Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Khanisyah Erza Gumilar and Version 3 by Lindsay Dong.
Heat shock factor 1 (HSF1) is a transcription factor crucial for cellular stress responses. HSF1 activates heat shock proteins (HSPs) in response to proteotoxic stress, aiding in protein folding and maintaining proteostasis. HSF1 is often overexpressed in various cancer cells, fueling malignancy and indicating a poor prognosis. The mechanisms behind HSF1-induced tumorigenesis are complex and cancer type-dependent. Targeting HSF1 presents a novel cancer treatment strategy.
- HSF1
- heat shock response
- cellular stress
- cancer stem cells
1. Introduction
The transcription factor heat shock factor 1 (HSF1) is crucial in regulating the heat shock response (HSR). HSR is a primary protective mechanism responding to stressful conditions such as elevated temperatures, oxidative stress, heavy metals, and proteotoxic insults [1][2][1,2]. When cells are exposed to proteotoxic stress, HSF1 induces the expression of heat shock proteins (HSPs) to act as chaperones, correcting the protein-folding process and maintaining proteostasis [2][3][2,3]. Beyond HSR, numerous studies demonstrate that HSF1 orchestrates transcriptional programs distinct from HSR and impacts cell proliferation, survival, and metabolism related to cancer [4][5][6][4,5,6]. HSF1 is overexpressed in multiple cancer types, and its activation supports malignancy and leads to poor prognosis [7][8][9][7,8,9]. As a result, HSF1 is a potential biomarker for identifying the malignancy of cells [10]. The mechanisms of HSF1-induced tumorigenesis are complex and involve diverse pathways, depending on the cancer type. Given the essential role of HSF1 in cancer, researchers are discovering the functions of HSF1 in tumorigenesis and developing HSF1 inhibitors as part of innovative targeted therapy [11].
HSF1 plays an important role in the progression of various cancer types, including those of the breast, lung, ovary, endometrium, and prostate and many other cancers. HSF1 has been reported to control critical oncogenic pathways, influencing cell cycle progression, apoptosis, and angiogenesis. Moreover, its potential to impact immunological responses, modulate the tumor microenvironment, and contribute to the development of therapeutic resistance highlights its importance in cancer biology.
 HSF1 binds to the HSE and functions as a critical regulator of HSR, triggering the transcription of genes encoding HSPs to prevent further damage by protein misfolding and aggregating [1][18][1,18]. However, recent studies discovered that, in addition to cytoprotective properties, continuous activation of HSF1 increases cell proliferation and survival and reprograms cell metabolism, similar to cancer cells [4][5][6][4,5,6]. Therefore, research focused on HSF1-induced tumorigenesis has increased dramatically.
HSF1 binds to the HSE and functions as a critical regulator of HSR, triggering the transcription of genes encoding HSPs to prevent further damage by protein misfolding and aggregating [1][18][1,18]. However, recent studies discovered that, in addition to cytoprotective properties, continuous activation of HSF1 increases cell proliferation and survival and reprograms cell metabolism, similar to cancer cells [4][5][6][4,5,6]. Therefore, research focused on HSF1-induced tumorigenesis has increased dramatically.
 HSF1 inhibition has emerged as a possible therapeutic strategy in cancer treatment. HSF1 inhibition has been demonstrated to sensitize cancer cells to chemotherapy, diminish tumor growth, and improve radiation therapy efficacy. Furthermore, HSF1 has emerged as a promising target for cancer therapy.
HSF1 inhibition has emerged as a possible therapeutic strategy in cancer treatment. HSF1 inhibition has been demonstrated to sensitize cancer cells to chemotherapy, diminish tumor growth, and improve radiation therapy efficacy. Furthermore, HSF1 has emerged as a promising target for cancer therapy.
