Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Christian Barbato and Version 2 by Sirius Huang.
The treatment of unresectable or metastatic Head and Neck Squamous Cell Carcinoma (HNSCC) has traditionally relied on chemotherapy or radiotherapy, yielding suboptimal outcomes. The introduction of immunotherapy has significantly improved HNSCC treatment, even if the long-term results cannot be defined as satisfactory. Its mechanism of action aims to counteract the blockade of tumor immune escape. This result can also be obtained by stimulating the immune system with vaccines.
- head and neck squamous cell carcinoma (HNSCC)
- therapeutic cancer vaccine
- Epstein–Barr virus (EBV)
- human papilloma virus (HPV)
- mRNA vaccine
1. Introduction
Head and neck squamous cell carcinoma (HNSCC) affects 450,000 individuals per year, accounting for an estimated 890,000 new cases, i.e., roughly 4.5% of all cancer diagnoses. The HNSCC incidence includes 380,000 cases of cancer of the oral cavity and the lip, 133,000 of the nasopharynges, 98,000 of the oropharynges, 84,000 of the hypopharynxes, 185,000 of the larynxes, and 54,000 of the salivary glands. The incidence and mortality rates of HNSCC are distributed across geographic regions and demographic traits, with a higher occurrence in men than in women and a male-to-female ratio of 2:1 [1].
In situations where surgical intervention is not viable, chemotherapy and radiation therapy are used. However, results are not optimal, particularly for recurrent or metastatic malignancies. The introduction of immunotherapy has improved those outcomes. Currently approved drugs for the treatment of HNSCC are pembrolizumab (KEYTRUDA, Merck and Co., Rahway, NJ, USA) and nivolumab (OPDIVO, Bristol Myers Squibb, New York, NY, USA), which have improved traditional chemotherapy results. Checkmate-141, Keynote-040, and Keynote-048 trials are milestones in HNSCC treatment and set a new standard of results for non-surgical therapy. However, they still are not satisfactory with long-term efficacy in 20 to 30% of patients only. The discussion of resistance mechanisms to immune checkpoint inhibitors is beyond the scope of this manuscript, but we can state that solutions need to be found to achieve better therapy performance [2][3][4][2,3,4].
In this scenario, the advancement of novel non-surgical therapies appears to be imperative. HNSCC are categorized as HPV-negative and HPV-positive. Tobacco consumption is the primary risk factor for the development of HPV-negative HNSCC. In addition, betel quid, areca nut, exposure to environmental pollutants, or excessive alcohol consumption is known to synergize with tobacco use to promote carcinogenesis [5][6][5,6]. While the tobacco- and alcohol-related neoplasms are decreasing, viral infection is on the rise. HPV is a common risk factor for HNSCC, being associated with oropharyngeal cancers (>70%) [7]. HPV vaccines have been approved for cervical cancer prevention in females, and their impact on HNSCC incidence has been observed [6]. However, therapeutic vaccines for HNSCC are still undergoing investigation. Their objective is to induce immunogenicity against HNSCC cells employing a range of mechanisms, including traditional approaches like cell-mediated cytotoxicity induced by antigens, as well as innovative strategies to counteract tumor immune escape mechanisms or stimulate the immune system’s cytotoxic activity against neoplastic cells [5].
