Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Megumi Watanabe and Version 2 by Lindsay Dong.
Cases of probable titanium allergy included those with true titanium allergies and those with a potentially different cause. However, the differentiation of these cases is difficult. Since no definitive method has been established for diagnosing titanium allergy, a comprehensive diagnosis based on the clinical course and clinical examination using a patch test/lymphocyte transformation test (LTT)/memory lymphocyte immunostimulation assay (/MELISA) is necessary. Implant treatment should be performed with caution in patients with any preoperative allergies.
- titanium allergy
- implant failure
- dentistry
1. Introduction
Dental metal allergy is one of the problems caused by the use of metals in dentistry. While mercury and nickel are well-known antigenic metals that can trigger allergic reactions, hypersensitivity reactions to titanium have recently been reported, especially in the field of orthopedics [1][2][3][4][1,2,3,4]. Because titanium shows excellent biocompatibility and is thought to not cause immune reactions in the host, titanium dental implants have been used as a safe and predictable treatment option for more than 50 years [5]. Their safety can be attributed to the high biocompatibility of titanium, since titanium implants continue to exist safely in the patient’s bone in harmony with a healthy organism and excellent biomaterials [6].
Although unlike dynamically moving joints, implants placed in the jawbone are considered to be in a relatively immobile state, so that the risk of titanium powder adhering to bone or soft tissue over time is considered to be lower compared to artificial joints, hypersensitivity reactions potentially caused by dental implants have also been reported. The causes of implant failure include bone tissue damage due to poor surgical techniques, bacterial infections, host factors such as poor healing and poor bone quality, poor prosthesis design, and excessive or traumatic occlusal loading on the implants [7], and these failures cannot be attributed to the use of titanium itself. However, unexplained implant failures may occur despite the absence of these issues, and rejection reactions or allergic responses to the implant may be a potential cause.
2. The Link between Implant Failures and Titanium Allergy
2.1. Mechanism of Dental Metal Allergy Development
Metal allergy is a delayed type of hypersensitive reaction and is classified as type IV in the allergy classification proposed by Coombs and Gell [8][23]. Delayed-type hypersensitivity reactions are those in which symptoms are observed within 24 to 48 h after contact with the antigen, due to the involvement of cellular immune responses by T lymphocytes.
In many cases, dental metal allergy occurs when metal restorations are placed in the oral cavity after metal in jewelry or cosmetics has been taken in through the skin and the patient becomes sensitized. Titanium is a material with high biocompatibility, has been used for dental implants for more than half a century [9][24], and is widely known to have shown very good clinical results. However, in recent years, there have been reports of cases of allergy to titanium. This may be due to the increased exposure to titanium. Titanium is included in cosmetics such as sunscreen and foundation, and is also used in pierced earrings as a safe alternative to nickel and other metals [10][11][12][25,26,27]. In other words, the opportunities to come into contact with titanium have been increasing in recent years, and it is not surprising that the body has become sensitized to titanium as it has been to other metals that have been allergens in the past [13][28].
The pathogenesis of metal allergy is established through a sensitization phase and an elicitation phase (Figure 12). The allergic reaction begins when a small hapten of 1 kDa or less adheres to the skin or mucous membranes, and it is not clear whether this hapten is a metal ion, a protein denatured by the metal, or something else. Clinically, however, it is thought that the dissolution (ionization) of metals by perspiration is important for the process of skin passage [14][29].
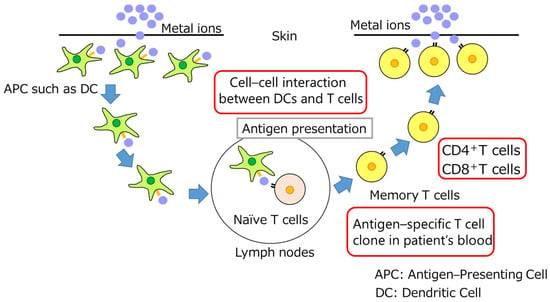 Several hours after adhering to the skin or mucous membranes, haptens pass through the keratinocyte layer of the epidermis and infiltrate into the subepithelium [15][16][30,31]. At this time, keratinocytes produce IL-1β, TNF-α, prostaglandin E2, etc., in response to haptens and activate antigen-presenting cells such as dendritic cells. Antigen-presenting cells that capture haptens migrate to local lymph nodes and present antigens to T cells via the major histocompatibility complex; the MHC and T-cell receptors thereby induce antigen-specific CD4-positive T cells and CD8-positive T cells. T cells that have memorized the antigen become memory T cells and prepare for the next antigen invasion. This is called sensitization, which usually takes one to two weeks. When the same hapten invades a sensitized individual again, keratinocytes produce cytokines that activate antigen-presenting cells, which in turn present antigens to T cells. In addition, existing memory T cells, i.e., antigen-specific T cells, respond rapidly to the hapten, triggering an inflammatory response. The elicitation phase lasts from 48 to 72 h. Thus, the interaction between keratinocytes, antigen-presenting cells, and T cells plays an important role in the development of metal allergy [17][32].