2. HSF1 Biology
2.1. HSF1 Structure and Function
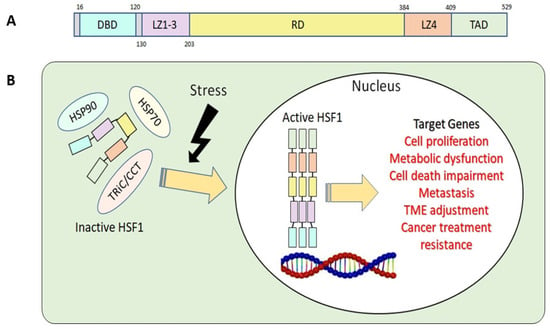
The structure of the HSF1 protein can be divided into five parts according to their functions: the DNA-binding domain (DBD), leucine zipper 1-3 (LZ1-3), the regulatory domain (RD), leucine zipper 4 (LZ4), and the transactivation domain (TAD) (Figure 1A) [12][13][12,13]. Under stress conditions, the N-terminal DBD binds to the target genes’ heat shock element (HSE) during HSR. This binding process requires HSF1 homotrimer formation and subsequent activation [14]. To avoid the continuous activation of HSF1, LZ1-3 and LZ4 form intramolecular interactions to keep HSF1 in its monomeric form and inactive [15]. RD, the domain between LZ1-3 and LZ4, provides an alternative way to regulate HSF1 positively or negatively via modification of specific amino acid residues, known as post-translational modification (PTM) [12][15][16][12,15,16]. Lastly, the C-terminal TAD is related to cell survival once cells undergo heat shock [17].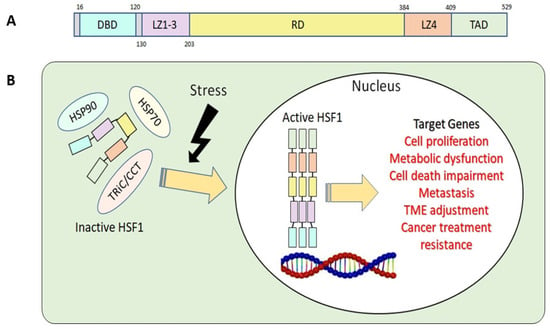
Figure 1. (A) Basic structure of human HSF1. DBD, DNA-binding domain; LZ1-3, leucine zipper 1-3; RD, regulatory domain; LZ4, leucine zipper 4; TAD, transactivation domain. (B) HSF1 activation related to tumorigenesis.
2.2. HSF1 Regulatory Mechanisms in Normal and Cancer Cells
HSF1 undergoes regulation through various mechanisms, such as intrinsic regulation by LZ1-3 and LZ4 and interactions with chaperones/chaperonins. Additionally, it is subject to various post-transcriptional and post-translational regulatory processes. [12][15][12,15]. Furthermore, a recent study also indicated that HSF1 is regulated by non-coding RNA [19]. Upon activation of HSF1 due to stress, it assembles into homotrimers, moves from the cytosol to the nucleus, initiates HSP transcription, and activates HSR. In the nucleus, HSF1 binds to various target genes and activates their respective functions and roles (Figure 1B). As chaperones accumulate in response to HSF1 activation, they engage with HSF1, holding it in the cytosol as a monomer. This interaction attenuates HSRs by rendering HSF1 inactive [12]. This negative-feedback pathway prevents HSF1 overactivation [20]. The regulatory mechanism of HSF1 hinges on post-translational modifications, a process wherein changes occur to the protein after it has been synthesized, for example, phosphorylation [21][22][23][24][25][21,22,23,24,25], acetylation [26][27][26,27], and SUMOylation [28]. These modifications play a pivotal role in fine-tuning HSF1 activity, influencing its ability to form functional complexes, translocate to the nucleus, and trigger downstream cellular responses. HSF1’s regulatory mechanisms can be changed in cancer cells, resulting in different patterns of activation and function. Even under non-stress settings, many cancer cells have a heightened and constitutive activation of HSF1. This persistent activation in cancer cells promotes survival and proliferation by increasing the expression of chaperone proteins and anti-apoptotic molecules, which aid in managing proteotoxic stress within rapidly growing malignant cells.3. HSF1 Involvement in Various Cancer Types
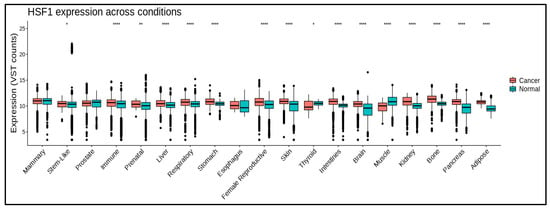
HSF1 promotes tumor progression and survival via a variety of methods. It controls gene expression during the cell cycle, apoptosis inhibition, tumor microenvironment modification, angiogenesis, and metastasis. HSF1 expression (Figure 2) is associated with poor prognosis and treatment resistance in various malignancies, including breast, prostate, lung, and ovarian cancers (Table 1). Some studies also suggest that HSF1 expression in tumor tissue also increases significantly according to clinical stage [29][30][31,32]. However, in some cancers, there are no significant correlation between HSF1 expression and clinical stage (Figure S1).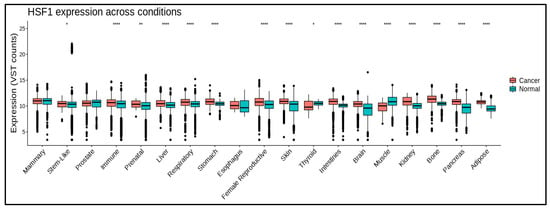
Figure 2. HSF1 mRNA levels in different cancers and normal tissues. HSF1 expression is significantly higher in some cancerous conditions. * means p ≤ 0.05; ** means p ≤ 0.01; **** means p ≤ 0.0001. Data are processed using https://gccri.bishop-lab.uthscsa.edu/correlation-analyzer/ (accessed on 10 October 2023).
