1. Mesenchymal Stem Cells as Drug Vehicles: Nanoparticles as Drug Carriers
Nanoparticle-based biomimetic systems provide an alternative treatment for drug delivery, but they still lack active targeting capability. Nanoparticle technology has managed to improve the capacity of MSCs as drug carriers by enhancing their homing as antitumor agents
[1][24]. The progression in the field of genetic engineering, biomaterials
[2][25], and nanotechnology has contributed to a better understanding on the role of mesenchymal (MSC), as drug carriers with nanoparticles
[3][26]. In particular, human mesenchymal stem cell (hMSC)-based therapy can enhance the homing of exogenous MSCs, which could be drug carriers
[4][27]; this enhanced capacity of MSC could be interesting from a clinical viewpoint
[5][12]; cancerous stem cells have the ability to self-renew and contribute to tumor metastasis and pharmacological resistance to drugs could be solved by MSC treatment against cancer since MSCs could release cytotoxic agents in the tumor microenvironment for its eradication
[6][28]; In fact, MSCs could act as a “Trojan horse” able to transport the oncolytic viral load to disseminate tumor beds for its eradication. Another strategy is the use of cell membrane-coated nanoparticles
[7][29]. In this way, even MSC-derived producers such as exosomes from bone marrow (MSC-BMSC) could prevent osteosarcomas growth in vitro
[8][16]. The CXCR4 inclusion in these nanoparticles could be an effective strategy for enhancing the homing of MSC toward tumors such as
reswe
archers mention earlier
[9][30]; the ability of MSCs as drug carriers is also enhanced by spheroidal nanoparticle technology, which facilitates the transport of “drugs/therapeutic agents” within MSCs
[10][31]. However, a limited capacity of homing towards the target tissue makes its clinical translation by reducing the release of “loaded drug” inside the tumor site. In addition, the risk of low viability of MSCs decreases the capacity to transport drugs
[11][32]. The monitorization of transplanted MSC cells in vivo with nanoparticles is possible; however, these NP can provoke cell aggregation, infections, or induce differentiation to an unexpected cell type or event risk of embolism in case of i.v infusion. These limitations reduce the efficacy of NP and consequently decrease the antitumoral capacity of MSC
[12][33].
CXCR4 plays a role in chemotaxis, adhesion, and migration, which contribute to tumor metastasis by a CXCR4 overexpression signaling pathways in tumor cells; these NP are carriers of si-RNA for CXCR4 while the CXCR4 blockade by AMD-3100 chemokine blocker can prevent tumor growth in vitro models of cancer
[13][34]; in fact, genetically engineered mesenchymal stem cell (BM-MSC: bone marrow mesenchymal stem cells) membrane-derived nanoparticles that overexpress CXCR4, enhanced the migration capacity toward the tumor locations; these cancer cells are identified using fluorescent NP in the site of tumor. From this perspective, several studies have demonstrated antitumoral effects of MSC although few papers reported its conversion to tumoral cells. This re
svie
archw describes the role of si-RNA for NP CXCR4-MSC as an antitumoral drug.
Does Transplanted Mesenchymal Stem Cells (MSC) Exert Antitumoral or Favor Tumorigenesis?
MSC releases several paracrine factors involved in proliferation or repair (i.e., bFGF fibroblast growth factor), Platelet growth factor (PDGF), neurotrophic factor (NTF), GDNF (glial neurotrophic factor), BDNF: brain-derived neurotrophic factor), endothelial growth factor (VEGF), HGF (hepatocyte growth factor), Insulin Growth factor (IGF-1)
[14][15][7,35]. For example, secreted factors by fat-derived mesenchymal stromal cells (MSC-ADSC) protect chondrocytes in rodents of osteoarthritis by increasing HFG, and these MSCs also promoted immunomodulatory effects
[16][36] and converted pro-inflammatory M1 monocytes into an anti-inflammatory M2 state
[17][37];
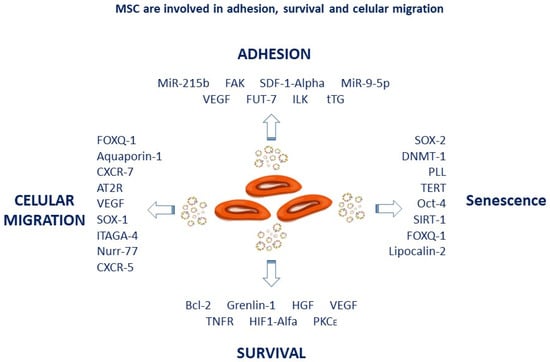
Figure 1 summarizes the effect/s of MSC on cell adhesion, migration and proliferation markers.