One of the factors that contribute to titanium’s excellent biocompatibility is that it is a very stable metal. Titanium is thought to have a passive oxide film on its surface that makes it difficult to ionize and pass through the skin [18][33]; however, the dynamics of titanium when skin is in direct contact with the titanium surface for a long period of time, such as with pierced skin, is unknown. It is not clear whether titanium is really stable in the harsh environment of the oral cavity. In the oral environment, titanium is constantly exposed to liquid components and proteins in saliva and food under body temperature; it is also exposed to H2S, an acid favored by bacteria; it is easily ionized by galvanic current generation due to coexistence with other types of metals; it is always in a crevice corrosion environment in the narrow gap between adjacent teeth; and it is subject to metal. The chloride ions in the tissue fluid exuding from the gingival sulcus and gingival pockets and in foodstuffs may destroy the passive oxide film. In addition, titanium particles are also taken into the body at the time of implantation, since dental implants are placed into bone through the mucosa. In other words, the increase in clinical reports of titanium allergy cases in recent years can be attributed to the increasing opportunities to become sensitized to titanium in daily life and the widespread use of titanium in dental treatment, as represented by dental implants, regardless of whether the reaction is truly allergic or not.
Several hours after adhering to the skin or mucous membranes, haptens pass through the keratinocyte layer of the epidermis and infiltrate into the subepithelium [15][16][30,31]. At this time, keratinocytes produce IL-1β, TNF-α, prostaglandin E2, etc., in response to haptens and activate antigen-presenting cells such as dendritic cells. Antigen-presenting cells that capture haptens migrate to local lymph nodes and present antigens to T cells via the major histocompatibility complex; the MHC and T-cell receptors thereby induce antigen-specific CD4-positive T cells and CD8-positive T cells. T cells that have memorized the antigen become memory T cells and prepare for the next antigen invasion. This is called sensitization, which usually takes one to two weeks. When the same hapten invades a sensitized individual again, keratinocytes produce cytokines that activate antigen-presenting cells, which in turn present antigens to T cells. In addition, existing memory T cells, i.e., antigen-specific T cells, respond rapidly to the hapten, triggering an inflammatory response. The elicitation phase lasts from 48 to 72 h. Thus, the interaction between keratinocytes, antigen-presenting cells, and T cells plays an important role in the development of metal allergy [17][32].
One of the factors that contribute to titanium’s excellent biocompatibility is that it is a very stable metal. Titanium is thought to have a passive oxide film on its surface that makes it difficult to ionize and pass through the skin [18][33]; however, the dynamics of titanium when skin is in direct contact with the titanium surface for a long period of time, such as with pierced skin, is unknown. It is not clear whether titanium is really stable in the harsh environment of the oral cavity. In the oral environment, titanium is constantly exposed to liquid components and proteins in saliva and food under body temperature; it is also exposed to H2S, an acid favored by bacteria; it is easily ionized by galvanic current generation due to coexistence with other types of metals; it is always in a crevice corrosion environment in the narrow gap between adjacent teeth; and it is subject to metal. The chloride ions in the tissue fluid exuding from the gingival sulcus and gingival pockets and in foodstuffs may destroy the passive oxide film. In addition, titanium particles are also taken into the body at the time of implantation, since dental implants are placed into bone through the mucosa. In other words, the increase in clinical reports of titanium allergy cases in recent years can be attributed to the increasing opportunities to become sensitized to titanium in daily life and the widespread use of titanium in dental treatment, as represented by dental implants, regardless of whether the reaction is truly allergic or not.
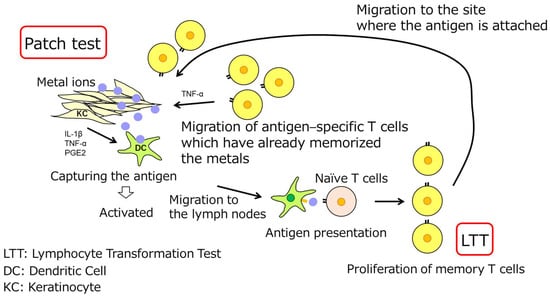
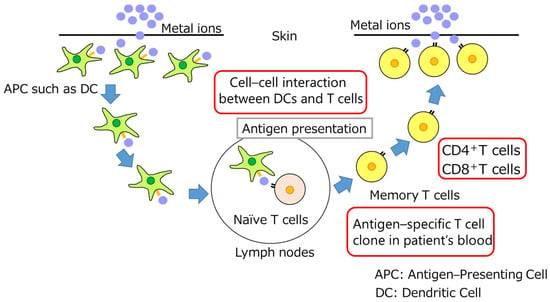
Figure 12. Possible mechanism of sensitization and elicitation. T cells: T cells are a type of lymphocyte that is involved in cellular immunity related to metal allergy. APC:-Antigen presenting cells. DC: Dendritic cells are the most professional potent antigen-presenting cells.
