and the damaged skin surface. Thus, the fact that the edible part of the plant is not exposed to fish feces in an aquaponic system is of paramount importance. Even if an aquaponically grown plant containing internalized pathogens is taken for consumption, disease is unlikely to follow because the roots containing the pathogens are usually removed [22]. This is a very important food safety advantage of plants grown in aquaponics compared to those grown in soil. Contrary to the aforementioned experiments, Wang et al. [21] did not find the presence of Salmonella spp. and Listeria monocytogenes in aquaponic water and the contaminated water did not lead to internalization of Shiga toxin-producing E. coli into the roots, leaves, and fruit of the lettuce, basil, and tomato plants studied. Also, while some authors reported the presence of E. coli and Salmonella in aquaponic systems [19][37][19,37], others did not find them [6][21][6,21]. Several investigations did not find one or more of the dangerous human pathogens E. coli O157:H7, Salmonella spp., and L. monocytogenes in aquaponic systems [6][22][38][6,22,38]. The abovementioned differences found in the various studies are probably due to the hygiene and the disease prevention practices applied in the different aquaponic systems. Plesiomonas spp., the existence of which are found in aquaponics (Table 1), are recently re-categorized from the Vibrionaceae family to the Enterobacteriaceae family, in which it is the only oxidase-positive member. Plesiomonas shigelloides most often causes enteritis in humans while the other illnesses associated with this bacterium include septicemia and central nervous system disease, eye infections, and a variety of miscellaneous ailments. The highest number of cases of P. shigelloides enteritis are reported in Southeast Asia and Africa. This bacterium is highly pathogenic to farmed fish [39][40][39,40]. Shigella sonnei, an important member of Enterobacteriaceae, is sometimes associated with vegetable-related foodborne disease outbreaks. In susceptible hosts, Shigella causes dysentery with typical symptoms of diarrhea, abdominal pain, vomiting, and fever. In the majority of cases, infected food workers are considered the main source of Shigella [41]. According to the WHO, Shigella spp. belong to the list of medium priority pathogens for which new antibiotics are urgently needed. Shigella spp. are fluoroquinolone-resistant [24]. In addition, raw fish and oysters are among the most commonly implicated foods in the transmission and cases of Shigella infection [42]. Aeromonas spp., pathogenic for fish and humans, include A. hydrophila, A. caviae, A. jandaei, A. sorbia, A. salmonidae, and A. veroni; among them the most common pathogen is A. hydrophila [10]. According to Jin et al. [43] Aeromonas hydrophila virulence factors include enzymes, enterotoxin, adhesion, hemolysin, flagella, lipopolysaccharide, secretory systems, and quorum sensing. In humans, Aeromonas can cause gastrointestinal tract disorders and wound and soft tissue infections, as well as septicemia [44]. The multidrug-resistance of Aeromonas species is evidence of an emerging health problem in both humans and aquatic animals [45][46][45,46]. Aeromonas infections (including A. hydrophila infections) were the most widespread bacterial diseases occurring throughout the year in carps such as Catla catla, Labeo rohita, Cirrhinus mrigala, and Hypophthalmichthys molitrix [29]. The genus Acinetobacter includes a complex and heterogeneous group of bacteria, many of which are causing a range of opportunistic, often catheter-related, infections in humans [47]. The important member of this genus, Acinetobacter baumanii, is an emerging opportunistic pathogen in human medicine and a major cause of nosocomial infections worldwide. It is well-known for its ability to form biofilms, its strong environmental adaptability, and, especially, its multidrug resistance. According to the WHO, A. baumannii belongs to the most critical group of pathogens for which new antibiotics are urgently needed. A. baumannii is carbapenem-resistant. The most frequent clinical manifestations of A. baumannii infection in patients are pneumonia and bacteremia [25][48][25,48]. In addition, A. baumanii is reported to be an etiological agent of disease outbreaks in mandarin fish (Siniperca chuatsi), channel catfish (Ictalurus punctatus), Indian major carps (Labeo rohita and Catla catla) and Prussian carp (Carassais auratus gibelio). Other Acinetobacter species, such as A. johnsonii, A. lwoffii, A. pittii, A. radioresistens, and A. junii, were found to cause fish disease in recent years, suggesting that Acinetobacter spp. are emerging fish pathogens, posing a new threat to aquaculture [29][49][29,49]. The genus Pseudomonas includes more than 140 species, most of which are saprophytic. More than 25 species are associated with humans and in most cases cause opportunistic infections. These include P. aeruginosa, P. fluorescens, P. putida, P. cepacia, P. stutzeri, P. maltophilia, and P. putrefaciens. P. aeruginosa and P. maltophilia account for approximately 80 percent of pseudomonads recovered from clinical specimens. Because of the frequency with which it is involved in human disease, P aeruginosa has received the most attention. It is a ubiquitous free-living bacterium and is found in most moist environments. It infects a remarkably broad array of species, including plants, insects, and vertebrates. Although it rarely causes disease in healthy humans, it is a major threat to hospitalized patients, especially those with serious underlying conditions such as cancer, tuberculosis, AIDS, and severe burns. P. aeruginosa causes bacteremia and infection of the urinary tract, respiratory