Figure 1. Trophic factors released by MSCs contribute to cell adhesion, migration, survival, and senescence. For example, CXCR4 or CXCR5 chemokines increase MSC mobilization, while trophic factors such as HGF VGEF play a role in survival.
The immunoregulatory activity of MSCs is mediated through secreted cytokines by antigen-presenting cells (IFN γ, IL-1α, IL-1β, and TNF-α)
[18][38] and several factors (IDO, TSG6, NO, IL-10, CCL2, galectins, PGE2 or TGF-β)
[19][20][21][39,40,41]. The activation of MSCs by Tumor necrosis factor α (TNF-α), IL-1β, nitric oxide (NO), liver growth factor (HGF), and VEGF promoted immunomodulatory effects in MSC
[22][42], see
Figure 1.
The few studies that detected protumor effects of MSC, in general, are explained by the transformation of these MSCs into cancer cells
[23][24][43,44]. Several factors like SDF-1 alpha (as occurs in gynecological tumors), HDGF (hepatoma-derived growth factor), VEGF, bFGF, or MCP-1 (monocyte chemotactic protein-1) are also involved in the proliferation of different cell types. These released factors by MSCs enhances the migration toward the tumor site in a CXCR4/SDF-1 dependent manner
[25][45]; in addition, the angiogenesis by VEGF increases the proliferation of tumor cells by forming new blood vessels. In this case, MSCs can enhance tumor proliferation, inducing metastasis by the conversion of MSCs into tumoral cells
[26][27][46,47]. For example, bone marrow-derived MSCs can progress to gastrointestinal epithelial cancer by
Helicobacter hepaticus infection in mice
[23][24][43,44].
MSCs exert antitumoral effects by regulating cell cycle proteins, reducing angiogenesis, promoting apoptosis of cancerous cells as well as immunomodulatory effects
[28][29][30][31][32][33][34][35][48,49,50,51,52,53,54,55]. In fact, when MSCs are co-transplanted in a glioblastoma rodent model of cancer, both angiogenesis and tumor progression are abolished in different types of cancers (e.g., from colorectal to hematological type)
[36][56].
To date, clinical studies have reported the safety of MSCs without tumor formation in patients. In a meta-analysis of 36 studies, including eight randomized trials with adequate control, the absence of tumors has been demonstrated after MSC transplantation (n = 1012 patients
[37][57]. In this way, the immunological status of MSC-transplanted animals with NP with different nanocarriers becomes relevant
[38][58]. For example, bone marrow-derived MSCs (BM-MSCs) can spontaneously transform into malignant fibrosarcoma after systemic administration to immunocompromised mice. However, the long-term MSC transplantation did not show tumors in tissues
[38][58]. Fibrosarcoma formation was detected after transplanting MSCs in immunocompetent mice with spontaneous p53 mutations
[39][59]. Two further studies conducted with stem cells observed malignant transformations of MSC cells in
Cynomolgus macaques [40][41][60,61]. These chromosomal aberrations seem to be associated with cellular senescence
[42][43][62,63]. In any case, the possibility of rare tumorigenic transformations should not be ignored and cytogenic aberrations should be tested in cases of long-term MSC transplantation
[44][64].
