Mediastinal masses present a diagnostic challenge due to their diverse etiologies. Accurate localization and internal characteristics of the mass are the two most important factors to narrow the differential diagnosis or provide a specific diagnosis. The International Thymic Malignancy Interest Group (ITMIG) classification is the standard classification system used to localize mediastinal masses. Computed tomography (CT) and magnetic resonance imaging (MRI) are the two most commonly used imaging modalities for characterization of the mediastinal masses.
1. Introduction
The mediastinum is a complex anatomical space between the lungs bounded superiorly by the thoracic inlet, inferiorly by the diaphragm, anteriorly by the sternum and posteriorly by the spine. The mediastinum contains vital structures that can be affected by a wide range of pathologies including neoplasm (benign and malignant), congenital and vascular abnormalities, glandular hyperplasia and lymphadenopathy. Accurate localization of the mass to a mediastinal compartment is the first and crucial step to creating a useful differential diagnosis. The mediastinal compartment classification system advocated by the International Thymic Malignancy Interest Group (ITMIG) in 2014 is the standard classification system used to localize mediastinal masses. This classification system divides mediastinum into three compartments: prevascular (anterior), visceral (middle) and paravertebral (posterior) compartments using anatomical landmarks on CT (
Figure 1)
[1][2][3][4][5][1,2,3,4,5].
Figure 1. ITMIG definition of mediastinal compartments. Sagittal reformatted CT with color overlay shows mediastinal compartment borders: prevascular compartment (orange), visceral compartment (green) and paravertebral compartment (purple).
Imaging plays an important role in the evaluation, diagnosis, staging and treatment planning of mediastinal pathologies. Mediastinal masses are commonly discovered incidentally upon chest radiography. Occasionally, mediastinal masses may be discovered upon echocardiography performed in patients with nonspecific chest pain. Echocardiography is also helpful in evaluating hemodynamic complications of intracardiac extension of mediastinal masses
[6][7][6,7]. Cross-sectional imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) are used to evaluate the internal characteristics of the mass. It should be accurately determined if the mass is solid or cystic and assessed for the presence of fat or calcification. Post-contrast images are used to determine vascularity of the mass. This approach helps the radiologists to narrow the differential or make a specific diagnosis.
2. Imaging Modalities
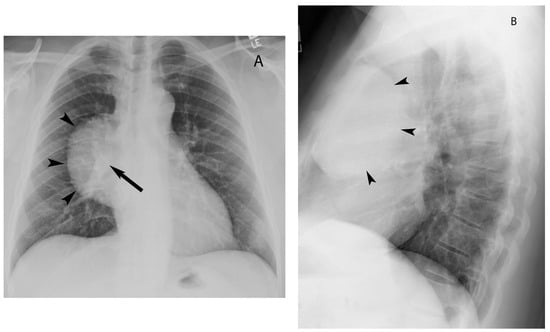
Chest radiography is often the first imaging modality to demonstrate mediastinal mass. Two view chest radiographs (PA and lateral) are particularly helpful for localizing the abnormality to a mediastinal compartment. The hilum overlay sign on frontal chest radiography helps in determining if an opacity in the region of the hilum is located within the hilum versus anterior or posterior to it. If the hilar vessels are seen through the mass, it indicates the mass does not originate in the hilum and is located either anteriorly or posteriorly to it
[8] (
Figure 2).
Figure 2. Hilum overlay sign. Chest radiograph posteroanterior view (
A) shows well-marginated mass over right hilum (arrowheads). Hilar vessels (arrow) are seen through the mass, suggesting the mass is either anterior or posterior to the hilum. Chest radiograph lateral view (
B) confirms the anterior location of the mass (arrowheads).