system, dermis, soft tissues, bones and joints, gastrointestinal tract, and blood [50][51][52][50,51,52]. According to the WHO, P. aeruginosa belongs to the most critical group of pathogens for which new antibiotics are urgently needed. P. aeruginosa is carbapenem-resistant [25]. Pseudomonas fluorescens, found in aquaponics by Chitmanat et al. [37], could be a rare cause of invasive hospital-acquired infections, with the usual site of infection being the bloodstream [53]. This bacterium, however, is commonly known for its strong food spoilage ability in ordinary and refrigerated food items (including milk and milk products, meat products, and vegetables) via its enzymes and pigment production [54]. Pseudomonads are one of the most dangerous fish pathogens that cause ulcerative syndrome and hemorrhagic septicemia. P. aeruginosa is part of the normal fish microbiota, but under stressful conditions this bacterium becomes highly opportunistic and pathogenic, causing serious disease [55]. On the other hand, P. fluorescens is found to cause chronic mortality in farmed Nile tilapia (Oreochromis niloticus) reared at low water temperatures [56]. Moreover, P. aeruginosa, P. fluorescens, P. putida, and P. stutzeri were among the common etiological agents of Labeo rohita and Catla catla infections [29]. In addition, P. aeruginosa is a typical plant pathogen capable of infecting the leaves and roots of the plant thale cress (Arabidopsis thaliana) [57]. The genus Staphylococcus, also found in aquaponics by Chitmanat et al. [37], consists of a number of species, of which S. aureus, S. epidermidis, and S. saprophyticus are the most frequently associated with human infection [58]. S. aureus is both a commensal bacterium and a human pathogen causing bacteremia and infective endocarditis as well as osteoarticular, skin and soft tissue, pleuropulmonary, and device-related infections [59]. According to the WHO, S. aureus belongs to the list of high priority pathogens for which new antibiotics are urgently needed. S. aureus is methicillin-resistant and vancomycin-intermediate-resistant [25]. Food handlers who have S. aureus on their skin and mucous membranes can act as a source of fish contamination during fish handling and processing [60]. On the other hand, S. aureus enterotoxins can cause gastroenteritis in humans via consumption of fish and fish products [13]. In addition, S. aureus is found to be pathogenic to Arabidopsis thaliana [57]. Recently, the opportunistic pathogen S. epidermidis has been the main cause of catheter-related bloodstream infections and early-onset neonatal sepsis as well as a frequent reason for prosthetic joint infections, prosthetic valve endocarditis, and other device-related infections [61]. This bacterium is reported to infect tilapia (Oreochromis niloticus), causing splenomegaly [56]. The widespread S. saprophyticus is both a commensal bacterium as well as a common human uropathogen associated with 10–20% of all urinary tract infections in sexually active women worldwide [62]. It was isolated from the liver and kidneys of freshwater-farmed hybrid sturgeon (Acipenser baerii × Acipenser schrenckii), and causes a disease with high mortality and surface bleeding [63]. Micrococcus spp. strains are commonly found in a wide variety of terrestrial and aquatic ecosystems, including soil, fresh and marine water, sand, and vegetation, as well as on the skin of warm-blooded animals, including humans. Also, Micrococcus spp. Strains have been reported to cause a variety of infections, usually as opportunistic pathogens. Thus, M. luteus strains are associated with septic arthritis, prosthetic valve endocarditis, and recurrent bacteremia. In addition, Micrococcus spp. Strains caused pneumonia in a patient with acute leukemia, localized skin infections in immunocompromised patients with HIV-1 disease, and catheter-related infection in patients with pulmonary arterial hypertension [64]. M. luteus, an important member of this genus, is found to cause disease in rainbow trout (Oncorhynchus mykiss), gilthead sea bream (Sparus aurata), sharpsnout sea bream (Diplodus puntazzo), and common dentex (Dentex dentex) [65]. This bacterium causes leafspot on mango as well [66]. Clostridium spp. were identified in an aquaponic system with multiple spoilage species. However, the species C. botulinum and C. perfringens, which cause foodborne disease outbreaks, were not detected by the authors [6]. Nevertheless, Khalil et al. [67] also found the presence of Clostridium in an aquaculture system, suggesting a potential risk of infection with pathogens of this genus in aquaponics. C. perfringens is widespread in nature; its primary habitat is the intestinal tract of humans and animals as well as the soil where feces are found [68]. Sabry et al. [69] found that in aquaculture there was a higher isolation level of C. perfringens from the external surface of fresh fish (31.8%) compared to the intestinal content of the same fish (9.1%). The virulence of C. perfringens results from the toxins produced by some of its strains. It causes several human diseases ranging from necrotizing enteritis to wound infection and life-threatening gas gangrene [69]. The other major pathogen of genus Clostridium, C. botulinum, is widely distributed in nature and occurs naturally in soil and aquatic environments. It is the cause for botulism due to the production of botulinum neurotoxin. Botulism is a severe human and animal disease characterized by flaccid paralysis leading to respiratory distress and death in the most severe cases. The presence of C. botulinum in fish can be associated with direct contact with contaminated aquatic environments and ingestion of C. botulinum spores from sediments or contaminated food. C. botulinum