The application of feedback devices for cardiopulmonary resuscitation (CPR) can effectively enhance the quality of life-saving treatment during CPR.
- cardiopulmonary resuscitation
- feedback
- cardiac arrest
- basic life support
1. Introduction
2. Classification of Feedback Devices for Cardiopulmonary Resuscitation
The feedback device for CPR has undergone significant development since its early use as a simple metronome. The metronome provides a fixed beat to assist the rescuer in maintaining a steady compression rate, thereby ensuring the quality of CPR and increasing the likelihood of successful resuscitation [5]. Feedback devices for CPR are generally divided into two categories based on the type of feedback information: auditory–visual feedback devices and physiological information data-monitoring feedback devices. Auditory–visual feedback devices provide a certain beat sound and display compression depth graphically or through color differences and can use sound, graphics, or color to correct the rescuer’s compression rate and depth in real time to ensure the quality of CPR. Physiological information data-monitoring feedback devices can monitor one or more parameters, such as cardiac output (CO), coronary perfusion pressure (CPP), mean arterial relaxation pressure (MARP), ECG amplitude spectrum area (AMSA), ETCO2, pulse oxygen saturation waveform, and regional cerebral oxygen saturation (rScO2), to adjust the compression strategy.2.1. Audio-Visual Feedback Devices
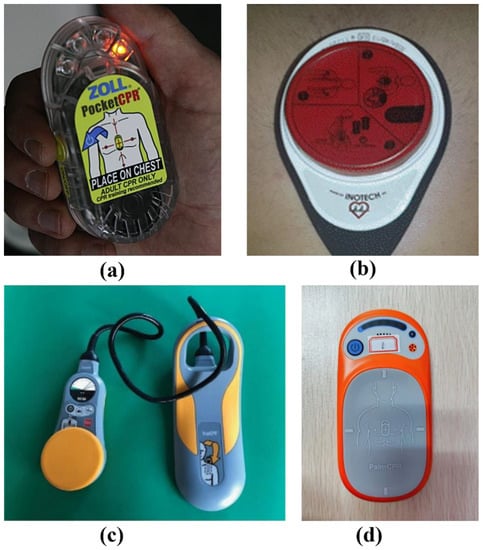
In 2015, the American Heart Association endorsed the use of feedback devices during CPR to enhance resuscitation quality [4]. Even for medical professionals, accurately assessing the depth and frequency of CPR may be challenging [6][7][9,10], and the quality of resuscitation may decline due to fatigue. Additionally, perceived compression depth and rate may differ from actual ones [8][11], which underscores the need for audio-visual feedback devices to improve CPR quality and enhance resuscitation quality. Currently, the development of audio-visual feedback devices for CPR has reached a relatively mature stage. These devices are predominantly based on two main components: pressure sensors and accelerometers. Pressure sensors measure the force applied to the patient’s chest, which is set based on the patient’s weight and the desired depth of compression. However, since it cannot detect individual compression, a pressure sensor-based feedback device can only provide feedback on compression depth and not on compression rate. On the other hand, accelerometers measure the acceleration of the patient’s chest and use these data to calculate the distance moved during compression. The latest CPR feedback devices on the market are predominantly based on accelerometers, with some models also integrating pressure sensors. While an accelerometer-based feedback device is equipped with an electronic processor capable of calculating the compression rate, it is not well-suited for monitoring the quality of ventilation [9][12]. As the earliest device with cardiopulmonary resuscitation feedback function, CPR-plus boasts several advantages, including non-invasiveness, portability, and easy use. The CPR-plus is shown in Figure 1a. It achieves compression depth measurement via a pressure-sensitive compression plate and features a metronome for prompt pacing.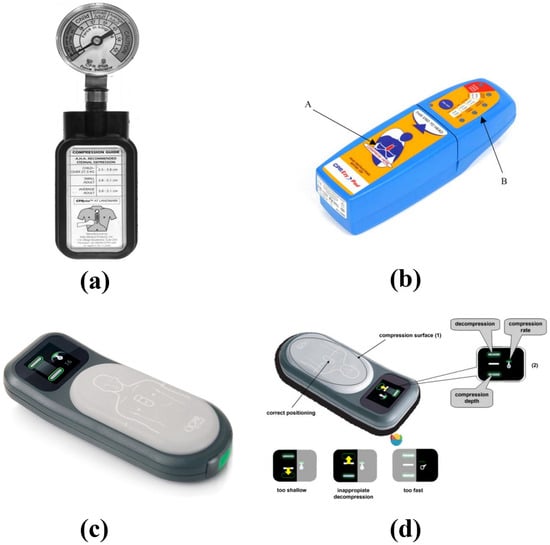
2.2. Research on Feedback Devices Based on Physiological Information Data Monitoring in China and Abroad
Simple feedback systems have been shown to improve the effectiveness of chest compression during CPR. However, a limitation of such systems is the lack of personalization for individual patients and a standardized execution. To address this issue, feedback devices utilizing physiological data monitoring are needed. Due to the limitations of the prehospital environment, invasive detection is often difficult. A study by Lampe et al. at Northwell Health established a time-dependent function correlating carotid blood flow during cardiac arrest resuscitation and response to varying chest compression. By predicting the carotid blood flow generated by subsequent chest compression, the study aimed to optimize CPR parameters in real time, maximizing carotid blood flow [15][29]. Sebastian et al. evaluated the feasibility of using a machine-controlled closed-loop CPR (MC-CPR) system to optimize coronary perfusion pressure (CPP) during CPR. Their real-time hemodynamic simulations demonstrated that MC-CPR, controlled by a closed-loop machine, significantly outperformed the AHA CPR guidelines in improving coronary perfusion pressure [16][30].2.3. Application Status and Effects of Cardiopulmonary Resuscitation Feedback Devices