4. HSF1 in Therapeutic Resistance
While chemotherapy or radiotherapy remains the primary approach for treating various cancer types, the ongoing challenge lies in the development of drug resistance by cancer cells despite notable advancements in treatment. Multiple factors contribute to this resistance, with one of the factors being the overexpression or activation of HSF1. Various cancer cells exhibit increased levels of HSF1, and this upregulation is linked to resistance against chemotherapy. Activated HSF1 boosts the production of HSPs, shielding cancer cells from the harmful impact of chemotherapy drugs. HSPs play a role in preventing protein misfolding and aggregation, aiding protein folding and breakdown, and inhibiting apoptosis—all contributing factors to the development of resistance to chemotherapy [28][31][32][33][34][35][28,62,75,76,77,78]. Cancer cells are stressed when subjected to chemotherapeutic drugs, which can activate HSF1 and the transcription of HSP70 and HSP90, further contributing to therapeutic resistance [36][37][68,79]. In addition to its role in HSP regulation, HSF1 also promotes tumor cell survival and proliferation by activating the expression of genes involved in cell cycle regulation [38][39][40][80,81,82], DNA repair [38][41][80,83], and angiogenesis [42][43][84,85]. Inhibition of HSF1 has been shown to sensitize cancer cells to chemotherapy and reduce tumor growth. Therefore, targeting HSF1 may provide a promising strategy for overcoming chemotherapy resistance in cancer treatment [44][45][46][69,86,87]. HSF1 is also a crucial factor in the transcriptional activation of multidrug resistance 1 (MDR1), which is involved in chemoresistance. The pivotal role of HSF1 in drug resistance can be demonstrated in the binding of HSF1 to the HSE of MDR1. Transfection of active HSF1 increases MDR1 mRNA and protein levels, stimulating drug efflux and the development of drug resistance [47][48][39,46]. On the contrary, HSF1 depletion downregulates the transcription of the MDR1 gene in the cells [49][88]. Another mechanism of multidrug resistance involves the ATP-binding cassette (ABC) transporters, which pump hydrophobic molecules out of the cell. The increasing efflux of drugs mediated by the ABC transporters is one of the most common mechanisms of drug resistance [50][89]. HSF1 promotes the activation of ABCB1, an ABC transporter. In melanoma cells with HSF1 overexpression, upregulation of ABCB1 gene transcription was prominent. The expression of the ABCB1 gene was found to be primarily dependent on HSF1 in all tested doxorubicin- and paclitaxel-resistant melanoma cell lines [51][90]. In addition to chemoresistance, HSF1 also plays a role in protecting cancer cells from the effects of radiotherapy by boosting the expression of HSPs [52][53][54][93,94,95]. Overexpression of HSF1 leads to radiotherapy resistance in cancer cells. HSF1 activation leads to the upregulation of genes involved in DNA repair, including Rad51, a protein involved in homologous recombination repair, a critical pathway for repairing DNA double-strand breaks induced by ionizing radiation [41][55][56][83,96,97]. Furthermore, HSF1 has been shown to regulate the expression of several anti-apoptotic genes, including Bcl-2 [57][58][98,99], which can protect cancer cells from radiation-induced apoptosis. HSF1 has also been shown to activate the NF-κB pathway [59][60][61][100,101,102], which regulates inflammation and immune responses. These three mechanisms may enhance radioresistance by inducing the expression of several pro-survival genes, including HSPs. High expressions of HSP27, HSP70, and HSP90 exert a radioresistant effect through the anti-apoptotic signaling pathway. In experiments using radioresistant lung cancer cells, a knockdown of HSF1 and administration of an HSP90 inhibitor resulted in a high level of cell apoptosis and increased cell sensitivity to radiotherapy [62][103]. Apart from these positive effects, the inhibition of HSP90 induces the release of HSF1 from the HSP90 complex, thereby stimulating the transcription of the cytoprotective chaperones HSP70 and HSP27 [8][63][64][8,42,104]. Therefore, this forms a feedback loop to counteract the effect of HSP90 inhibition.5. Targeting HSF1 for Cancer Treatment