2. Mesenchymal Stem CellSC as Vehicles for Drug Delivery against Tumoral Cells
The International Organization for Standardization (ISO) textually defines a nanomaterial as a “material with any external dimension in the nanoscale or having an internal structure or surface structure in the nanoscale (1–100 nm)”. The European Commission adopted a definition for a nanomaterial (2011) as follows: “A natural, incidental or manufactured material containing particles, in an unbound state or as an aggregate or as an agglomerate and where, for 50% or more of the particles in the number size distribution, one or more external dimensions is in size range 1–100 nm”. The United States Food and Drug administration (US FDA) states that nanomaterials are “materials up to one micron if these ones exhibit properties or phenomena that are attributable to its dimensions”. In this re
svie
archw, a size range between 1–1000 nm is considered for nanomaterials and nanoparticles (NPs)
[45][46][65,66]. Metallic nanoparticles, with a dimension of 1–100 nm, were first described by Faraday M (1987) in an aqueous solution when he recognized the formation of ruby colored-AuNPs after a reaction of gold salt
[45][65]. NPs can be used in several biomedical applications because of their unique physicochemical properties (high ratio of surface area to volume, surface plasmon resonance (SPR), presence of edges and corners, and electron storage capacity, among others
[47][48][67,68]. NPs have several sized and shapes and can be prepared with different chemical, physical, and biological methods
[49][69]. For example, gold (Au), copper (Cu), Silver (Ag) are pure metals metallic NPs, while cerium oxide NPs (nanoceria), Silicate NPs (SiNPs), zinc oxide (ZnO), titanium oxide (TiO
2), and iron oxide NPs (SPIONs) are metal oxide. Accordingly, scientists have attempted to use stabilizing agents, such as polyacrylic acid, polyvinylpyrrolidone, and polyvinyl alcohol, which are adsorbed onto the surface of particles; as a consequence, the minimized particle aggregation takes place and form a stable solution of the metallic NPs
[50][70]. The tiny size of nanomaterials allows efficient interaction with the cell surface of cell components, including stem cells
[51][71]. Drug delivery, diagnostics, imaging, cancer therapy, anti-microbial, and antiangiogenic are several biomedical applications of NP that would allow better therapeutic use of metallic NPs in the field of regenerative medicine. The Impact of metallic nanoparticles on stem cell proliferation and differentiation has been revised under different pathological conditions
[52][72]. Collectively, particles with tailored physicochemical properties can exert differential influence on stem cell differentiation and signaling pathways, which regulate stem cell differentiation and proliferation by regulating inflammation and oxidative stress
[52][53][72,73]. As an example, silica-coated magnetic nanoparticles (NP) decreased the migratory capacity of human bone marrow-derived mesenchymal stem cell (hBM-MSC) by reducing membrane fluidity and also affects levels of proteins involved in focal adhesion
[54][74]. In addition, biophysical properties can alter nanomaterials effects on stem cells and reduce the membrane fluidity or reduce 10%or more the viability of hBM-MSCs labeled with silica-coated magnetic NPs (stained with rhodamine B isothiocyanate); MNPs-SiO increased the oxidative stress in hBM-MSCs as compare to controls. The major mechanism underlying nanoparticle-induced cell shrinkage and abnormal formation of focal adhesions involved cytoskeletal depolymerization
[53][73]. However, in this study, MNPsSiO
2 (RITC)-induced lipid oxidation in a concentration-dependent manner without specific interaction with cytoskeletal proteins. Thus, the migratory capacity of hBM-MSCs is impaired by MNPs-SiO
2 (RITC)
[53][73].
It is known that passive transport and endocytosis are two key processes required for the reuptake of NP by cells in general, including MSC
[45][65]. The NP’s physicochemical properties (e.g., size, shape, and stiffness and surface charge), biocompatibility and bioaccumulation, colloidal stability, degradation rate, e.g., solubility as well as the route of administration (e.g., intravenous, oral, intranasal, dermal) are cue factors neccesary for a final good penetrance within the tumor location
[54][74]. These factors can influence the cell–NP interactions and subsequent uptake. The principal parameters to take into consideration for NP physicochemical properties on endocytic mechanisms are revised by several authors
[53][54][55][73,74,75].