CPR feedback devices are widely utilized in CPR training. In studies investigating CPR training, it has been observed that training with a feedback device enhances CPR competency and overall quality more significantly than traditional CPR training methods [17][35]. Furthermore, the utilization of feedback devices can augment skill acquisition and overall performance in cardiopulmonary resuscitation [18][36]. From a practical standpoint, the combination of current CPR audio-visual feedback devices and smartphones offers a more accessible feedback tool for emergency situations. By utilizing the data collected through a smartphone’s built-in accelerometer, real-time assessment of compression depth and frequency can be achieved, aligning closely with the actual values. This enables accurate real-time feedback on CPR quality through a dedicated CPR mobile application [19][38].2.4. Integration of Feedback Devices with Defibrillator and Related Equipment
Real CPR Help™ is an enhanced functionality integrated into Zoll’s AED Plus, utilizing accelerometer technology within the ZOLL defibrillator electrodes, furnishing real-time feedback concerning the accuracy of CPR compression in terms of depth and frequency. Audio and visual prompts guide the operator through the CPR process.3. Current Limitations of Cardiopulmonary Resuscitation Closed-Loop Feedback Devices
To improve the quality and success rate of CPR and provide effective guidance for rescuers, as well as personalize chest compression for cardiac arrest patients, feedback devices for CPR are continuously being developed. These feedback devices have achieved significant results in terms of improving the quality of CPR and increasing the survival rate of cardiac arrest patients. However, some limitations and problems still remain.-
Limited Application Scenario
-
A Non-Intuitive Feedback Mode
-
Limitations of Feedback Parameters
-
Limited Contribution to Improving Chest Compression Quality
4. Equipment Support of CPR Feedback Physiological Parameter Monitoring
4.1. End-Tidal Carbon Dioxide Monitoring Equipment
The infrared method is routinely utilized in clinical settings, primarily due to its main absorption wavelength for CO2 at 4260 nm. Based on this property, CO2 concentration can be deduced from its absorption rate. Two modes of application are prevalent for the infrared method: bypass flow and mainstream flow [20][45]. In mainstream flow mode, the sensor is directly connected to the patient’s tracheal tube connector, becoming an integral part of the artificial airway. The airflow actively traverses the sensor. The key advantages of the mainstream infrared method lie in its swift medical diagnostic response due to the sensor’s direct contact with the airflow. Infinium Medical has developed the Cleo EtCO2 Monitor with Vitals, an intuitive device for non-invasively measuring patients’ vital signs, including blood pressure, SpO2, rapid temperature, and exhaled carbon dioxide. The device supports continuous monitoring over extended periods and is applicable in a variety of settings. Its uses encompass both intubated and non-intubated applications, on-site inspections, bedside monitoring, and more [21][46]. Masimo’s Emma Capnograph, a portable real-time carbon dioxide analyzer, provides continuous and clear visualizations of carbon dioxide measurements. The device can display EtCO2 and respiratory rate measurements, along with real-time ETCO2 waveforms within a timeframe of 15 s [22][47].4.2. The Application of End-Tidal Carbon Dioxide in Cardiopulmonary Resuscitation Feedback
End-tidal carbon dioxide (ETCO2), serving as an indirect measure of blood flow during cardiopulmonary resuscitation (CPR), is widely employed as a guiding tool in the CPR process [23][48]. Throughout the course of CPR, ETCO2 maintains a direct correlation with cardiac output, thus making it a common metric for gauging output during CPR [24][49]. Existing research suggests a linear relationship between the depth of chest compression and end-expiratory carbon dioxide values. An analysis utilizing mixed-effects models on a sample of 230 subjects revealed a 4.0% increase in ETCO2 (p < 0.0001) for each 10 mm augmentation in chest compression depth and a 1.7% increase (p = 0.02) in ETCO2 with every 10-compression/min increase in chest compression frequency [25][50].5. Conclusions
Modern CPR is a crucial step in basic life support, and to improve the quality of CPR and minimize the risk of injury, real-time and effective CPR feedback is vital. CPR feedback devices can truly improve CPR quality in training and real life. In complex out-of-hospital settings such as accidents, they can also provide effective assistance and improve the efficiency of treating cardiac arrest patients, thus exhibiting a broad scope of applicability. Over time, CPR feedback devices have evolved from simple visual and auditory feedback based on manual compression to personalized feedback from automated CPR machines using real-time physiological monitoring. The latest CPR devices leverage technological advancements to provide increasingly intelligent feedback, incorporating a diverse range of monitoring data with deep learning algorithms to predict blood flow perfusion and support accurate compression.