in fish can pose a significant threat to public health, especially when mishandling during fish processing occurs or insufficient heat treatment fails to destroy all C. botulinum spores in the final product [70][71][70,71]. Also, Clostridium spp. were associated with some soft rot diseases of herbaceous crops and sweet potato, as well as carrot and potato diseases [72]. Worthy of attention for the present work is the study of Khalil et al. [67] who examined the microbial population of two commercial recirculating aquaculture systems because they found multiple genera of bacteria and fungi not found so far in the studies of microbial communities of aquaponic systems. Since aquaculture systems are a part of aquaponic systems, the results obtained by these authors have been added to this research. They found the presence of genera Acinetobacter, Bacteroides, Chryseobacterium, Legionella, Pseudomonas, Microbacterium, Clostridium, and Rhodococcus, some of which were already mentioned above because they were discovered in aquaponics as well (Table 1). Bacteroides spp. are important clinical pathogens which are found in most anaerobic infections in humans. They are the most predominant anaerobes in the human colon and of these B. fragilis is the most virulent [73]. Some Bacteroides species can play both beneficial and pathogenic roles based on their location in the human organism, often being beneficial in the gut but opportunistic pathogens elsewhere in the body where they cause bacteremia and abscess formation [73][74][73,74]. According to Kabiri et al. [75], the microbiome of fish fecal samples obtained from tilapia (Oreochromis niloticus), grass carp (Ctenopharyngodon idella), channel catfish (Ictalurus punctatus), and blue catfish (Ictalurus furcatus) included B. eggerthii, B. uniformis, B. ovatus, and B. stercoris. It should be noted that B. ovatus belongs to B. fragilis group and has pathogenic potential [76]. The species of Chryseobacterium are commonly found in environmental, food, and water sources and some have been isolated from the clinical environment, humans, and animals, while others are pathogenic for fish and humans. Some species such as C. indologenes, C. soldanellicola, C. oranimense, and C. koreense could be potential human pathogens, while C. piscium might be pathogenic to fish. C. indologenes is the most frequently isolated Chryseobacterium species from clinical specimens. It is a rare etiological agent of human disease, usually causing nosocomial infections that include bacteremia, pneumonia, meningitis, pyomyositis, keratitis, as well as indwelling device-related infections such as urinary tract, surgical, and burn wound infections. In foods, Chryseobacterium spp. are generally considered spoilage bacteria, as most are psychrotolerant and produce proteolytic enzymes, while some produce biogenic amines [77][78][77,78]. Also, C. indologenes is one of the primary causative agents of Panax notoginseng root rot [79]. Legionella spp. have been identified as one of the major causes of severe community-acquired pneumonia or nosocomial pneumonia. The most frequently isolated pathogenic species of this genus is the opportunistic pathogen L. pneumophila. The bathing facilities of public baths are the major source of infection [80][81][80,81]. Legionella infection occurs almost exclusively by aspiration of contaminated water while person-to-person transmission is very rare [82]. Microbacterium spp. are typically found in various environmental sources, such as soil and water samples. The most frequently isolated species from clinical samples are M. oxydans and M. paraoxydans. They rarely cause human infection, mostly infecting immunocompromised patients and catheter insertion sites, making them difficult to identify in clinical settings. Microbacterium spp. could be the cause for bacteremia, peritonitis, and endophthalmitis [83][84][83,84]. A Rhodococcus species with clinical importance is R. equi. Although it is mainly an opportunistic pathogen, a number of cases described infection occurring among individuals with normal immune systems. The main clinical symptom is pneumonia but this bacterium can disseminate to cause disease in virtually any human tissue [85]. Moreover, Speare et al. [86] reported a Rhodococcus sp. with pathogenic potential to juvenile Atlantic salmon (Salmo salar). In addition, R. fascians is a plant-pathogenic bacterium that causes malformations on aerial plant parts, whereby leafy galls occur at axillary meristems [87]. This species typically causes disease on herbaceous perennials [88]. In conclusion, the various human pathogenic bacteria found in aquaponics are usually of fish origin or end up in the water when proper hygiene practices are not applied and followed. It should be noted that only a few cases of Salmonella spp. and one incident of E. coli O157:H7 in aquaponics have been found in the literature so far. Moreover, no cases of L. monocytogenes have been reported in aquaponics until now. Most of the other pathogens found so far in aquaponics are opportunistic, and dangerous mainly to immunocompromised patients. However, many aquaponic pathogens are listed in the WHO list of drug-resistant bacteria for which new antibiotics are urgently needed. This could pose a challenge to infection treatment. Many of the human bacterial pathogens are pathogenic to fish but rarely to plants (Figure 1), which should be considered when preventive actions against disease are taken. In view of the aforementioned facts, if strict hygiene practices are followed, aquaponic systems are a good choice for growing healthy fish and plants safe for human consumption.Table 1.
Pathogenic bacteria in aquaponics that are potentially hazardous for human health.