3. Cystic Lesions
Well-defined homogeneous fluid-attenuating (0 to 20 HU) lesions in the prevascular mediastinum are of benign etiology including thymic and pericardial cysts
[9][10][19,20]. These can be distinguished from one another based on their locations—thymic cysts are present in the thymic bed (
Figure 3) and pericardial cysts are commonly located at the right cardiophrenic angle (
Figure 4). Sometimes, thymic cysts may demonstrate attenuation values higher than simple fluid. In such cases, MRI is useful due to its ability to distinguish cystic lesions from solid lesions. They are hyperintense on T2W images and do not enhance after administration of intravenous contrast material (
Figure 5)
[11][12][10,11]. Multilocular cystic lesions in the prevascular mediastinum may represent multilocular thymic cyst or lymphangioma. When multilocular cystic lesion with septations or soft tissue component extends to the neck, axilla or chest wall, the possibility of lymphangioma should be considered
[10][13][20,21]. The presence of soft tissue component in the cystic lesion raises the possibility of malignancy with differentials including cystic teratoma or cystic thymoma (
Figure 6). The soft tissue component may enhance with intravenous contrast administration
[14][15][16][22,23,24].
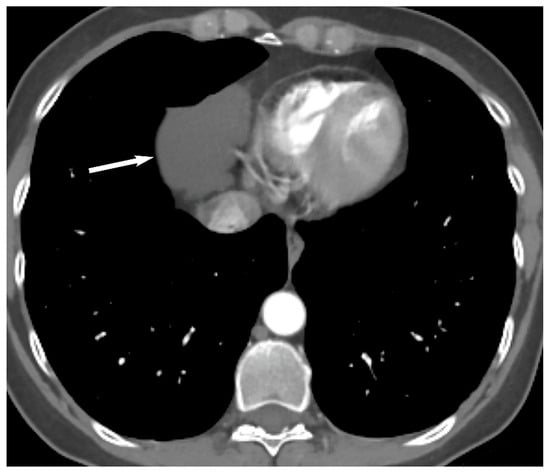
Figure 3. Thymic cyst. CT shows a fluid attenuating structure (15 Hounsfield units) in the prevascular mediastinum in the region of thymic bed (arrow).
Figure 4. Pericardial cyst. CT shows a fluid attenuating structure (10 Hounsfield units) in the prevascular mediastinum at the right anterior cardiophrenic angle (arrow).
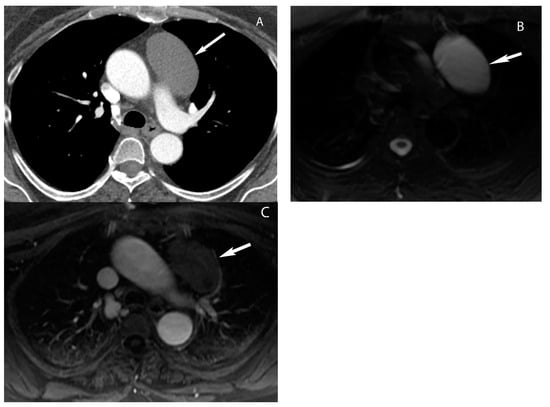
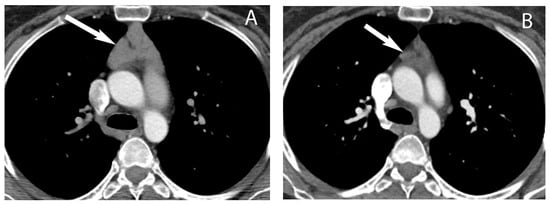
Figure 5. Thymic cyst. (
A) CT shows a well-defined homogeneous structure with density slightly higher than simple fluid (40 Hounsfield units) in the prevascular mediastinum (arrow). MRI (
B,
C) shows T2 hyperintensity (arrow in (
B)) and no enhancement with gadolinium (arrow in (
C)) consistent with fluid.
