Pancreatic cancer (PDAC) is one of the most aggressive solid tumors and is showing increasing incidence. Here provide practical help for all clinical oncologists and to summarize the current management of PDAC using a simple “ABC method” (A—anatomical resectability, B—biological resectability and C—clinical conditions). For anatomically resectable PDAC without any high-risk factors (biological or conditional), the actual standard of care is represented by surgery followed by adjuvant chemotherapy. The remaining PDAC patients should all be treated with initial systemic therapy, though the intent for each is different: for borderline resectable patients, the intent is neoadjuvant; for locally advanced patients, the intent is conversion; and for metastatic PDAC patients, the intent remains just palliative.
- pancreatic cancer
- therapy
- prognosis
1. Introduction
2. Resectable PDAC and Simple “ABC Method”
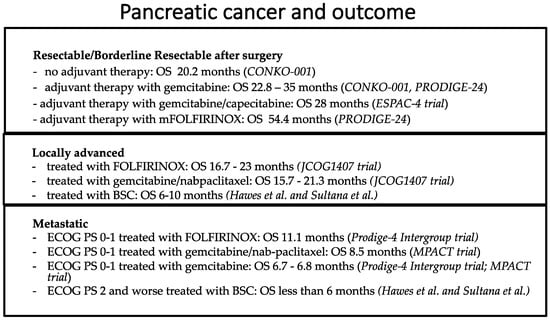
Surgical resection is the only potentially curative treatment for pancreatic cancer. Unfortunately, only a minority of PDAC patients (approximately 15–20%) are judged to be technically eligible for potentially radical resection at the time of initial diagnosis. Anatomical resectability can be determined according to different international guidelines. The most used international classifications are MD Anderson Cancer Center, AHPBA/SSO/SSAT, NCCN and Alliance [17][18][19][20][17,18,19,20]. Generally, resectable PDAC is defined as the absence of arterial and venous contact. Regarding arterial involvement, an exact description of the common hepatic arteries, celiac axis or superior mesenteric artery is necessary, and for venous involvement, the portal and superior mesenteric vein are of particular interest to pancreatic surgeons. It needs to be specified that NCCN and Alliance guidelines consider venous contact (without arterial involvement) <180° as anatomically resectable PDAC if there is no deformity or stenosis of the portal and superior mesenteric vein [17][18][19][20][17,18,19,20]. The major aim of surgery is its radicality in terms of R0 margin achievement. R0 margins are characterized by a distance >1 mm between tumor cells and margins. The type of surgery depends on the primary tumor location: the recommended surgery in the case of pancreatic head tumors is pancreatoduodenectomy, also known as the Whipple procedure. In the case of cancer of the body and tail, distal pancreatectomy with splenectomy should be performed. As for the other gastrointestinal solid tumors, a minimum number of lymph nodes should be removed during surgery; for PDAC, a minimum of 15 lymph nodes is recommended. Another important point in PDAC diagnostics and treatment workup is biopsy. If upfront resection is planned, no histological characterization is necessary in the case of radically resectable pancreatic tumors without high-risk features, with typical radiological and clinical imaging. In the presence of jaundice, preoperative biliary stenting is not necessary in order to normalize blood levels of bilirubin, and upfront surgical resection should be recommended. This is to avoid complications associated with biliary drainage that may delay the surgery. Only when jaundice is associated with cholangitis or bilirubin > 25 mol/L is preoperative biliary stenting considered [21]. High-volume centers for pancreatic surgery are recommended as these procedures are burdened by the high rates of mortality and morbidity. It is very important to pay attention to possible postoperative complications, such as steatorrhea, where, for pancreatic enzymes, a prescription might be indicated (see also the next chapter on pancreatic exocrine insufficiency). Moreover, glucose blood levels should be monitored and adequate treatment for diabetes should be prescribed. Finally, splenectomy renders the patients more vulnerable to infectious complications; therefore, vaccinations, such as meningococcus and pneumococcus, should be performed. Unfortunately, even if radical surgery is possible with R0 margins, the rate of recurrence for pancreatic