| Bacteria | Fish Species | Plant Type | Reference | ||||
|---|---|---|---|---|---|---|---|
| Gram-Negative | |||||||
| Aeromonas hydrophila | Hybrid catfish (Clarias macrocephalus × C. gariepinus); Nile tilapia (Oreochromis niloticus); Mozambique tilapia (Oreochromis mossambicus) | Lettuce (Lactuca sativa) | [37][89][90][37,89,90] | ||||
| Acinetobacter spp. | Nile tilapia (Oreochromis niloticus) | [67] | |||||
| [ | 66 | Acinetobacter baumanii | hybrid catfish (Clarias macrocephalus × C. gariepinus) | Lettuce (Lactuca sativa) | [37] | ||
| ] | |||||||
| Aspergilllus flavus | Carp (Cyprinus carpio) | [177] | Bacteroides spp. | ||||
| Aspergilllus niger | Nile tilapia (Oreochromis niloticus) | Carp (Cyprinus carpio)[67] | |||||
| [ | 177 | ] | Chryseobacterium spp. | Clarias (Clarias gariepinus); Nile tilapia (Oreochromis niloticus) | [67 | ||
| Cladosporium spp. | Clarias (Clarias gariepinus) | ] | |||||
| [ | 66 | ] | Coliforms | Rainbow trout (Oncorhynchus mykiss); lambari fish (Astyanax bimaculatus); tilapia (Oreochromis niloticus x O. aureus); Nile tilapia ( | |||
| Fusarium spp. | Oreochromis niloticus); catfish (Silurus glanis); koi (Cyprinus rubrofuscus) | Clarias (Clarias gariepinus); Carp (Duckweed (Lemna minuta); lettuce (Lactuca sativa) | Cyprinus carpio) | Lettuce (Lactuca sativa)[3][4 | [66]][175][19][177][22][38][91][92][3,4,19,22,[66,175,17738,91,92] | ||
| ] | E. coli | Rainbow trout(Oncorhynchus mykiss); hybrid catfish (Clarias macrocephalus × C. gariepinus); Nile tilapia (Oreochromis niloticus); | Duckweed ( | ||||
| Phaeoacremonium spp. | Lemna minuta | ); lettuce (Lactuca sativa) | Nile tilapia (Oreochromis niloticus)[4][6][19][21][22][37][89][92][4,6,19,21,22,37,89,92] | ||||
| [ | 66 | ] | Legionella spp. | Nile tilapia (Oreochromis niloticus) | |||
| Macrophomina spp. | Nile tilapia (Oreochromis niloticus) | [67] | |||||
| [ | 66 | ] | Pseudomonas spp. | Nile tilapia (Oreochromis niloticus) | [67] | ||
| Microascus spp. | Nile tilapia (Oreochromis niloticus) | [89][67,89] | |||||
| [ | 66 | ] | Pseudomonas fluorescens | Hybrid catfish (Clarias macrocephalus × C. gariepinus) | |||
| Mucor spp. | Lettuce ( | Clarias (Clarias gariepinusLactuca sativa) | )[37] | ||||
| [ | 66 | ] | Plesiomonas shigelloides | Hybrid catfish (Clarias macrocephalus × C. gariepinus) | Lettuce (Lactuca sativa) | ||
| Penicillium spp. | Nile tilapia (Oreochromis niloticus); Carp (Cyprinus carpio) | [ | 37] | ||||
| Salmonella spp. | Rainbow trout (Oncorhynchus mykiss); hybrid catfish (Clarias macrocephalus × C. gariepinus) | Duckweed (Lemna minuta); lettuce (Lactuca sativa) | [19][37][19,37] | ||||
| Shigella sonnei | Mozambique tilapia (Oreochromis mossambicus) | [90] | |||||
| Gram-positive | |||||||
| Clostridium spp. | Nile tilapia (Oreochromis niloticus); Clarias (Clarias gariepinus) | [6][6[67],67] | |||||
| Microbacterium spp. | Clarias (Clarias gariepinus) | [67] | |||||
| Micrococcus spp. | Hybrid catfish (Clarias macrocephalus × C. gariepinus) | Lettuce (Lactuca sativa) | [37] | ||||
| Rhodococcus spp. | Nile tilapia (Oreochromis niloticus) | [67] | |||||
| Staphylococcus spp. | Hybrid catfish (Clarias macrocephalus × C. gariepinus) | Lettuce (Lactuca sativa) | [37] |
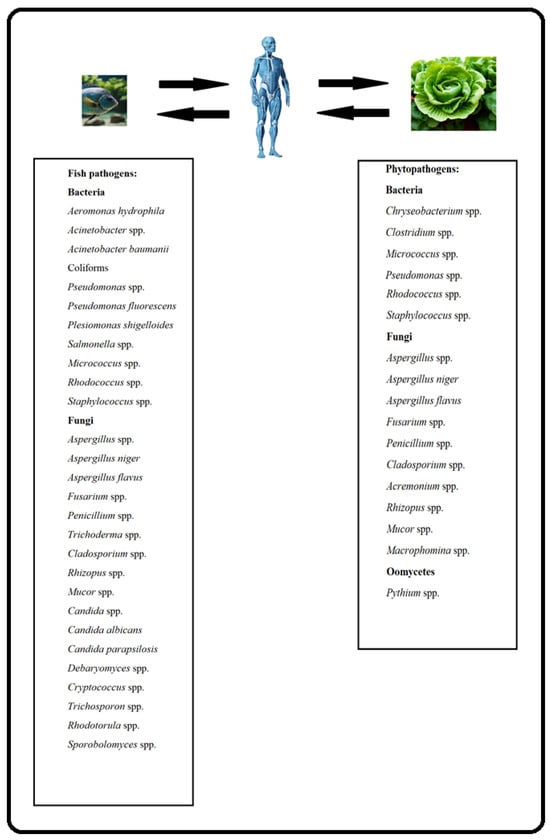
Figure 1.
Fish and plant pathogens in aquaponics that are potentially hazardous for human health.