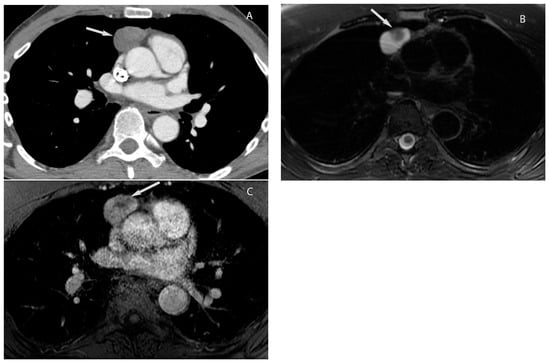
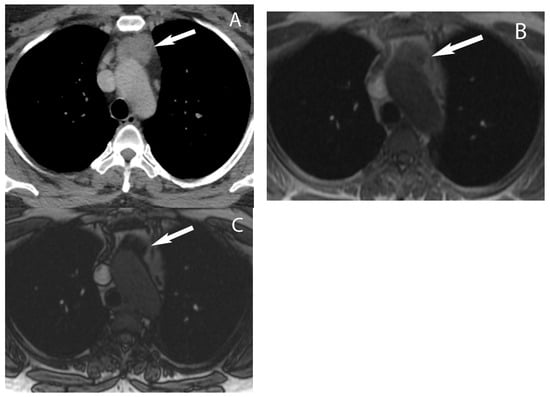
Figure 6. Cystic thymoma. CT (
A) shows a mixed attenuation (cystic and solid) mass in the prevascular mediastinum. T2W MRI (
B) shows hyperintense cystic component and hypointense solid nodule (arrow in (
B)). Post-gadolinium MRI (
C) shows enhancement of the solid nodule. Pathology showed cystic thymoma.
4. Thymic Hyperplasia
Thymus is a lymphatic organ situated in the prevascular mediastinum. It is relatively large during infancy but gradually decreases in size and is replaced by fat as a normal aging process. Rebound thymic hyperplasia can occur at any age due to physiological stress such as surgery, radiation therapy, chemotherapy, burns or steroid use. Thymic hyperplasia can manifest as diffuse symmetric enlargement of the gland maintaining its triangular bilobed shaped or a discrete mass. Thymic hyperplasia is easy to diagnose upon CT when it manifests as diffuse enlargement of the gland (
Figure 7).
Figure 7. Thymic hyperplasia. CT (
A) shows diffuse enlargement of the thymus maintaining its triangular or bilobed shape (arrow). Follow-up CT (
B) 12 months later shows fatty involution of the thymus (arrow).
However, when thymic hyperplasia manifests as a discrete mass, it can be a diagnostic challenge to distinguish thymic hyperplasia from thymic neoplasm upon CT. If the clinical suspicion for thymic hyperplasia is high, follow-up CT in 2–3 months can be obtained to demonstrate expected decrease in the size of the gland. Alternatively, MRI with chemical shift imaging may be helpful in distinguishing thymic hyperplasia from true thymic neoplasm. Thymic hyperplasia shows homogeneous decrease in signal intensity on opposed-phase sequence relative to in-phase sequence due to the presence of fat in contrast to thymic neoplasms that do not show any signal drop
[17][18][19][20][12,18,26,27] (
Figure 8).
Figure 8. Thymic hyperplasia. CT (
A) shows a rounded soft tissue mass in the prevascular mediastinum (arrow) in a woman with breast cancer. Differential diagnosis includes thymic epithelial neoplasm or metastatic disease. MRI chest in-phase image (
B) shows the mass is isointense to muscle (arrow) and shows drop in signal on opposed-phase image (
C) consistent with thymic hyperplasia.