The interaction between different NPs and cells depends not only on the shape of the NPs but also on the cell type. The particle size and shape influence the biological function and the NP internalization into the cells; Additionally, other factors such as stiffness, the hydrophilic or hydrophobic properties are important for NP-stem cell interactions
[51][71]. In fact, the uptake of NPs is inversely correlated with the particle sizes; in fact, the higher uptake of smaller size NPs (30–50 nm) was reported, compared to bigger size NPs (50–200 nm) with less cellular internalization
[56][57][76,77]. The interaction between different NPs and cells depends on the shape of the NPs and the type of cell. Shape can increase or decrease uptake of NPs because the sphero-cylinders are more efficiently endocytosed compared to spheres of the same diameter. The membrane curvature, less available receptor binding sites, and surfactant molecules could also explain the lack of multivalent binding to the receptors
[58][59][78,79]. In this way, spherical-shaped NPs showed higher uptake rate than non-spherical NPs
[59][60][79,80]. The chemical modification of NPs by increasing the softness and the hydrophobicity increases the rate of internalization
[61][81]. In addition, a particle surface charge has been associated with differential cellular internalization since a positive charge can quickly enter the nucleus and avoid the lysosomal degradation of NP; conversely, those particles with neutral or negative charges access into the lysosomes instead of at the perinuclear region
[62][63][82,83]. As an example, the anti-microbial activity of TiO
2 NPs was elevated when combined with gold Au/TiO
2 nanocomposite by alteration in the surface charge of TiO
2 NPs when were conjugated with gold
[64][84]. Finally, the potential interference of food supplements could affect the NP uptake capacity
[54][65][74,85]. As an example,
rwe
searchers highlight the endocytosis and cytotoxicity of zinc oxide (ZnO) NPs and vitamin C co-exposure affect the uptake of NP by neural stem cells
[66][86].
The ability to carry drugs is enhanced when MSC cells are exposed to nanoparticles (NP)
[67][8]. Several studies demonstrated that certain drugs could be internalized by caveolins or clathrin receptors in MSC (present on the cell membrane); caveolins are essential proteins that form invaginations of the cell membrane and also play a role in intracellular transport. Drugs can also be internalized by pinocytosis or macropinocytosis
[68][87].
On the other hand, intracellular degradation of NPs often takes place in the lysosomes following the endocytosis pathway. The degradation process is affected by the acid pH in the endolysosomes (close to pH 4.5); these lysosomes strong proteolytic activity regulates redox signaling mechanisms by glutathione and metallothioneins; thus, this environment favors the dissolution of several metallic NPs (iron oxides, ZnO, CuO, Ag, and AuNP); The pace of NP degradation within the cells showed similarities between the cell responses to metallic NPs and ionic forms
[54][74]. The Aurosome formation illustrates that ions and NPs of the same metal seems to been processed by cells in the same manner. For example, Au ions and NPs have a common intracellular fate in aurosomes, and their internalization and location in lysosomes appear quickly after exposure to ionic Au but within days to months after exposure to Au NPs
[54][74].
The modification of the particle surface by the addition of functional group can modulate its cellular uptake and could induce toxicity in the cells by TiO
2 nanorods functionalized with various functional groups, such as carboxyl groups (–COOH), poly (ethylene glycol) (–PEG), and amines (–NH
2), which showed a variation in their uptake by rat bone marrow-derived MSCs (rBM-MSCs)
[55][69][70][75,88,89]. In fact, TiO
2–NH
2 nanorods and the core nanorods showed the highest rate of cellular internalization compared with TiO
2–COOH and TiO
2–PEG nanorods with lower uptake. However, the TiO
2 core nanorods are toxic and increase reactive oxygen production
[65][70][85,89]. Another study has demonstrated that delivery of methotrexate, (anti-cancer drug), was conducted by binding on the carboxyl group with the surface of AuNP
[70][89]. On the other hand, the anti-microbial activity of TiO
2 NPs increased when they were combined with gold (Au/TiO
2 nanocomposite)
[64][84]. Thus, the application of metallic NPs allows drug delivery for cancer therapy
[66][71][86,90].