2.2. Fungi and Fungus-Like Microorganisms (Oomycetes)
Filamentous fungi occur commonly in the environment due to their ability to grow on almost any substrate and under harsh conditions, and to produce spores that are dispersed in the air at low temperatures. They are heterotrophic and saprophytic organisms, extracting nourishment and energy from dead organic matter and possessing the ability to synthesize various natural products such as primary and secondary metabolites. These fungi can be dispersed in the environment in various ways, mostly by air, soil, water, and seeds, while the transmission route through insects acting as vectors is less frequent. Aspergillus, Fusarium, Penicillium, Cladosporium, Acremonium, Alternaria, and Curvularia are some of the most common fungal genera that belong to the filamentous fungi family, with the Aspergillus species reportedly most abundant and widespread worldwide [93][94][93,94]. Members of Fusarium, Aspergillus, and Penicillium genera, in particular, are known to produce secondary metabolites termed mycotoxins in specific conditions of temperature and humidity. The main mycotoxins produced by Aspergillus spp. are aflatoxins, and by Fusarium spp. are fumonisins, trichothecenes, and zearalenone. The main mycotoxin produced by Penicillium spp. is ochratoxin A. Consumption of mycotoxin-contaminated food or feed can lead to acute or chronic toxicity in humans and animals. Mycotoxins show genotoxic, carcinogenic, and mutagenic effects, and some of them have immunosuppressive activity [95][96][95,96]. Through aquaponic water, these mycotoxins produced by diseased plants could disseminate and accumulate in fish. Moreover, it has been confirmed that fungi can produce mycotoxins in water as well [97]. Finally, mycotoxins can enter the human organism through consumption of fish or/and plants produced by aquaponics. Aspergillus spp. are filamentous fungi commonly found in soil, decaying vegetation, and seeds and grains (Table 2). Only a few well-known species of genus Aspergillus are considered important opportunistic pathogens in humans. A. fumigatus is the most common and life-threatening airborne opportunistic fungal pathogen which is particularly important for immunocompromised hosts. Inhalation of A. fumigatus spores (conidia) into the lungs can cause multiple diseases in humans that depend on the immunological status of the host. These diseases include invasive pulmonary aspergillosis, aspergilloma and various forms of hypersensitivity diseases such as allergic asthma, hypersensitivity, pneumonitis and allergic bronchopulmonary aspergillosis [98]. After A. fumigatus, A. flavus is the second leading etiological agent of invasive aspergillosis and it is the most common cause of superficial infection. The most common clinical syndromes associated with A. flavus include chronic granulomatous sinusitis, keratitis, cutaneous aspergillosis, wound infections, and osteomyelitis following trauma and inoculation. In addition, A. flavus produces aflatoxins, the most toxic and potent hepatocarcinogenic natural compounds ever characterized [99]. A. niger is a mold rarely reported as a cause of pneumonia [100]. Opportunistic plant infections by Aspergillus species are also common following drought, insect damage, or other environmental stresses. In particular, infection by A. flavus and A. parasiticus strains causes large economic losses in agriculture due to related contamination with mycotoxins. A. flavus is the main cause of Aspergillus infections and aflatoxin contamination of crops. In contrast, while A. fumigatus is the most common cause of human and veterinary aspergillosis, it is not known to cause disease in any host plant [101]. A. niger is a common phytopathogen that infects many fruits and vegetables, such as onion, corn, and others, causing destruction, rotting, and decomposition of plant tissues [102]. Moreover, A. niger, A. flavus, A. ochraceus, A. terreus, and A. versicolor were found to cause mycotic infections in freshwater Nile tilapia (Oreochromis niloticus) [103]. Therefore, it can be concluded that if Aspergillus spp. members break into an aquaponic system, serious disease to humans, plants, and/or fish is likely to occur. Fusarium spp. show a global distribution and are associated with a wide range of emerging infections in plants, animals, and humans collectively termed fusariosis. In the medical field, various species of Fusarium are associated with local or invasive infections in both immunocompromised and immunocompetent individuals. The most prevalent infections are onychomycosis, skin infections, and keratitis. Among human pathogenic Fusarium, F. solani is the most common and virulent (comprising approximately 40–60% of infections), followed by F. oxysporum (~20%) and F. fujikuroi and F. moniliforme (~10%) [104][105][104,105]. Phytopathogenic Fusarium spp. are F. oxysporum, F. solani, F. fujikuroi, and F. graminearum. They infect a wide range of plants, including popular aquaponics plants such as tomato, cucumber, onion, spinach, pea, eggplant, and strawberry [106][107][106,107]. F. moniliforme and F. udum were found to be natural pathogens of freshwater fish reared in reservoirs, causing mycosis and high mortality [108]. In addition, the F. solani species complex causes superficial and systemic mycosis of Nile tilapia (Oreochromis niloticus) and zebrafish (Danio rerio) [109][110][109,110]. The abovementioned facts show that Fusarium spp. and especially F. solani are highly hazardous for aquaponics, due to their high pathogenic potential for plants, fish, and humans. Penicillium spp. are multifarious and widespread in the environment but, despite their abundance and diversity, they are not often associated with human and animal infections. The species usually related to such infections are