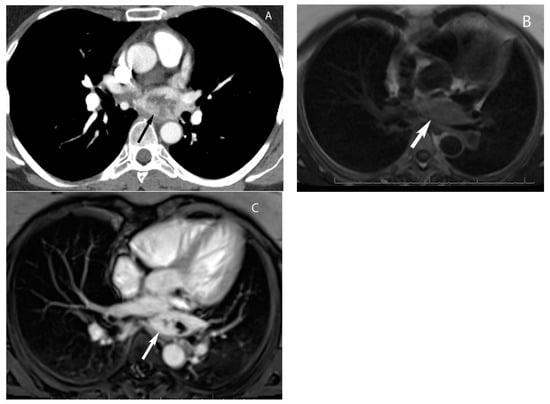
5. Thymic Epithelial Neoplasms
Upon CT, noninvasive thymoma appears as a homogeneous or mildly heterogeneous soft tissue mass with well-circumscribed borders (
Figure 9). When a soft tissue mass has irregular or lobular borders, or heterogeneity due to necrosis or cystic changes and intrinsic calcification, invasive thymoma should be suspected
[21][22][29,30]. Intravenous contrast is useful to assess for local invasion and CT may show infiltration of the mediastinal fat, encasement or frank invasion of vascular structures, invasion of the pleura or pericardium. Pleural implants (drop metastases) may be present with invasive tumors and are highly suspicious for thymoma (
Figure 10).
Figure 9.
Thymoma. CT shows a well-defined homogeneous soft tissue mass in the prevascular mediastinum (arrow).
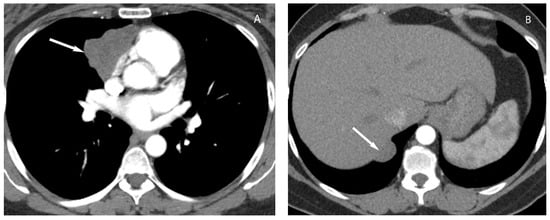
Figure 10. Thymoma with pleural drop metastasis. CT (
A,
B) shows a lobulated soft tissue mass in the prevascular mediastinum (arrow in (
A)) and a diaphragmatic pleural nodule in the right lower chest (arrow in (
B)).
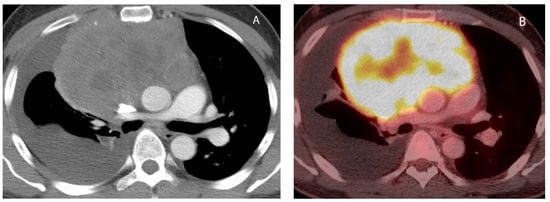
6. Lymphoma
Upon imaging, primary mediastinal lymphoma may present as a lobulated homogeneous soft tissue mass or may show areas of low attenuation due to necrosis/cystic degeneration
[8][23][24][25][8,15,38,39] (
Figure 112). It might be difficult to distinguish lymphoma from other mediastinal soft tissue masses upon imaging, and biopsy is required to confirm the diagnosis. Vascular encasement or displacement without invasion is characteristic of lymphoma. When such imaging findings are seen in young patients along with B symptoms (fever, weight loss and night sweat), a diagnosis of mediastinal lymphoma should be considered. When enlarged lymph nodes are seen involving multiple mediastinal lymph node stations in the setting of extrathoracic lymphadenopathy, secondary involvement of systemic lymphoma should be considered
[2][23][2,15]. F18-fluorodeoxyglucose-positron emission tomography/computed tomography (FDG-PET/CT) is the modality of choice for the initial staging and ongoing surveillance of lymphoma during treatment. It may be helpful in identifying occult lesions in the spleen, bones and gastrointestinal tract. FDG-PET/CT is also used to guide tissue sampling by identifying the most FDG avid lesions and avoiding necrotic or uninvolved tissues
[26][27][28][13,14,40].
Figure 112. Primary mediastinal lymphoma. CT (
A) shows large heterogeneous soft tissue mass in the prevascular mediastinum. The mass is hypermetabolic on FDG PET-CT (
B). Biopsy showed diffuse large B cell lymphoma.