To prepare efficient magnetic nucleic acid carriers, it is necessary to improve the endocytosis efficiency of PEGylated magnetic nanoparticles. For example, heptafluorobutyryl-polyethylene glycol-polyethyleneimine (FPP) are used to coat magnetic nanoparticles (MNPs) to obtain magnetic nanocarriers FPP-MNPs. The fluorinated cationic polymer-coated magnetic nanoparticles FPP-MNPs can be loaded with siRNA
[72][73][91,92]. The NP used in the core can be designed for future applications (e.g., anti-cancer drug delivery). These membrane-coated NPs have been shown to preferentially accumulate at tumor sites
[74][4]. Via these mechanisms, MSCs could carry antitumor drugs to localized sites of the tumor
[75][5]. In addition, the use of natural polymers, which can be “packaged” on the surface of MSCs, enhances their drug delivery
[51][71]. For example, supermagnetic iron oxide nanoparticles (SPIONs: a type of iron oxide NPs: SPIONs) possess superparamagnetism property when are subjected to an external magnetic field
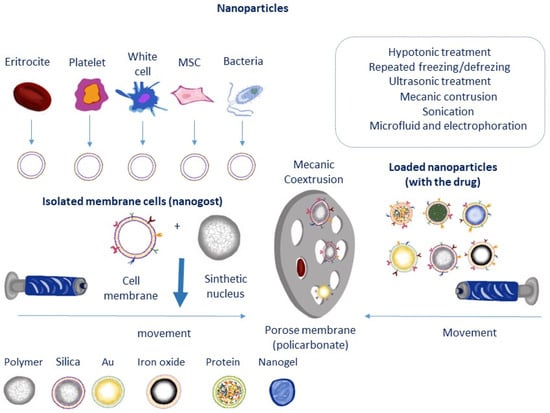
, see Figure 2)
[52][76][77][78][72,93,94,95]. SPIONs nanoparticles are considered as being a safe nanomaterial for stem cell labelling. For example, coating SPIONs Superparamagnetic iron oxide NPs with dextran (DEX) and then labeling stem cells promoted myogenic differentiation under a pulsed electromagnetic field (MyoG and Myh2 marker)
[79][96]. However, the special physicochemical properties of SPIONs induced cytotoxicity by affecting cellular components (DNA, nucleus, and mitochondria)
[80][97]. The surface chemistry alteration of SPIONs by citrate significantly hampered osteogenic differentiation of MSCs and also decreased the expression of induced osteogenic differentiation-related genes
[70][89]. Conversely, high concentration of SPIONs (Ferucarbotran: 300 µg/mL) abrogated the osteogenic differentiation and enhanced the cell migration of MSC, which was mediated via the activation of β-catenin, and also matrix metalloproteinase 2 (MMP2) signaling pathways. Therefore, free iron is implicated in SPION-induced inhibition of the osteogenic differentiation of hMSCs
[81][98]. Conversely, SPIONs (Feridex)-labeled hBM-MSCs did not affect the osteogenic or adipogenic differentiations, although they suppressed the chondrogenic differentiation
[82][99].
Figure 2. Nanoparticle technology and physical methods for the introduction of several carriers in different types of cells (MSC, eritrocytes, etc…). Adapted from [87].
On the other hand, external stimuli such as magnetic fields can influence the high rate of particle internalization into stem cells
[77][94]. In this way, the magnetic field-induced assembly (stripe-like) of magnetic SPIONs was exploited for the conversion of primary mouse bone marrow cells into osteoblasts
[83][100]. The interface between SPION magnetic assemblies and the cells promote osteogenic differentiation rather than the particles internalization into the human bone marrow stem cells (BM-MSCs)
[84][101]. In addition, SPIONs induced hMSCs proliferation by regulating cell cycle-related proteins under oxidative stress
[85][102]. As an example, SPION-induced gap junction communication between cardiomyoblasts while MSCs protected against myocardium infarct in mice
[86][103].
Rafieepour et al. reported toxicological effects of Fe
3O
4 and SiO
2 single and combined exposure of magnetite (Fe
3O
4) in cells were exposed to different NP concentrations (10, 50, 100, and 250 mg/mL), which were simultaneously for 24 h and 72 h. In contrast, the effect of combined exposure to Fe
3O
4 and SiO
2 NPs is less toxic by the accumulation of intracellular proteins, forming a protein corona. In addition, Fe
3O
4 could induce the synthesis of cellular proteins, forming a protein corona on the surface of silica NPs and thereby reducing its cytotoxicity
[87][104]. Thus, the formation of a corona can reduce cellular uptake of functionalized NPs by shielding the ligands from binding to their receptors, which prevent the recognition by transferrin receptors. Consequently, the composition of a protein corona is an important determinant of NPs fate and their cellular internalization
[88][105]. However, the corona composition varies depending on the nature of the biological fluids in which NPs are dispersed
[89][106]. The preparation of engineered NPs with the desired functional group is a tool for biomedical applications
[90][91][107,108]. The internalization rate of polystyrene NPs and polystyrene NPs functionalized with an amine group in MSCs was studied in vitro
[92][109]. Amino-functionalized polystyrene NPs showed faster internalization and higher cellular uptake in comparison to unfunctionalized polystyrene NPs. For example, TiO
2 NPs are toxic for MSCs in a size-dependent manner by reducing cell migration, promoting a lack of cell membrane integrity, and suppressing osteogenic differentiation
[93][110]. TiO
2 nanotubes larger than 50 nm showed a drastically decrease in the proliferation and differentiation of MSCs
[94][111]. In addition, TiO
2–COOH nanorods abolished the osteogenic differentiation of rat BM-MSCs
[70][89].