2.2. Clinical Symptoms of Titanium Allergy
Erythema, dermatitis, and local swelling were identified as the clinical manifestations of probable titanium allergy. Itching, burning, and pain have also been reported in some cases. Nevertheless, since hypersensitivity reactions to titanium have been reported in patients with postoperative complaints [19][34], a more reliable method for the diagnosis of titanium allergy is required to rule out other non-allergic factors as the causes of clinical symptoms. Although titanium must be proven to be the allergen to exclude other non-allergic factors as the cause of clinical symptoms, there is no established method to reliably diagnose titanium allergy. Currently, the diagnosis of suspected hypersensitivity reactions to titanium is based on an assessment of the clinical course, symptoms, application of conventional metal allergy tests, and the effect of treatments such as implant removal.2.3. Immunological Mechanisms of Metal-Allergy-Testing Methodologies
Metal allergy is a cellular immune reaction centered on T cells, and an immune response is triggered when metal sensitized on the skin is contained in a restoration or cement placed in the oral cavity. The patch test reproduces this in vivo (Figure 23). When a metal reagent is applied to a patient’s back skin, memory T cells, that have already been sensitized to the metal and have stored the antigen in the patient’s body, gather around the metal and produce inflammation such as redness and swelling by cytokine production on the skin, which is judged as positive. On the other hand, if there are no memory T cells for the metal in the body, no inflammation occurs, and the test is negative. Although the patch test is the most reliable examination method currently available, false-positive and false-negative results are possible, and the interpretation of the results is often difficult, so thorough knowledge is required. There is also a risk of new sensitization by the application of metallic reagents. Furthermore, there is a risk of temporary allergic flare-ups due to the application of the metal to the skin [20][35].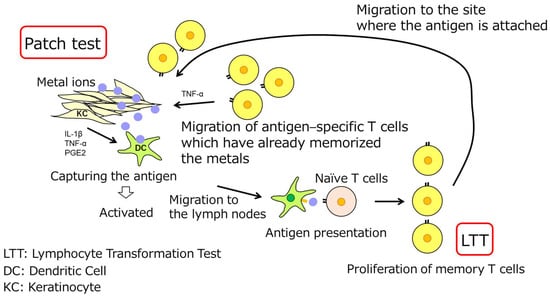
Figure 23.
Immunological mechanisms of patch test and LTT.
LTT is a method of testing a patient’s peripheral blood to detect memory T cells that react specifically to a certain metal to find metal-positive allergic reagents (Figure 23). The conventional LTT has low sensitivity and specificity, and is prone to false positives, making it inadequate for routine use compared to the patch test. However, LTT is an in vitro method using the patient’s blood, and if only a blood sample is taken, it is less physically demanding on the patient than the patch test, and there is no risk of new sensitization or allergic flare-ups due to metals. More research is required to improve and practicalize this approach by enhancing its sensitivity and specificity [21][36].
2.4. Diagnostic Techniques Used in Titanium Allergy Detection and Their Limitations
The patients in four and three articles were diagnosed using patch tests and LTT/MELISA, respectively. Patch tests and blood-based LTT/MELISA are currently used for the definitive clinical diagnosis of metal allergies [22][23][37,38]; however, both are known to yield false-positive and false-negative results in evaluations using titanium as the antigen, and are not completely reliable testing methods [19][24][25][26][27][28][29][9,11,14,34,39,40,41]. A systematic review examining the effectiveness of patch testing and LTT/MELISA in patients with suspected Ti hypersensitivity reported inconsistent results in terms of reliability and validity [30][42]. In addition, Ti allergy is historically new [31][32][33][34][43,44,45,46], and there are no uniform standards for the reagents and protocols used in the tests.
The use of Ti as an antigen for testing requires a solvent, and different solvents have been reported to produce different immunoreactions [19][34]. In a retrospective study, the commonly used agent TiO2 was reported to be likely to produce false-negative test results regardless of concentration, and titanium (IV) oxalate hydrate (TiC4O9H2-xH2O) was shown to drop to pH 2.0–3.0 when exposed to air and cause irritation, resulting in unstable test results [35][47]. In some studies, both TiCl4 and TiO2 were used; however, in Hosoki’s paper, the same patient did not react to TiO2 but showed positive results with TiCl4 in a patch test performed simultaneously [26][14].