cancer patients is very high, particularly during the first 2 years. The prevalent way of disease recurrence is systemic with distant metastases, suggesting that patients might hide micro-metastatic disease [2][22][2,22]. In order to reduce the risk of high recurrence, adjuvant chemotherapy should be offered to all PDAC patients who undergo pancreatic surgery for cancer. For fit patients, an adjuvant three-drug chemotherapy regimen with modified FOLFIRINOX (fluorouracil, irinotecan, leucovorin, and oxaliplatin) represents the actual standard of care in this setting. This regimen showed a significant improvement in median overall survival (OS) compared to gemcitabine monotherapy (OS 54.4 vs. 35 months, HR 0.64; p = 0.003) [23]. Gemcitabine plus capecitabine or gemcitabine alone are alternatives for patients with contraindications to FOLFIRINOX, such as patients over 75 years old, with poor performance status or postoperative complications [24][25][26][27][24,25,26,27]. The median OS for PDAC patients treated after potentially radical pancreatic surgery with gemcitabine plus capecitabine was 28.0 months compared with 25.5 months in the gemcitabine group (HR 0.82; p = 0.032) [25]. Adjuvant chemotherapy with gemcitabine in monotherapy showed better efficacy in terms of longer DFS (13.4 vs. 6.9 months in the control arm; p < 0.001), though no statistically significant difference in OS was seen (22.1 vs. 20.2 months in the control arm; p = 0.06) [26]. Interestingly, in the subgroup analysis, only PDAC patients with negative lymph nodes on the final histological report had statistically significant benefits in terms of OS from adjuvant gemcitabine treatment (34 vs. 27.6 months; p = 0.04) [26]. Adjuvant chemotherapy should generally start within 12 weeks from surgical resection, even though evidence suggests that the completion of adjuvant treatment, rather than its timing, is important to achieve an OS benefit [28][29][28,29]. On the contrary, adjuvant chemoradiotherapy is not currently indicated and should not be performed outside of clinical trials [30]. The clinical evidence for neoadjuvant treatment use for anatomically resectable PDAC is mostly based on the long-term results of the PREOPANC trial and a meta-analysis of randomized controlled clinical trials, in which both resectable and borderline resectable PDAC patients were evaluated [31][32][31,32]. Therefore, neoadjuvant approaches in clearly resectable PDAC without high-risk factors are still contradictory, and the results of phase III trials are awaited (PREOPANC3 and ALLIANCE A021806) [33][34][33,34]. Through the years, the definition of resectable PDAC has been updated to achieve a more uniform definition, and in addition to “anatomic considerations”, “biological” and “conditional”, factors are now being considered to define pancreatic cancer to be resectable or borderline resectable (“ABC method”) [35]. Therefore, even patients with anatomically resectable PDAC should be evaluated for the presence of high-risk biological and conditional features. High-risk biological features include suspicious hepatic or pulmonary lesions, the presence of positive lymph nodes (histologically proven or based on the positivity of a PET-FDG scan), large pancreatic primary tumors with dimensions superior to 2–3 cm, elevated baseline levels of the tumor biomarker CA 19-9 and several clinical characteristics, such as celiac-type pain or significant weight loss (≥10% of body weight) [16][35][16,35]. In fact, increased baseline serum levels of CA 19-9 (especially ≥500 UI/mL) inversely correlate with resectability as well as with survival rates [36]. Similarly, the existence of positive lymph nodes strongly impacts the prognosis of PDAC patients regardless of tumor resectability or tumor stage [37]. The high-risk conditional factors include performance status and co-morbidities that increase the risk of morbidity or mortality after surgery. Given the higher probability of non-radical resection, patients with resectable tumors and high-risk factors are not considered optimal candidates for upfront surgery