P. citrinum, P. chrysogenum, P. digitatum, P. expansum, and P. marneffei and the mode of infection is mostly via inhalation and sometimes ingestion. Diseases that result from Penicillium infection of any Penicillium species are commonly referred to as penicillosis. Species of this genus have been mentioned in relation to human infections such as keratitis, endophthalmitis, otomycosis, pneumonia, endocarditis, and urinary tract infections [93][111][93,111]. Additionally, P. expansum is a dominant post-harvest pathogen among fruits and vegetables [112] while P. cyclopium, P. viridicatum, P. hirsutum, and P. allii have been reported as garlic pathogens [113]. Some Penicillium spp. are highly hazardous for blue tilapia (Oreochromis aureus), Nile tilapia (Oreochromis niloticus), and Indian carp (Catla catla) [103][114][115][103,114,115]. In addition, Shahbazian et al. [116] isolated P. expansum and P. citrinum from infected eggs of rainbow trout (Oncorhynchus mykiss). These facts emphasize that the presence of Penicillium spp. in aquaponic systems results in a certain danger to human, plant, and fish health. Unlike Aspergillus, Fusarium, and Penicillium, which cause severe infections in a wide variety of patients, Trichoderma has generally been considered nonpathogenic in humans, but localized and disseminated infections in immunocompromised and immunocompetent patients have been reported worldwide. T. longibrachiatum is the most frequently reported species associated with invasive fungal infections, followed by T. atroviride, T. bissettii, T. citrinoviride, T. harzianum, T. koningii, T. pseudokoningii, and T. viride [117]. Trichoderma spp. cause a variety of clinical manifestations, such as invasive pulmonary infection, peritonitis, CNS infection, endocarditis, fungemia, and disseminated disease affecting distant organs, particularly in patients with hematological malignancies and those undergoing long-term ambulatory peritoneal dialysis (CAPD) [117][118][117,118]. Trichoderma spp. are considered beneficial for aquaponically grown plants, because they are plant symbionts widely used as biofertilizers and biocontrol agents for plant diseases [119]. In addition, it has been reported that Trichoderma spp. extracts have antimicrobial activity against human and fish pathogens due to the secondary metabolites produced by these fungi [120]. Nevertheless, T. asperellum is considered a rare and low-pathogenic fungus in fish [121]. Cladosporium spp. are existing in both outdoor and indoor environments and they rarely cause illness in humans. Nevertheless, subcutaneous abscesses, central nervous system, and pulmonary infections in immunocompromised patients have been documented in the literature. One of the most frequently reported species with pathogenic potential is C. bantiana, followed by C. sphaerospermum [122][123][122,123]. Cladosporium spp. are associated with numerous agricultural crop diseases, causing leaf spots, scab, postharvest rots, and other symptoms leading to economic losses [124]. Also, they cause mycotic infections in freshwater Nile tilapia (Oreochromis niloticus) [103]. Acremonium spp. are commonly found in soil, rotting vegetation, and decaying food [125]. Species reported to cause human infections include A. alabamensis, A. falciforme, A. kiliense, A. roseogriseum, A. strictum, A. potroni, and A. recifei. This genus has been recognized as an etiological agent of human skin infections. Eumycotic mycetoma is caused by a variety of fungi, but not often by Acremonium. In addition, the most common pathogens of onychomycosis (fungal nail infection) are dermatophytes and Fusarium spp. followed by Acremonium spp. In the literature cases of keratitis, osteomyelitis, peritonitis and dialysis fistulae infection, localized infections, pneumonia, and disseminated infections, including meningitis, endocarditis, and cerebritis, have been published. Reports of systemic infections are almost always in patients with underlying risk factors such as malignancy and transplantation [125][126][125,126]. A. strictum is potentially pathogenic to the flower stems of weakened carrot plants under stress conditions [127]. The hyphomycetous genus Phaeoacremonium shows morphological characteristics between Acremonium and Phialophora. The main environmental source of these fungi are woody plants. The current list of human pathogens includes P. alvesii, P. amstelodamense, P. griseorubrum, P. krajdenii, P. parasiticum, P. rubrigenum, P. sphinctrophorum, P. tardicrescens, and P. venezuelense, of which P. parasiticum is the most frequently isolated from human hosts. Most reported cases of Phaeoacremonium infection included subcutaneous abscesses, cysts, or chronic or acute osteoarthritis in immunocompetent or immunocompromised patients; these cases were often initiated by traumatic inoculation. Disseminated infections, fungemia, or endocarditis have been found in a few cases involving immunocompromised patients [128][129][128,129]. The ubiquitous Rhizopus is the most common fungal genus causing mucormycosis; other less common etiological agents of infection include Mucor spp. and Rhizomucor spp. The infection usually affects immunocompromised patients and commonly presents two clinical syndromes: sinopulmonary and rhinocerebral. Some rare forms include cutaneous, intestinal, and pulmonary diseases [130]. The human pathogenic species of this genus include R. microsporus and R. azygosporus [131][132][131,132]. Additionally, it was reported that R. arrhizus caused rot on sunflower and tomato plants in China and Pakistan, respectively [133][134][133,134]. In addition, Rhizopus spp. are responsible for post-harvest fruit rot in strawberries in the UK [135]. Rhizopus spp. are one of the etiological agents of mycotic infections with economic importance in freshwater Nile tilapia (Oreochromis niloticus) [103]. The Mucor genus consists of early diverging fungi which are basal in comparison to higher fungi (i.e., Ascomycota and Basidiomycota phyla). Mucor species are very abundant in nature and often ubiquists. They could cause either superficial (cutaneous, subcutaneous) or invasive mycoses called mucormycoses, especially in immunocompromised patients. According to literature data, only three Mucor species are frequently cited in human infection cases: M. circinelloides, M. indicus, and M. pusillus [136]. Mucor is one of the genera responsible for postharvest rot of strawberry fruit [135][137][135,137]. Also, Reyes [138] reported a severe rot of tomato, cucumber, eggplant, and pepper infected by M. mucedo. Mucor spp. have been found to be highly pathogenic to cultured fish such as silver carp (Hypophthalmichthys molitrix) and goldfish (Carassius auratus) [139]. In addition, the aforementioned human pathogen M. circinelloides was found to be pathogenic to yellow catfish (Pelteobagrus fulvidraco) and zebrafish (Danio rerio) as well [140][141][140,141]. The Microascus genus comprises species commonly isolated from soil, decaying plant material and indoor environments. A few species are also recognized as phytopathogens and opportunistic pathogens in insects and animals, including humans [142][143][142,143]. M. cirrosus causes cutaneous infection [144], pulmonary infection [145], and fatal invasive infection with fungemia [146]. There are cases of human subcutaneous infection caused by M. ennothomasiorum [147], mycetoma caused by M. gracilis [148], and suppurative cutaneous granulomata caused by M. cinereus [149]. In general, Microascus spp. rarely cause infections and they usually occur in immunocompromised patients [146]. Wallemia spp. are known for their ability to grow in osmotically challenging environments, such as dry or salted foods, dry feed, indoor and outdoor air, etc. Up until now, only strains of W. sebi, W. mellicola, and W. muriae were related to human health problems as either allergological conditions or rare subcutaneous/cutaneous infections [150]. Genus Macrophomina was assigned to the Botryosphaeriaceae family and includes several phytopathogens: M. phaseolina, M. pseudophaseolina, M. euphorbiicola, and M. vaccinia [151]. The most important pathogenic species of this genus is M. phaseolina. This fungus rarely causes disease in humans. So far, there have been cases of keratitis and infections in a renal transplant recipient and a child with acute myeloid leukemia. Most of the cases were in immunocompromised patients [152]. M. phaseolina infects at least 500 plant species, causing diseases such as stem and root rot, charcoal rot, and seedling blight [153]. Yeasts exist in several environmental niches, including marine, aquatic, atmospheric, and terrestrial habitats. Yeasts in fish mucus and intestines are considered opportunistic pathogens that attack the fish organism when it is stressed or immunocompromised. Several genera of yeasts, isolated from fish and found in aquaponics, are considered human pathogens as well (e.g., Candida, Cryptococcus, Debaryomyces, Rhodotorula, and Trichosporon spp.) [154]. The black yeast-like fungi Aureobasidium are ubiquitous microorganisms found in a wide variety of environments as saprophytes, endophytes, and pathogens. They are known to be capable of producing numerous different metabolites, many of which find applications in the field of plant pathogen control [155]. The main pathogenic species of this genus are A. pullulans and A. melanigenum, which could be a source of infection in immunocompromised hosts. The reported clinical manifestations include keratomycosis, cutaneous mycoses, peritonitis, meningitis, and fungemia [156][157][156,157]. Yeasts of the genus Candida can be isolated from samples of groundwater, mineral water, domestic and industrial wastewater, rivers, and lakes, demonstrating the ubiquity of this genus and its ability to adapt to different environments. Candida species cause opportunistic infections in both healthy and immunocompromised individuals, including candidiasis, candiduria, and nail mycosis, as well as systemic infections that can debilitate patients or even lead to death [158]. Approximately 75% of all Candida infections in humans are caused by C. albicans, while C. glabrata, C. parapsilosis, and C. tropicalis are important emerging pathogens related to nosocomial infections. It is reported that C. albicans causes > 150 million mucosal infections and ~200,000 deaths per annum due to invasive and disseminated disease in susceptible individuals [158][159][158,159]. Furthermore, C. albicans is a cause of mycotic infections with economic importance in freshwater Nile tilapia (Oreochromis niloticus), common carp (Cyprinus carpio), catfish (Clarias gariepinus), and grey mullet (Mugil cephalus) [103][160][103,160]. In addition to C. albicans, other Candida species pathogenic to Nile tilapia (Oreochromis niloticus) include C. parapsilosis and C. guilliermondii [161]. Closely related to Candida spp. are Debaryomyces spp. with the most prominent member being D. hansenii. This yeast is commonly found in natural substrates and in many types of cheese. It has been repeatedly associated with catheter-related bloodstream infections and, rarely, with other infections [162]. D. hansenii demonstrated pathogenicity to goldfish (Carassius auratus), Atlantic salmon (Salmo salar), African catfish (Clarias gariepinus), and rainbow trout (Oncorhynchus mykiss) as well [154][163][154,163]. Cryptococcus spp. reside in diverse ecological niches. Both C. neoformans and C. gattii, the most important members of this genera, are abundant in decaying materials within hollows of different tree species. C. neoformans is particularly abundant in avian excreta. It is the main