2. Immunosurveillance and Immune Escape Mechanisms
The immune system plays a crucial role in the uncontrolled growth and spread of neoplastic cells, as seen via immunosurveillance [7]. It can eliminate cancer cells that are constantly produced throughout an individual’s life. During neoplastic progression, several mutations in cancer cell DNA permit the acquisition of the ability to evade the immune response through the downregulation of HLA antigens, a decrease in or loss of expression of tumor-associated antigens, and the production of immunosuppressive cytokines [8]. Tumor antigens are taken up by antigen-presenting cells (APCs), such as dendrites, and are exposed to host T lymphocytes, which in turn form effector and memory T lymphocytes. Cytotoxic T lymphocytes and natural killer cells circulate in the peripheral blood and lymphoid and non-lymphoid tissues, as well as in tumoral tissues [9]. T cells encounter tumor cells equipped with these same antigens and become activated and kill them through a cytotoxic mechanism. Cancer cell death is induced via the release of cytokines such as interferon (IFN)-γ, tumor necrosis factor (TNF)-α, granzyme, perforins, and IL-2 [10][11][10,11]. To proliferate freely, tumors may develop immune escape mechanisms via cytotoxic T-lymphocyte protein 4 (CTLA4) and programmed cell death protein 1 (PD-1). Immunotherapy drugs have been developed to inhibit these molecules and allow the immune system to act on tumors [2][3][2,3]. In addition to the molecular mechanisms of immune escape expressed on the surface of tumor cells, there are several others that involve the tumor microenvironment. These include increases in the percentage of immunosuppressive cells in the tumor matrix (myeloid-derived suppressor cells, tumor-associated macrophages, and T regulatory cells); the secretion of immunosuppressive molecules, such as transforming growth factor-β (TGF-β); and the signal transducer and stimulator of transcription (STAT)-3, as well as the formation of physical barriers and an intricate vascular network that physically prevents the penetration of immune cells into the tumor matrix [5][12][5,12].3. Anticancer Vaccine Categories
The anticancer vaccines under study can be divided into two groups: traditional vaccines that induce a T cell-mediated immune response against specific tumor antigens, and less conventional vaccines targeting immune escape mechanisms [5][11][5,11]. Autologous vaccines, which utilize patient-specific antigens, offer a highly targeted and specific immune response. However, the complex process, including the extraction and inactivation of tumor cells, as well as the associated development costs and lack of standardization, pose challenges to their widespread use. As a result, recombinant vaccines, which are generated through the laboratory synthesis of tumor antigens, are being subjected to more extensive trials. These recombinant vaccines offer potential advantages in terms of standardization and scalability [5].4. Anticancer Vaccine Antigens
The antigens expressed by tumors are divided into vague categories, and some antigens may belong to more than one. According to the classification of Zarour et al., those categories are oncofetal, oncoviral, overexpressed/accumulated, cancer-testis, linear-restricted, mutated, post-translationally altered, or idiotypic antigens (Table 1) [13][14][15][16][13,14,15,16]. Tumor antigens recognized by T lymphocytes can also be classified as shared antigens, tumor-associated antigens, and tumor-specific antigens, according to Coulie et al. [17].Table 1.
Categories of tumor antigens.
| Categories of Tumor Antigens | Description |
|---|---|
| Classification by Zarour et al. | |
| Oncofetal | Usually expressed in fetal tissues |
| Oncoviral | Encoded by virus DNA/RNA |
| Overexpressed/Accumulated | Expressed in both healthy and neoplastic tissues with higher levels in cancer cells |
| Cancer-testis | Expressed in adult reproductive tissues physiologically and in neoplastic cells |
| Linear-restricted | Expressed by specific cancer histotypes |
| Mutated | Only expressed by cancer |
| Post translationally altered | Post-transcriptional alteration of molecules |
| Idiotypic | Highly polymorphic genes expressed in a specific “clonotype” in cancer tissues |
| Classification by Coulie et al. | |
| Shared antigens | Expressed both by tumor and healthy cells |
| Tumor associated antigens | Antigens expressed by tumor and healthy cells that are upregulated in cancers |
| Tumor specific antigens | Expressed only by tumor cells |
5. Anticancer Vaccine Platforms
Devaraja et al. [5] conducted a classification of anticancer vaccine platforms, elucidating the advantages and disadvantages associated with each of them (Figure 12).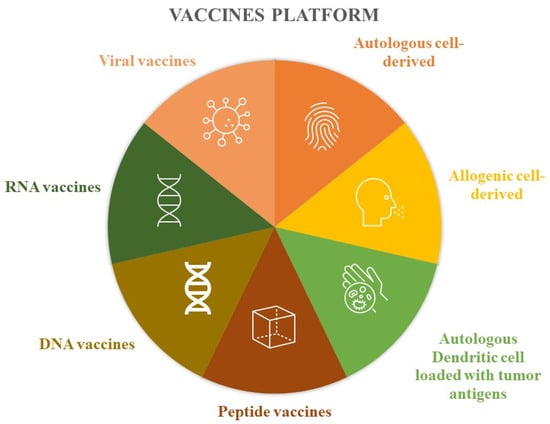
Figure 12.
Vaccine platforms.
Table 2.