and should, therefore, receive neoadjuvant chemotherapy (Figure 1). Neoadjuvant chemotherapy includes several advantages, such as the early treatment of micrometastatic disease, the downstaging of disease and an increased likelihood of an R0 resection, and is associated with increased OS rates; in addition, it does not negatively affect major surgical complications rates. Before neoadjuvant treatment initiation, a biopsy for PDAC confirmation is mandatory. According to the SWOG S1505 trial, which compared a neoadjuvant chemotherapy three-drug regimen with modified FOLFIRINOX and a neoadjuvant two-drug regimen with gemcitabine/nab-paclitaxel in patients with anatomically resectable pancreatic cancer, no statistically significant difference in overall survival was seen between the two treatment arms, though the gemcitabine/nab-paclitaxel regimen showed a higher rate of complete and major pathologic response (42% vs. 25% in the mFOLFIRINOX arm) [38]. The optimal duration of neoadjuvant treatment is unknown. There is a general consensus that 6 months of nonsurgical therapy is optimal; therefore, adjuvant chemotherapy can be administered continuing the preoperative regimen for a total of 6 months.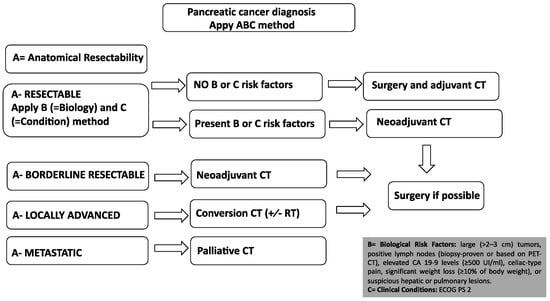
3. Borderline Resectable and Locally Advanced PDAC
Borderline resectable pancreatic adenocarcinomas (BRPCs) are a subgroup of technically resectable pancreatic cancer but at high risk of non-radical resection (R1) and/or early recurrence after surgery (anatomically resectable PDAC with high-risk biological or conditional factors). Locally advanced pancreatic adenocarcinomas (LAPCs) are tumors with local infiltration that preclude potentially radical pancreatic surgery with R0 margins. Both BRPC and LAPC should, therefore, be treated with initial systemic chemotherapy treatment using the same regimens used in a metastatic setting (FOLFIRINOX or gemcitabine/nab-paclitaxel; see Figure 1) [39][40][39,40]. According to a recent meta-analysis of non-randomized patient cohorts, in patients with BRPC or LAPC, primary treatment with FOLFIRINOX compared with gemcitabine-based chemotherapy appears to provide a survival benefit for patients that are ultimately unresectable [41]. For patients who undergo surgical resection, outcomes are similar between gemcitabine-based chemotherapy and FOLFIRINOX when delivered in a neoadjuvant setting [41]. When the tumor is not resectable after induction chemotherapy, chemoradiotherapy might be considered, even if several randomized studies did not demonstrate any survival benefit and its role remains controversial [42][43][42,43]. Less than 30% of LAPC will undergo surgery after “conversion therapy” [43][44][43,44], and one-third of PDAC patients die from local progression without distant metastases. Finally, chemoradiotherapy can be useful as a symptomatic treatment of LAPC-related pain [16][45][16,45].4. Metastatic PDAC
4.1. First-Line Therapy
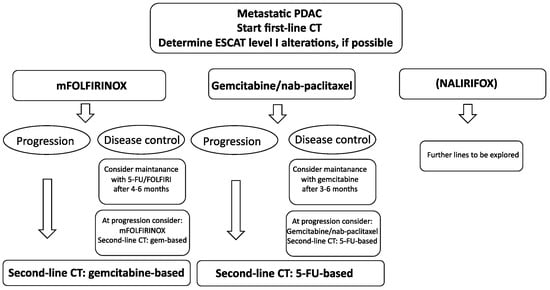
According to phase III clinical trials, FOLFIRINOX or gemcitabine/nab-paclitaxel are the two regimens for fit PDAC metastatic patients [39][40][39,40]. FOLFIRINOX is a three-drug regimen that showed better survival outcomes compared to gemcitabine monotherapy with an OS of 11.1 vs. 6.8 months, respectively, and is recommended for metastatic PDAC patients with good clinical conditions (ECOG PS 0–1) and younger ages (less than 75 years). The median PFS was 6.4 months in the FOLFIRINOX group and 3.3 months in the gemcitabine group. Progressive disease was described in 15.2% in the FOLFIRINOX group and 34.5% in the gemcitabine group [39]. Importantly, according to a meta-analysis that evaluated 1461 metastatic PDAC patients, no difference in mOS, mPFS, and ORR between the standard FOLFIRINOX regimen utilized in the PRODIGE4 study and the modified FOLFIRINOX regimens was seen. Modified FOLFIRINOX differs from “classical” FOLFIRINOX in the omission of the 5-FU bolus and/or dose reductions in infusional 5-FU, irinotecan, and/or oxaliplatin, with consequent less collateral side effects and better tolerance. Based