7. Germ Cell Tumors
Upon CT, teratomas usually present as a well-defined heterogeneous mass with variable amounts of fat and soft tissue and may contain calcification (Figure 123). Rarely, bone or tooth can be identified within the mass. They may be predominantly cystic (unilocular or multilocular) and the presence of a fat fluid level within the mass is highly suggestive of mature teratoma but less commonly seen [4][18][29][4,18,46].
Figure 123. Mature teratoma. CT axial (
A) and coronal reformat (
B) show a well-defined mass containing soft tissue, fat (arrow in (
A)) and calcification (arrow in (
B)) in the prevascular mediastinum compatible with mature teratoma.
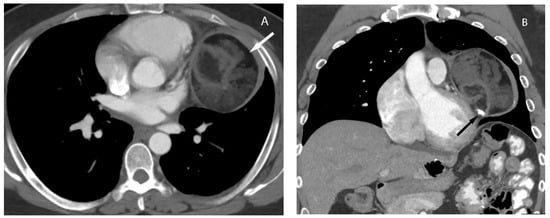
8. Cystic Lesions
The most common cystic lesions in the visceral compartment include bronchogenic and esophageal duplication cysts. Bronchogenic cyst commonly occurs near the carina or less frequently in the right paratracheal region. Upon CT, it typically manifests as well-circumscribed, homogeneous lesions with fluid attenuation (0 to 20 HU). The cyst wall may show enhancement with contrast administration or contain calcification. Internal heterogeneity can occur in some cases due to hemorrhagic or proteinaceous contents or infection of the bronchogenic cyst. MRI is helpful in such cases to confirm the cystic nature of these legions. MRI shows high signal intensity on T2-weighted images and variable signal intensity on T1-weighted images depending upon the hemorrhagic or proteinaceous contents of the cystic lesion. Typically, these lesions do not enhance but sometimes enhancement of the wall may be seen after gadolinium administration (Figure 135) [11][12][30][10,11,50].
Figure 135. Foregut duplication cyst. CT (
A) shows a well-marginated structure in the visceral mediastinum with attenuation values slightly higher than simple fluid. MRI (
B,
C) show high signal intensity upon T2W imaging (arrow in (
B)) and no enhancement upon post-gadolinium imaging (arrow in (
C)) consistent with fluid.
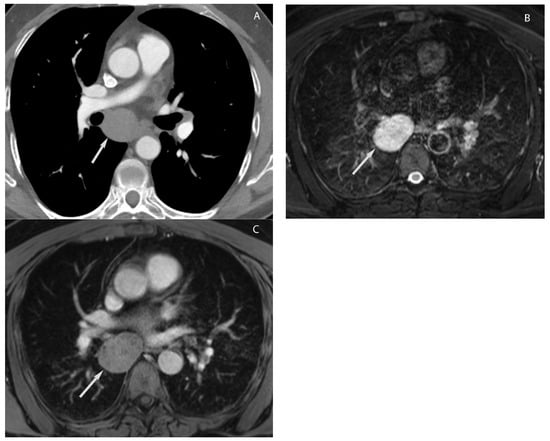
9. Hypervascular Lesions
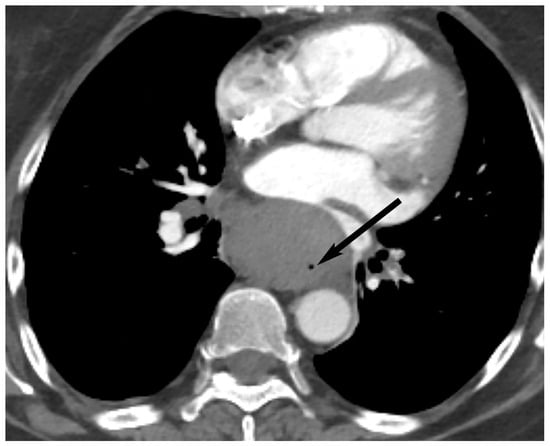
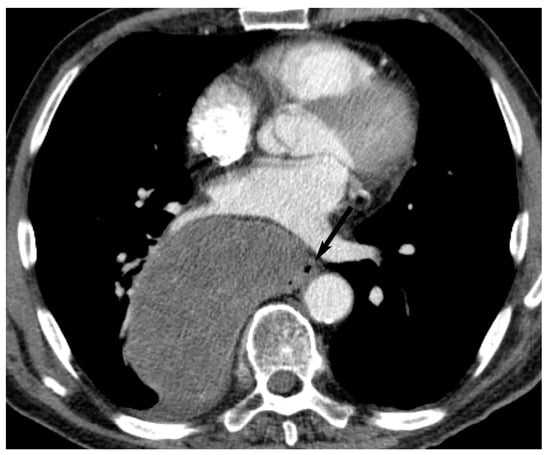