Advantages and disadvantages of vaccine platforms.
| Vaccines Platform | Advantages | Disadvantages |
|---|---|---|
| Autologous cell-derived | Exposed to all patient tumor antigens Vaccine designed for specific patient disease |
Difficult to manufacture. not standardizable. requires sufficient tissue biopsy |
| Allogenic cell-derived | More potential antigens available; standardization; lower costs |
Less personalization |
| Autologous dendritic cell loaded with tumor antigens | Dendritic cells are the most powerful antigen-presenting cells | Require leukaphereses; require cell culture processing |
| Peptide vaccines | Easy to produce; easy to store; no viral component |
Easy tolerance; rapid degradation in human body; usually require immunogenic adjuvants |
| DNA vaccines | Use of multiple genes; can be combined with immunostimulatory agents |
Modest efficacy; risk of genetic recombination |
| RNA vaccines | Low levels of side effects; low levels f autoimmune disease |
Rapid degradation |
| Viral vaccines | Induce immune and cell-mediated responses |
6. Virus Infection-Based Cancer Vaccines
6.1. Epstein–Barr Virus (EBV)-Related Nasopharyngeal Carcinoma (NPC) Vaccines
Therapeutic vaccination has been extended to NPC in view of its association with EBV. The approaches developed are based on a dendritic cell-based strategy and use virus-based vaccines. Virus-induced malignancies have multiple therapeutic targets due to non-self-origin. The Epstein–Barr virus nuclear antigen-1 (EBNA1) and the Epstein–Barr virus latent membrane proteins 1/2 (LMP1/2) are target antigens. Four trials (NCT01256853, NCT01800071, NCT01147991, NCT01094405) investigated the efficacy of EBNA1 C-terminal/LMP2 chimeric protein-expressing recombinant modified vaccinia, the Ankara vaccine (MVA) [18]. The study of Trabecutel (Atara Biotherapeutics) and allogenic EBV-T-cell immunotherapy was suspended after phase 1B by the sponsor and phase 2 was never conducted. The trial NCT03769467 was a multicenter, open-label, single-arm phase 1B/2 study to assess the safety and efficacy of Trabecutel in combination with pembrolizumab for the treatment of platinum-pretreated patients with recurrent/metastatic EBV+ NPC (Figure 23).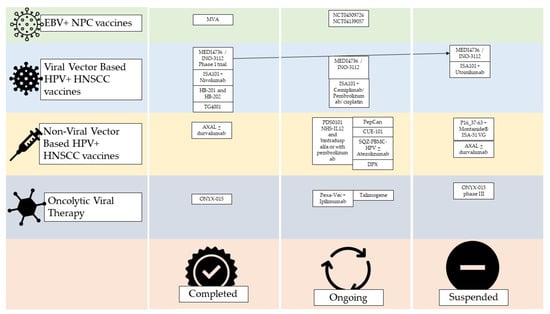
Figure 23. Current status of virus based HNSCC vaccine trials on humans. Unless otherwise stated, the studies considered were phase 1 or 2. Completion does not indicate the success of the therapy, but only the end of the study and the publication of its data. EBV = Epstein–Barr virus; NPC = nasopharyngeal carcinoma; HPV = human papilloma virus; HNSCC = head and neck squamous cell carcinoma; MVA = modified Ankara vaccine; DPX = DepoVaxTM.
6.2. HPV+ HNSCC Vaccines
Viral Vector-Based HPV+ HNSCC Vaccines
HPV+ HNSCC vaccines are different from prophylactic HPV vaccines such as Gardasil (Merck and Co., Rahway, NJ, USA) and Cervarix (GlaxoSmithKline Biologicals, Rixensart, Belgium), which target the L1 capsid protein of the virus. Infected cancer cells do not express L1, but they need the oncoproteins E6 and E7, which are induced by the virus. The therapeutic vaccines under development target those proteins from HPV-16 and -18. For example, MEDI4736 also known as INO-3112 is a DNA-based vaccine with two components, one targeting E6 and E7 antigens from HPV-16 and -18 and another that encodes for a recombinant interleukin IL-12. The vaccine has been studied in a phase Ib/II trial involving 18 HNSCC HPV+ patients and 18 out of 21 showed antigen-specific T cell activity and persistent cellular response after 1 year. The authors concluded that INO-3112 can generate durable peripheral and tumor immune responses and hypothesized that it could be used in association with immune checkpoint inhibitors [19]. INO-3112 was studied in the suspended NCT04001413 studies and two studies in combination with durvalumab in the treatment of recurrent or metastatic HNSCC. In the first, 35 patients were enrolled, but 17 patients died during the study and 13 did not complete follow-up (NCT03162224); the second, preliminary unpublished data, and the study population was composed of any HPV+ cancer (not just head and neck) and to date, the study is indicated as ‘active’ and ‘not recruiting’ (NCT03439085) (Figure 23). ISA101, a synthetic long-peptide HPV-16 vaccine inducing HPV-specific T cells, was studied in combination with Nivolumab in 24 patients, including 22 with oropharyngeal cancer (phase 2). The authors observed an overall response rate of 33%, with a median