Collectively, particles with tailored physicochemical properties can exert differential influence on stem cell differentiation and affect its proliferation. Interestingly, the stem cell differentiation capacity is influenced by ROS production
[52][94][72,111].
On the other hand, MSCs can interact with two different classes of nanoparticles (NP), either those containing polylactic acid or lipid nanocapsules. In addition, covalent, hydrophobic, or electrostatic interactions on the surface of MSCs enhance the drug-carrying capacity
[95][96][112,113]. For example, glycolic acid polyconjugates enhance nanoparticle drug delivery in human MSCs
[97][114]. In addition, covalent, hydrophobic, or electrostatic interactions on the surface of MSCs also increase their drug-carrying capacity
[97][114]. For example, glycolic acid polyconjugates enhance nanoparticle drug delivery in human MSCs
[97][114] while coating PLGA-type nanoparticles with the macrophage membrane promotes anti-angiogenesis effects
[98][115]. PLGA nanoparticles can be loaded with saikosaponin D, a compound with potential therapeutic properties against cancer; the use of red blood cells as biomimetic membranes guarantee a prolonged blood circulation time of the NPs. In addition, enzymatically active methods as the use of catalase on the erythrocyte membrane
[99][116] could metabolize endogenous hydrogen peroxide from the tumor as a strategy for tumor eradication
[100][117]; thus, the cell membrane-engineered NPs effectively inhibited tumor growth (e.g., breast cancer metastasis in vitro and in vivo) by blocking angiogenesis (a process involved in tumor dissemination). In turn, labeling with fluorescent particles (such as coumarin-6 dye) allows the identification of tumor cells in tissues by fluorescence emission
[101][118]. Another study reported that carbon nanoparticles can reduce the viability of human MSC cells
[53][102][73,119].
From this perspective, nanotechnology facilitates the migration and distribution of MSCs within tissue with high sensitivity and resolution
[102][103][104][105][106][107][108][119,120,121,122,123,124,125]. Paclitaxel-loaded polymeric NPs (anticancer drug) as drug delivery system significantly inhibits tumor growth and also suppresses lung metastasis. Platelet membranes as nanocarriers can be co-loaded with tungsten oxide nanoparticles (W18O49) and metformin (PM-W18O49-Met NP) to treat lymphomas; in fact, PM-W18O49-Met significantly inhibited tumor growth by inducing apoptosis of lymphoma tumors in vitro and in vivo. In this study, metformin reduced tumor oxygen consumption and enhanced the therapeutic effects of W18O49
[104][121]. For example, gold nanoparticles can induce their differentiation into osteocytes, a property attributable to such gold nanoparticles
[108][125]. Gold nanoparticles loaded with the IR775c label facilitate the monitoring and distribution of MSC cells ¨in vivo¨ by fluorescent particles (such as coumarin-6 dye) in tumor cells with high sensitivity and resolution
[101][103][104][109][118,120,121,126]. Interestingly, gold nanoparticles can induce their differentiation into osteocytes, a property attributable to such gold nanoparticles
[108][125]. Conversely, carbon nanoparticles can reduce the viability of human MSC cells
[74][4]. Figure 2 shows the most representative cell types and coated used in nanothecnology.
On the other hand, transfection consists of the introduction of foreign genetic material into eukaryotic cells by plasmids, allowing the passage of genetic material (such as supercoiled DNA constructs or siRNA) by electroporation. Additionally, the use of liposomes with mixed lipids allows its fusion with the cell plasma membrane and also enhance its deposition inside the cell
[102][119]. The negative charge on the surface of MSCs and the hydrophobicity allow the drug anchorage
[51][71]. The “anchoring” occurs successfully with silica NPs to the surface of MSCs by specific recognition molecules against cancer cells. In this way, the expression of CD73 and CD90 antibodies on the cell membrane of MSC contributes to the specific binding of silica NPs, ensures a high circulation for long periods, and increases the homing toward the tumor localization
[106][107][123,124].