species of this genus and the predominant etiological agent of cryptococcosis, a globally distributed invasive fungal infection which presents substantial therapeutic challenges. The disease affects both immunocompromised and immunocompetent individuals and can cause pneumonia and meningoencephalitis [164]. Cryptococcus spp. has been found to be pathogenic to tilapia (Oreochromis niloticus) and African catfish (Clarias gariepinus) [154]. Thichosporon species are yeasts that are common in the environment and may be a part of the normal microbiota of the human skin and gastrointestinal tract. Additionally, they are often found to cause superficial infections of the skin, nails, and hair and invasive infection in immunocompromised patients. Also, a rare case of a Trichosporon brain abscess has been documented [165][166][165,166]. Among the most frequent etiological agents of Trichosporon infections are T. inkin, T. asahii, T. cutaneum, T. mucoides, T. ovoides, and T. asteroides [167]. In addition, Trichosporon spp. have been found to be pathogenic to tilapia (Oreochromis niloticus), gray mullet (Mugil cephalus), and African catfish (Clarias gariepinus) [154][161][154,161]. Rhodotorula are ubiquitous saprophytic yeasts that can be found in many environmental sources, as well as opportunistic pathogens that colonize and infect susceptible patients. Most of the cases of Rhodotorula infection in humans demonstrated symptoms of fungemia associated with central venous catheter use [168]. In addition, Rhodotorula spp. have been found to be pathogenic to tilapia (Oreochromis niloticus), African catfish (Clarias gariepinus), and gray mullet (Mugil cephalus) as well [154][161][154,161]. Closely related to Rhodotorula, Sporobolomyces are yeasts commonly isolated from environmental sources including lake water, tree leaves, and air with their natural habitat in humans, mammals, birds, and plants. S. salmonicolor is the most frequently isolated member of Sporobolomyces spp. from clinical samples, although S. salmonicolor infections are quite rare. This pathogenic yeast has previously been reported to cause invasive infections including dermatitis, cerebral infection, fungemia, encephalitis, ocular infection, and lymphadenitis [169]. As an opportunistic pathogen, S. salmonicolor can occasionally cause disease in fish as well [170]. Genus Malassezia comprises yeast species that are part of the normal human skin microbiota from where they can easily inhabit the environment, including aquaponic water. They are involved in skin disorders, such as pityriasis versicolor, seborrheic dermatitis, atopic eczema, and folliculitis [171]. Sterigmatomyces spp. are marine-derived yeasts belonging to the phylum Basidiomycota. Imashioya et al. [172] reported a rare case of liver abscess due to S. halophilus in a boy with acute lymphoblastic leukemia. Pythium is a genus of fungus-like parasitic oomycetes. Although rare, human pythiosis caused by Pythium insidiosum has occurred in the USA, Thailand, Australia, New Zealand, Haiti, and Malaysia. The disease might be manifested as a vascular, ophthalmic, subcutaneous, or systemic type [173]. In addition, P. insidiosum is pathogenic to fish as well [174]. Moreover, Pythium spp. cause many plant diseases, including damping-off, root rot, collar rot, and stem rot in different production systems, including aquaponics and hydroponics [175][176][175,176]. In conclusion, most of the pathogenic molds found in aquaponics are dangerous to humans, plants, and fish (e.g., Aspergillus, Fusarium, Mucor, Penicillium, Rhizopus, Cladosporium, etc.). On the other hand, aquaponic yeasts are mainly pathogenic to fish and humans (Figure 1). Usually, the fungi found in aquaponics are described by the researchers in terms of genus, and in rare cases in terms of species. However, only some species of the fungal genus are pathogenic to humans. Thus, in most cases, the risk of the presence of human fungal pathogens in aquaponic water is not particularly high. From the analysis of different fungal pathogens, it can be concluded that they usually cause opportunistic infections in immunocompromised patients. As such, if proper hygiene practices are followed, the fungi in aquaponics are not a major concern for human health. In this regard, however, monitoring of mycotoxin content in fish and plants is necessary, since they can enter the human body through food consumption.Table 2.
Pathogenic fungi and oomycetes in aquaponics that are potentially hazardous for human health.
| Fungi | Fish Species | Plant Type | Reference |
|---|---|---|---|
| Molds | |||
| Acremonium spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Aspergilllus spp. | Clarias (Clarias gariepinus) | ||
| [ | |||
| 66 | |||
| ] | |||
| [ | |||
| 177 | |||
| ] | [ | 66 | ,177] |
| Rhizopus spp. | Carp (Cyprinus carpio) | [177] | |
| Trichoderma spp. | Clarias (Clarias gariepinus); Carp (Cyprinus carpio) | [66][177][66,177] | |
| Wallemia spp. | Clarias (Clarias gariepinus) | [66] | |
| Yeasts | |||
| Aureobasidium spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Candida spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Candida albicans | Carp (Cyprinus carpio) | [177] | |
| Candida parapsilosis | Carp (Cyprinus carpio) | [177] | |
| Cryptococcus spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Debaryomyces spp. | Clarias (Clarias gariepinus) | [66] | |
| Malassezia spp. | Clarias (Clarias gariepinus) | [66] | |
| Rhodotorula spp. | Clarias (Clarias gariepinus) | [66] | |
| Sterigmatomyces spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Sporobolomyces spp. | Nile tilapia (Oreochromis niloticus) | [66] | |
| Trichosporon spp. | Clarias (Clarias gariepinus); Nile tilapia (Oreochromis niloticus) | [66] | |
| Oomycetes | |||
| Pythium spp. | Lettuce (Lactuca sativa) | [175] |