duration of response of 10.3 months and a median overall survival of 17.5 months, and only two grade 3 or 4 toxicity events were reported [20]. The efficacy of ISA101 in combination with Cemiplimab, Pembrolizumab, cisplatin, or Utomilumab, is ongoing (phase2), but no preliminary results have been published (NCT03669718, NCT04369937, NCT04398524). In addition, the association of ISA101 and Utolimumab (NCT03258008) was discontinued (Figure 23). Choriomeningitis lymphocytic virus and Pichinde virus were used as two vaccines against the HPV16 E6E7 fusion protein. HB-201 and HB-202 were evaluated in the NCT04180215 trial. It is interesting to observe how intratumoral administration is being evaluated for these vaccines, alone or combined with systemic administration, as well as parenteral administration. Furthermore, the authors also experimented with the alternating administration of the two drugs, observing greater immunogenicity than with the exclusive use of one of the two (Figure 23) [21]. The vaccine TG4001 (Tipapkinogene sovacivec) is formed via an attenuated viral vector expressing the coding sequences for the E6 and E7 proteins of HPV-16 and -18, and IL-2. A phase 1B/2 study was conducted, and among nine patients enrolled, five with head and neck cancer, only three showed T-mediated peripheral immunity against E6/E7, and four showed increased CD8 infiltrate and/or T-reg/CD8 ratio in the neoplastic tissue (Figure 23) [22].Non-Viral Vector-Based HPV+ HNSCC Vaccines
SQZ-PBMC-HPV (SQZ Biotechnologies, Watertown, MA, USA) is a vaccine produced using a proprietary technology called cell squeeze technology, which acts on circulating mononuclear cells. Phase 1 trial NCT04084951 evaluated its safety and efficacy in monotherapy and association with atezolizumab (Tecentriq) or any other ICI, in patients with locally advanced, recurrent, or metastatic HPV+ cancers, including HNSCC. Preliminary results showed good tolerability and immune response, even though the HNSCC population was only 3 out of the total 12 (Figure 23) [23]. PDS0101 is a liposomal-based vaccine against HPV16 E6 and E7 proteins that also contain R-DOTAP, a lipid under evaluation for anti-HPV+ and HNSCC activity. This vaccine is under study in combination with NHS-IL12 and bintrafusp alfa or with pembrolizumab. NHS-IL12 is an immunocytokine that results in IL-12, and bintrafusp alfa is a molecule obtained by combining a human IgG1 against PD-L1 and the extracellular domain of the TGF-β receptor type II, and the result is an action against TGFβRII. Their associations with PDS0101 are under evaluation in the NCT04287868 trial, whose recruitment is expected to end on 1 January 2024, and no preliminary results have been published yet. The case of the association with pembrolizumab in the trials NCT04260126 (VERSATILE002) and NCT05232851 is different, as preliminary results have been disclosed. The phase II study VERSATILE002 has a population of patients affected by recurrent or metastatic HNSCC, who are positive for both HPV 16 and PD-L1. The phase 1/2 trial NCT05232851, however, has a population of patients with locally advanced squamous cell carcinoma of the oropharynx. PDS0101 and pembrolizumab were well tolerated with no significant toxicity in the enrolled population [24]. Their combination showed significant anti-tumor activity and the FDA granted the Fast Track designation to this association for use in recurrent or metastatic HPV16+ and HNSCC (Figure 23) [25]. AXDS 11-001, also known as Axalimogene Filolisbac or AXAL (Advaxis Inc., Princeton, NJ, USA), is based on the bacterium Listeria monocytogenes listeriolysin O, modified to secrete the HPV-E7 tumor antigen as a fusion protein called LLO-E7 [26]. The NCT02002182 trial enrolled 15 patients divided into two groups, in one of which the vaccine was administered before transoral robotic surgery in the treatment of squamous cell carcinoma of the larynx, while the other group was directly subjected to surgery to evaluate the immune response induced by the vaccine. Only nine patients completed the study, five in the experimental group and four in the control group. ADXS 11-001 showed increased systemic immune response and CD4+ and CD8+ T cell infiltration. At the same time, the vaccinated subjects had an incidence of adverse events of 55.5% compared to 16.7% in the control group [26]. The suspicion of adverse events associated with this type of drug seems to have been increased by two further trials, NCT02291055 and NCT01598792. The first involved a combination of AXAL and durvalumab and was put on hold due to the death of a patient. The second, concerning HPV16+ oropharyngeal carcinoma, had only two patients enrolled and was suspended because one experienced dose-limiting toxicity (Figure 23) [27].7. Oncolytic Viral Therapy