Paragangliomas are rare neuroendocrine tumors that arise from chromaffin cells located outside of the adrenal gland. They can occur anywhere along the sympathetic chain or parasympathetic ganglia. These are highly vascular neoplasms that rarely occur in the visceral mediastinum, most commonly affecting the left atrium. These lesions typically manifest as homogeneously and intensely enhancing masses upon CT. Sometimes, internal heterogeneity may be present due to tumor necrosis. Upon MRI, these tumors show high signal density in T2-weighted images and may have intermediate signal intensity in T1-weighted images (
Figure 146)
[29][31][32][33][46,48,51,52].
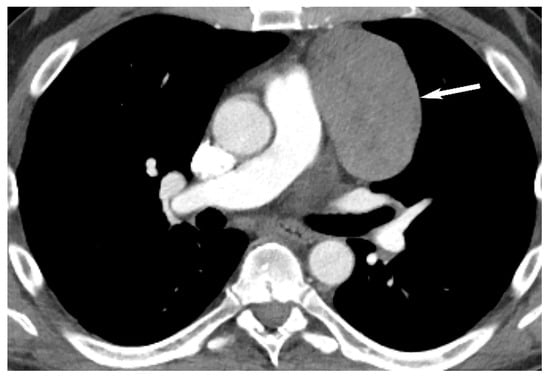
Figure 146. Paraganglioma. CT (
A) shows a hypervascular mass with central necrosis in the visceral mediastinum behind the left atrium. MRI (
B,
C) shows the mass is hyperintense compared to muscle upon black blood double inversion MRI (arrow in (
B)) and hypervascular upon post-gadolinium imaging (arrow in (
C)).
10. Esophageal Lesions
Both esophageal carcinoma and esophageal gastrointestinal stromal tumor (GIST) can present as esophageal masses and are challenging to differentiate upon imaging. Esophageal GISTs are relatively rare and more commonly found in the stomach or small intestine. Esophageal carcinomas often present as irregular or infiltrative masses that can invade the adjacent structures (
Figure 158). GISTs, on the other hand, tend to have a well-defined or lobulated shape and smooth margins. GISTs are mesenchymal tumors that usually arise in the submucosal layer of the esophageal wall. Therefore, they may show an extraluminal growth pattern that can cause luminal narrowing or displacement (
Figure 169). In contrast, esophageal carcinomas arise from the mucosal layer and tend to infiltrate the wall, resulting in concentric growth and wall thickening. Upon contrast-enhanced images, esophageal carcinomas typically show heterogeneous enhancement whereas GISTs may show a homogeneous enhancement pattern. It is important to note that histopathological evaluation is necessary for accurate diagnosis
[34][35][58,59].
Figure 158. Esophageal carcinoma. CT shows a soft tissue mass in the visceral mediastinum inseparable from the esophagus (arrow). Biopsy showed esophageal carcinoma.
Figure 169. Esophageal gastrointestinal stromal tumor (GIST). CT shows a large heterogeneous mass in the visceral mediastinum inseparable from the esophagus (arrow). Biopsy showed gastrointestinal stromal tumor