2.1. Interaction between Nanoparticles (NP) and Stem Cells
The preparation of NPs, along with their physicochemical properties, affects the biological function of MSC. Several mechanisms are involved in metallic NP-induced cellular proliferation and differentiation while oxidate reactive species and inflammatory mediators as well as the regulation of several transcription factors are factors that affects the differentiation of MSC in several cell types
[52][72].
The silica-coated magnetic NP decreased human hBM-MSC migratory capacity by reducing membrane fluidity and also impairs the expression of focal adhesion molecules
[53][73]. Regarding stem cell differentiation, previous studies have demonstrated positive and negative impacts of AgNPs on stem cell differentiation. As an example, AgNPs of size 10 or 20 and 30 nm are not toxic for MSCs cells but did not affect the differentiation. The shape, size, and surface characteristics of AuNPs impacted their potential to induce the osteogenic differentiation of MSCs. In human adipose-derived stem cells (hADSCs), the induction of osteogenic differentiation is prompted by AuNPs (sized 30 and 50 nm). In addition, gelatin hydrogels loaded with AuNPs increased the proliferation and osteogenic differentiation of hAD-MSCs. In human hBM-MSCs and MC3T3-E1 cells, miR029b-delivered polyethyleneimine (PEI)-capped AuNPs efficiently promoted the osteogenic differentiation without significant toxicity; In addition, L(D)-PAV-AuNPs-exposed MSCs showed upregulation of osteogenic differentiation marker genes; in another study the small size of AuNPs (4 nm) affects the differentiation of hBM-MSCs compared with large size AuNPs (40 nm). The small AuNPs markedly suppressed osteogenic differentiation and induced the adipogenic differentiation of hBM-MSCs. Collectively, the differentiation of stem cells in small size AuNP-treated hBM-MSC is influenced by oxidative stress and inflammation. Interestingly, AuNP-loaded functionalized nanofibrous scaffold promoted the cardiogenic differentiation of the MSCs by upregulating cardiogenic differentiation-related markers
[52][72]. The affinity of MSCs with metallic nanoparticles and polymeric nanoparticles has been studied in cite
[107][124]Clathrin or caveolin-dependent endocytosis is considered to be the main mechanism for the uptake of nano-size materials. Clathrin and caveolin-dependent endocytosis, phagocytosis, macropinocytosis, and pinocytosis represent mechanisms for the cellular internalization of NPs. The exocytosis or release of NPs is carried out via vesicle-dependent release, non-vesicle-dependent release, and lysosomal secretion. The treatment with several inhibitors (nocodazole, lovastatin, chlorpromazine, and cytochalasin A) could affect the cellular uptake in vitro and are tools for the study of NP cellular internalization
[110][111][112][113][114][115][116][127,128,129,130,131,132,133].
The interaction of the nanomaterials with the cell membrane or intracellular components, as well as signaling pathways by internalized NPs, were reported in vitro
[111][116][128,133]. The conjugation of polyethylene glycol to the surface of NPs is one of the key tools for surface modifications of the carriers (see
Table 1 and Figure 2). As an example, the AuNP represents a model metallic NP with high efficiency for delivering nucleic acids, recombinant proteins, and drug compounds to the tumor
[117][134]. As an anti-cancer strategy, the delivery of methotrexate, a well-known anti-cancer drug, was conducted by the binding of its carboxyl group with the surface of AuNP
[70][89]. For additional details on the possible application of noble metallic NPs in drug delivery for cancer therapy consult cyte
[52][118][72,135]. These treatments with AgNPs of 10, 20 and 30 nm size are not toxic for MSCs and as coating material, could increase the adipogenic differentiation of hBM-MSCs and induce the osteogenic differentiation of urine-derived stem cells
[111][112][113][114][115][116][117][128,129,130,131,132,133,134].
shows brief information on the size of different NPs [124]).
Table 2. Nanoscale unit, major compound, and shape/size.
2.2. Agents for MSC Vehicles
Table 2