The use of viruses as weapons to kill cancer cells was pioneered over 20 years ago. ONYX-015 first entered clinical trials in 1996; it is an adenovirus with a deletion of the E1B gene engineered to selectively lyse p53-deficient neoplastic cells and not attack healthy cells. The drug has been tested using intratumor administration. Post-treatment biopsies showed the presence and/or replication of the virus in 7 of 11 patients in the tumor but not in the immediately adjacent tissues. A total of 21% of patients showed tumor regression with a volume greater than 50% and no alterations of the surrounding tissues [28][29][35,36]. Intratumoral ONYX-015 has also been studied in combination with the systemic administration of cisplatin and 5-fluorouracil. The rationale behind Khuri et al. attempting this approach was that while ONYX-015 demonstrated efficacy in HNSCC, the disease rapidly relapsed. The scholars observed a response in all patients treated with the combination, while the group treated only with traditional chemotherapy underwent progression. Again, the intratumor replication of the virus was confirmed by biopsies [30][37]. In 2001, the use of ONYX-015 was also tested intravenously in patients with metastatic solid tumors. The authors observed an increase in neutralizing antibodies and several inflammatory cytokines. But, in this study, only two of the patients had HNSCC [31][38]. Given the promising results of the phase 2 studies regarding ONYX-015, a phase 3 study has been reported to have taken place more than 20 years ago, but no data are available [32][33][34][39,40,41]. Pexa-Vec is an oncolytic virus vaccine derived from the Wyeth-strain that has been genetically modified to express the huma GM-CSF. The mechanism of action includes the activation of dendritic cells and the enhancement of the tumor immune infiltrating cells. The association of Ipilimumab with the treatment of locally advanced, recurrent, or metastatic solid cancers, including HNSCC, is under evaluation in the NCT02977156 trial. Talimogene is derived from the herpes virus carrying GM-CSF, and its association with pembrolizumab demonstrated a tolerable safety profile, but the efficacy was similar to that of pembrolizumab monotherapy in historical HNSCC trials (Figure 23) [35][42]. H101 is another oncolytic adenovirus-based vaccine like ONYX-015. Its intratumorally administration associated with systemic chemotherapy has been compared with chemotherapy alone. The combination arm showed a higher response rate (79% vs. 39.6%, p < 0.001). In 2005, the Chinese government approved the H101 vaccine in combination with cisplatin-based chemotherapy for the treatment of nasopharyngeal carcinoma (Figure 23).8. Cancer Testis Antingen-Based Vaccines
The most frequently over-expressed cancer testis antigens in HNSCC are from the MAGE group [36][43]. A pilot study using Trojan vaccines demonstrated acceptable toxicity and systemic immune responses against HLA-II-restricted epitopes in five MAGE-A3/HPV 16+ patients with recurrent or metastatic (R/M) HNSCC. Montanide ISA 51 and GM-CSF were used as adjuvants to facilitate dendritic cell migration to the vaccination site and enhance antigen presentation [37][44]. A phase 1 trial (NCT00257738), involving additional cases of progressive recurrent or metastatic HNSCC (HLA A2+), confirmed the feasibility and safety of these vaccines. Unfortunately, the trial, originally intended to enroll 90 cases, prematurely closed due to poor accrual after enrolling only 17 patients (Figure 34). Any immunized patients in both studies demonstrated partial or complete clinical response. The efficacy of a dual-antigenic peptide vaccine comprising MAGED4B and four-jointed box 1 (FJX1) was studied, evidencing strong immunogenic responses with the peptide combination compared to individual use. These have only been studied in vitro or in mouse models (Figure 34) [38][39][45,46].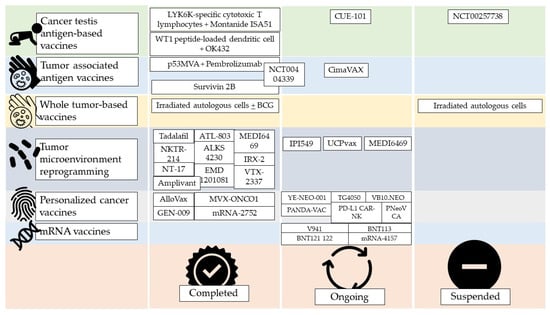
Figure 34. Current status of non-virus-based HNSCC vaccine trials on humans. Unless otherwise stated, the studies considered were phase 1 or 2. Completion does not indicate the success of the therapy but only the end of the study and the publication of its data. MVA = modified Ankara vaccine.