on these studies, modified FOLFIRINOX regimens have been adopted in clinical practice for first-line palliative settings [46]. Gemcitabine and nab-paclitaxel represent an alternative regimen for metastatic PDAC patients, as OS in the gemcitabine–abraxane group improved with statistical significance compared to gemcitabine monotherapy (8.5 vs. 6.7 months, p < 0.001). The median PFS was 5.5 months in the gemcitabine and nab-paclitaxel group and 3.7 months in the gemcitabine group. Progressive disease was described in 20% in the gemcitabine and nab-paclitaxel group and 26% in the gemcitabine group [40][47][40,47]. There are no prospective randomized trials with a head-to-head comparison between the two regimens (FOLFIRINOX vs. gemcitabine/nab-paclitaxel), though analyses of non-randomized “real world” studies to date have not provided evidence of a major benefit of one regimen over the other; therefore, there is no clear preference [48]. Recent studies have suggested that basal-like PDAC characterized by low GATA-6 tissue expression is less sensitive to platinum-based chemotherapy (including FOLFIRINOX) than the classical type [49][50][49,50]. Single-agent gemcitabine can be given to patients with poorer performance status to provide clinical benefit [51]. Clinical benefit response is experienced by 23.8% of gemcitabine-treated patients compared with 4.8% of 5-FU-treated patients. The median survival durations were 5.6 and 4.4 months for gemcitabine-treated and 5-FU-treated patients, respectively. The survival rates at 12 months were 18% for gemcitabine patients and 2% for 5-FU patients [51]. A PS of 3 or 4, however, contraindicates any palliative chemotherapy and only allows the best supportive care. Therefore, PDAC patients who are capable of only limited selfcare, confined to a bed or chair more than 50% of waking hours, should not undergo any active anticancer treatment. Recently, at the ASCO 2023 conference, the results of phase III NAPOLI-3 were shown.4.2. The Role of Maintenance after First-Line Therapy
There are limited data to recommend the management of patients with locally advanced or metastatic pancreatic cancer who achieved disease control or reduction after first-line palliative treatment. In this setting, maintenance therapy represents an important tool in order to minimize chemotherapy toxicity while preserving survival benefits [52][53]. The only drug approved for maintenance therapy in metastatic PDAC, with germline BRCA mutation, is Olaparib [53][54], though it is not available in all countries due to regulatory restrictions. Generally, after FOLFIRINOX, maintenance with 5-FU/capecitabine or FOLFIRI might be considered. 5-FU monotherapy maintenance appeared to be as effective as FOLFIRI, in a FOLFIRINOX de-escalation maintenance strategy; therefore, 5-FU maintenance might be considered an option after 4 months of FOLFIRINOX chemotherapy with no progressive disease [54][55][55,56]. After gemcitabine and nab-paclitaxel, maintenance with gemcitabine might be considered [56][57]. The optimal maintenance strategy, however, is not defined.5. Second-Line Therapy
Around half of metastatic PDAC patients are eligible for second-line chemotherapy [57][58]. Currently, there is no standard second-line treatment. Generally, after progression on FOLFIRINOX, treatment with gemcitabine, as well as gemcitabine and nab-paclitaxel, is a reasonable option, when feasible considering the regulatory issues in different countries [58][59][60][59,60,61]. After progression on first-line gemcitabine-based chemotherapy regimens, several treatment possibilities with 5-FU-based combinations are available, including liposomal irinotecan plus 5-FU/leucovorin combinations, FOLFIRI, mFOLFIRINOX, FOLFOX, XELOX, OFF (oxaliplatin, 5-FU/LV) or docetaxel plus oxaliplatin combinations [61][62][63][64][65][66][67][68][62,63,64,65,66,67,68,69]. According to a recent meta-analysis, irinotecan-based regimes (NALIRI and FOLFIRI) may be the preferred options for second-line treatment with regard to survival outcomes, as shown in Figure 2 and Figure 3 [69][70].