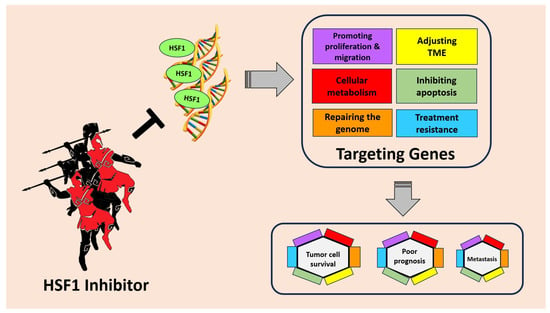
Inhibitors of HSF1 are compounds designed to block or modulate the activity of HSF1. These inhibitors have been studied for their potential therapeutic applications, especially in cancer treatment, where HSF1 is often upregulated and contributes to the survival and growth of cancer cells. Targeting HSF1 for cancer treatment holds great promise as an innovative therapeutic strategy. HSF1, known for its role in cellular stress response, has emerged as a critical regulator in tumorigenesis. In cancer cells, HSF1 becomes hyperactivated, leading to the overexpression of genes involved in anti-apoptotic mechanisms and cellular metabolism. This heightened HSF1 activity also promotes the migration and invasion of cancer cells, facilitating tumor spread to distant sites. Moreover, HSF1 contributes to drug resistance, making cancer treatments less effective (Figure 3).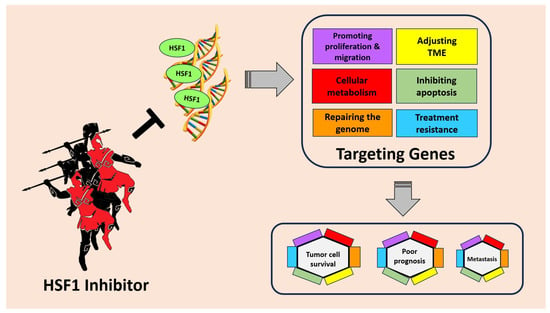
Figure 3. HSF1 plays an important role in tumor cell survival, poor prognosis, and metastasis through several mechanisms. HSF1 can increase the expression of genes involved in anti-apoptotic mechanisms, cellular metabolism, promoting migration, and even drug resistance. By inhibiting HSF1, cancer progression can be suppressed and provide better hope to patients.
In light of these findings, scientists have explored inhibiting HSF1 as a potential therapeutic approach (Table 2). By targeting HSF1, researchers aim to disrupt the pro-cancer effects of this transcription factor. Targeting HSF1 as a cancer therapy is currently in the pre-clinical stage, and it is regarded as a promising cancer treatment strategy. In several malignancies, a decrease in HSF1 activity can inhibit aneuploidy and cancer cell proliferation [64][104].
Despite successfully blocking HSF1 in vitro and in animal models, each agent has therapeutic limitations. Under stress, HSF1 plays a vital role in cancer and normal cells. Inhibiting HSF1 for anti-cancer treatment can be harmful to normal cells. As a result, it is critical to specifically identify and target cancer cells to reduce cytotoxic effects on normal cells. This necessitates the improvement of existing drugs through synthetic techniques that change functional groups/motifs or the identification and isolation of new natural molecules capable of overcoming possible off-target difficulties [65][107].
Most current inhibitors indirectly interfere with HSF1, lacking specificity and potency. Developing direct small-molecule inhibitors for HSF1 is challenging due to its complex structure. Moreover, the mechanisms of HSF1 in tumorigenesis and development are complicated, involve diverse signaling pathways, and may depend on different cancer types. Recent advancements in HSF1 drug development have brought renewed hope, exemplified by the discovery of direct HSF1 inhibitors such as DTHIB [29][66][31,108] and CCT361814 [67][68][69][109,110,111]. These inhibitors have demonstrated potent and specific suppression of tumor growth in pre-clinical animal studies while displaying low toxicity to normal tissues. Encouragingly, CCT361814 has entered Phase I clinical trials. The prospect of developing new generations of HSF1 inhibitors, especially those directly targeting HSF1 itself, holds promise.
A lack of possible target locations in the tertiary structure makes developing HSF1 inhibitors problematic. HSF-1 is a transcription factor with relatively weak “druggability” [65][70][107,112]. Furthermore, its complex activation pathway involves several components, including multichaperone complexes and various PTMs. Nonetheless, promising HSF1 inhibitors have been developed, frequently derived from natural compounds or synthesized chemical structures [46][71][87,113]. Below are examples of HSF1 inhibitors tested in vitro and in vivo. So far, NXP800 (CCT361814) is the only HSF1 inhibitor that has entered clinical trials. It is expected that, in the near future, other HSF1 inhibitors will enter clinical trials.
